Clinical Diabetes/Therapeutics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chapter 7: Monogenic Forms of Diabetes
CHAPTER 7 MONOGENIC FORMS OF DIABETES Mark A. Sperling, MD, and Abhimanyu Garg, MD Dr. Mark A. Sperling is Emeritus Professor and Chair, University of Pittsburgh, Department of Pediatrics, Children’s Hospital of Pittsburgh of UPMC, Pittsburgh, PA. Dr. Abhimanyu Garg is Professor of Internal Medicine and Chief of the Division of Nutrition and Metabolic Diseases at University of Texas Southwestern Medical Center, Dallas, TX. SUMMARY Types 1 and 2 diabetes have multiple and complex genetic influences that interact with environmental triggers, such as viral infections or nutritional excesses, to result in their respective phenotypes: young, lean, and insulin-dependence for type 1 diabetes patients or older, overweight, and often manageable by lifestyle interventions and oral medications for type 2 diabetes patients. A small subset of patients, comprising ~2%–3% of all those diagnosed with diabetes, may have characteristics of either type 1 or type 2 diabetes but have single gene defects that interfere with insulin production, secretion, or action, resulting in clinical diabetes. These types of diabetes are known as MODY, originally defined as maturity-onset diabetes of youth, and severe early-onset forms, such as neonatal diabetes mellitus (NDM). Defects in genes involved in adipocyte development, differentiation, and death pathways cause lipodystrophy syndromes, which are also associated with insulin resistance and diabetes. Although these syndromes are considered rare, more awareness of these disorders and increased availability of genetic testing in clinical and research laboratories, as well as growing use of next generation, whole genome, or exome sequencing for clinically challenging phenotypes, are resulting in increased recognition. A correct diagnosis of MODY, NDM, or lipodystrophy syndromes has profound implications for treatment, genetic counseling, and prognosis. -

Myalept® (Metreleptin)
UnitedHealthcare Pharmacy Clinical Pharmacy Programs Program Number 2021 P 2032-11 Program Prior Authorization/Medical Necessity Medication Myalept® (metreleptin) P&T Approval Date 5/2014, 7/2014, 8/2014, 7/2015, 6/2016, 5/2017, 5/2018, 5/2019, 5/2020, 5/2021 Effective Date 8/1/2021; Oxford only: 8/1/2021 1. Background: Myalept (metreleptin) is a leptin analog indicated as an adjunct to diet as replacement therapy to treat the complications of leptin deficiency in patients with congenital or acquired generalized lipodystrophy.1 Myalept is available only through a restricted distribution program under a Risk Evaluation and Mitigation Strategy (REMS), called the Myalept REMS program, because of the risks associated with the development of anti-metreleptin antibodies that neutralize endogenous leptin and the risk of lymphoma. 2. Coverage Criteria: A. Initial Authorization 1. Myalept will be approved based on all of the following criteria: a. Diagnosis of congenital or acquired generalized lipodystrophy associated with leptin deficiency -AND- b. Myalept is being used as an adjunct to diet modification -AND- c. Prescribed by an endocrinologist -AND- d. Documentation demonstrates that patient has at least one of the following: (1) Diabetes mellitus or insulin resistance with persistent hyperglycemia (HgbA1C > 7.0) despite both of the following: (a) Dietary intervention (b) Optimized insulin therapy at maximum tolerated doses © 2021 UnitedHealthcare Services, Inc. 1 -OR- (2) Persistent hypertriglyceridemia (TG > 250) despite both of the following: (a) Dietary intervention (b) Optimized therapy with at least two triglyceride-lowering agents from different classes (e.g., fibrates, statins) at maximum tolerated doses Authorization will be issued for 12 months B. -

Putting Medications in Perspective for Chronic Weight Management
05/06/2019 1 Donna H. Ryan, MD Professor Emerita Pennington Biomedical Research Center Baton Rouge, LA, USA The Role of Pharmacology in Weight Management: Putting Medications in Perspective for Chronic Weight Management 1 Disclosures • Consulting fee: Amgen, Gila Therapeutics, IFA Celtic, Novo Nordisk, Bausch Health, Real Appeal, Sanofi, Quintiles Novella, Paul Hastings, Simmons and Simmons, ReDesign Health, KVK Tech • Speakers bureau: Novo Nordisk, Bausch Health • Equity: Gila Therapeutics, Scientific Intake, Epitomee, ReDesign Health 2 05/06/2019 2 Objectives At the end of the session, attendees will be able to • identify when to start a weight loss medication, • identify how to choose the right one for the right patient, • identify when to combine approaches for better results and • discuss future prospects in obesity pharmacotherapy. • 3 Should we treat obesity with drugs? 4 05/06/2019 3 Should we treat obesity with drugs? No! not by themselves Yes! when patients need help • Drugs don’t work on their own. • For patients who struggle to lose They work through biology to enough weight to get health reinforce the patient’s intention to benefits, drugs can help them adhere to a dietary plan. Better better adhere to the dietary plan adherence = more weight loss. to lose more weight. Drugs also Drugs also sustain lost weight as sustain weight loss as long as they long as they are taken. are taken. 5 Rationale for Medications in Obesity Management • Food intake is biologically determined. • Weight loss is opposed and regain promoted by physiology of reduced obese state. • Medications work through biology of appetite regulation to help patients adhere to diet plans. -

Modifications to the Harmonized Tariff Schedule of the United States to Implement Changes to the Pharmaceutical Appendix
United States International Trade Commission Modifications to the Harmonized Tariff Schedule of the United States to Implement Changes to the Pharmaceutical Appendix USITC Publication 4208 December 2010 U.S. International Trade Commission COMMISSIONERS Deanna Tanner Okun, Chairman Irving A. Williamson, Vice Chairman Charlotte R. Lane Daniel R. Pearson Shara L. Aranoff Dean A. Pinkert Address all communications to Secretary to the Commission United States International Trade Commission Washington, DC 20436 U.S. International Trade Commission Washington, DC 20436 www.usitc.gov Modifications to the Harmonized Tariff Schedule of the United States to Implement Changes to the Pharmaceutical Appendix Publication 4208 December 2010 (This page is intentionally blank) Pursuant to the letter of request from the United States Trade Representative of December 15, 2010, set forth at the end of this publication, and pursuant to section 1207(a) of the Omnibus Trade and Competitiveness Act, the United States International Trade Commission is publishing the following modifications to the Harmonized Tariff Schedule of the United States (HTS) to implement changes to the Pharmaceutical Appendix, effective on January 1, 2011. Table 1 International Nonproprietary Name (INN) products proposed for addition to the Pharmaceutical Appendix to the Harmonized Tariff Schedule INN CAS Number Abagovomab 792921-10-9 Aclidinium Bromide 320345-99-1 Aderbasib 791828-58-5 Adipiplon 840486-93-3 Adoprazine 222551-17-9 Afimoxifene 68392-35-8 Aflibercept 862111-32-8 Agatolimod -

CDR Clinical Review Report for Soliqua
CADTH COMMON DRUG REVIEW Clinical Review Report Insulin glargine and lixisenatide injection (Soliqua) (Sanofi-Aventis) Indication: adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus inadequately controlled on basal insulin (less than 60 units daily) alone or in combination with metformin. Service Line: CADTH Common Drug Review Version: Final (with redactions) Publication Date: January 2019 Report Length: 118 Pages Disclaimer: The information in this document is intended to help Canadian health care decision-makers, health care professionals, health systems leaders, and policy-makers make well-informed decisions and thereby improve the quality of health care services. While patients and others may access this document, the document is made available for informational purposes only and no representations or warranties are made with respect to its fitness for any particular purpose. The information in this document should not be used as a substitute for professional medical advice or as a substitute for the application of clinical judgment in respect of the care of a particular patient or other professional judgment in any decision-making process. The Canadian Agency for Drugs and Technologies in Health (CADTH) does not endorse any information, drugs, therapies, treatments, products, processes, or services. While care has been taken to ensure that the information prepared by CADTH in this document is accurate, complete, and up-to-date as at the applicable date the material was first published by CADTH, CADTH does not make any guarantees to that effect. CADTH does not guarantee and is not responsible for the quality, currency, propriety, accuracy, or reasonableness of any statements, information, or conclusions contained in any third-party materials used in preparing this document. -
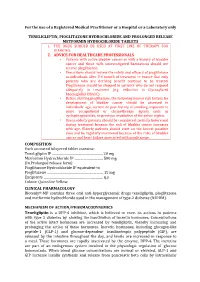
For the Use of a Registered Medical Practitioner Or a Hospital Or a Laboratory Only TENELIGLIPTIN, PIOGLITAZONE HYDROCHLORIDE AN
For the use of a Registered Medical Practitioner or a Hospital or a Laboratory only TENELIGLIPTIN, PIOGLITAZONE HYDROCHLORIDE AND PROLONGED RELEASE METFORMIN HYDROCHLORIDE TABLETS 1. THE DRUG SHOULD BE USED AT FIRST LINE OF THERAPY FOR DIABETES. 2. ADVICE FOR HEALTHCARE PROFESSIONALS • Patients with active bladder cancer or with a history of bladder cancer and those with uninvestigated haematuria should not receive pioglitazone. • Prescribers should review the safety and efficacy of pioglitazone in individuals after 3-6 month of treatment to ensure that only patients who are deriving benefit continue to be treated. Pioglitazone should be stopped in patients who do not respond adequately to treatment (e.g. reduction in Glycosylated haemoglobin HbA1C). • Before starting pioglitazone, the following known risk factors for development of bladder cancer should be assessed in individuals: age, current or past history of smoking, exposure to some occupational or chemotherapy agents such as cyclophosphamide, or previous irradiation of the pelvic region. • Use in elderly patients should be considered carefully before and during treatment because the risk of bladder cancer increases with age. Elderly patients should start on the lowest possible dose and be regularly monitored because of the risks of bladder cancer and heart failure associated with pioglitazone. COMPOSITION Each uncoated bilayered tablet contains: . 20 mg (InTeneligliptin Prolonged IP release .………………………..……………….. form) PioglitazoneMetformin Hydrochloride Hydrochloride IP IP …………………..…... equivalent to mg Pio . 15 mg .s Colour:glitazone Quinoline ………………………….…………………… Yellow Excipients ………………………….……………………..... q CLINICAL PHARMACOLOGY Biotenly®-MP contains three oral anti-hyperglycaemic drugs teneligliptin, pioglitazone and metformin hydrochloride used in the management of type-2 diabetes (NIDDM). MECHANISM OF ACTION/PHARMACODYNEMICS Teneligliptin is a DPP-4 inhibitor, which is believed to exert its actions in patients with type 2 diabetes by slowing the inactivation of incretin hormones. -

Amylin's $1 Billion Heavyweight Deal
news Amylin’s $1 billion heavyweight deal In November, Amylin announced a $1 billion partnership with Osaka, Japan–based Takeda to codevelop and commercialize obesity treatments. Takeda paid the San Diego–based biotech $75 million upfront for Symlin/metreleptin combination as part of an agreement that could exceed $1 billion if certain development and sales-dependent milestones are hit. The deal also includes Amylin’s amylinomimetic compound davalintide, which is currently only in phase 2 studies. But, as Stephen O’Rahilly, director of the Metabolic Research Laboratories at the University of Cambridge in the UK, points out, Symlin (pramlintide) is already approved and is “used by a lot of type I diabetes patients to smooth out control and prevent the weight gain that happens when on insulin.” The agreement comes amid a surge of deals in metabolic disease, particularly for diabetes treatments that have potential weight loss benefits for the obese. For example, on December 23, Amylin Paris-based Sanofi-Aventis paid €100 ($143) million for a 19.9% stake in Zealand Pharma. This Amylin has gained a strong position in the already crowded metabolic disease marketplace. Copenhagen-based biotech is developing a peptide analog of Amylin’s Byetta (glucagon-like peptide 1 (GLP-1)/exendin 4) for type 2 diabetes, which has also shown efficacy in promoting weight loss. In what has become a crowded market, products will likely gain a competitive edge if they can fight both metabolic disease and obesity, the latter with a potential market of 300 million people worldwide. Amylin already looks to have consolidated its position. -

Korelasi Kadar Asam Urat Dalam Darah Terhadap Luaran Klinis Stroke
Artikel Penelitian KORELASI KADAR ASAM URAT DALAM DARAH TERHADAP LUARAN KLINIS STROKE ISKEMIK AKUT THE CORRELATION BETWEEN URIC ACID SERUM LEVELS AND ACUTE STROKE ISCHEMIC OUTCOME Daniel Mahendrakrisna,* Aria Chandra Gunawan Triwibowo Soedomo** ABSTRACT Background: Uric acid is an end metabolism product of purine. It has been known as an important antioxidant in the serum. Correlation between uric acid serum with stroke has been reported controversial finding. However, Uric acid has been proposed to be a stroke risk factor. Aim: To determine the correlation between uric acid serum levels and acute stroke ischemic outcome. Method: This was a cross-sectional study at Surakarta Hospital. All of first experience stroke ischemic patients proven by CT-Scan were included as subjects. Demographic data (age, sex, blood pressure, etc) and laboratory results such as uric acid 24 hours, blood glucose test (random glucose test and fasting glucose test), lipid profile (cholesterol, triglyceride) were obtained from medical records. Data was analysed by software and p<0.05 was statistically accepted. Results: Of 49 acute stroke ischemic patients were include to this study. The mean of uric acid level serum as 5.71±2.64 mg/dL. 30,6% subjects had hyperuricemia and 8,2% subjects had hypouricemia. There were no correlation between uric acids levels with stroke clinical outcome (r= 0.08, p>0.05). Discussion: There was no correlation between uric acid serum levels and acute stroke ischemic outcome.. Keywords: Ischemic, Modified Rankin Scale, outcome, stroke, uric acid ABSTRAK Latar Belakang: Asam urat dalam darah merupakan produk akhir dari metabolism purin pada manusia dan merupakan diduga menjadi salah satu antioksidan yang penting didalam plasma. -

IJBCP International Journal of Basic & Clinical Pharmacology the Observational, Cross-Sectional Study of Drug Utilization
Print ISSN: 2319-2003 | Online ISSN: 2279-0780 IJBCP International Journal of Basic & Clinical Pharmacology DOI: http://dx.doi.org/10.18203/2319-2003.ijbcp20194771 Original Research Article The observational, cross-sectional study of drug utilization 90% and use of dipeptidyl peptidase-4 inhibitor in the patients with type 2 diabetes mellitus Prashant P. Shivgunde1*, Shantanu R. Joshi2, Archana D. Kodilkar1 1Department of University Research, Maharashtra ABSTRACT University of Health Sciences (MUHS), Mhasrul, Vani- Background: Diabetes is a chronic metabolic disease which affects the quality Dindori Road, Nashik, of life. It leads to multiple complications due to metabolic involvement. Out of Maharashtra, India multiple drugs used to treat diabetes, dipeptidyl peptidase 4 (DPP-4) inhibitors 2 Global Herbs Pharmaceuticals, are comparatively new drugs used for type-2-diabetes mellitus (DM) treatment. Pune-Satara Road, Pune, This study aimed to find out the drug utilization (DU) 90% and use of DPP-4 Maharashtra, India inhibitors in patients with type-2-DM. Methods: A prospective, cross-sectional, observational study was conducted at Received: 28 September 2019 a private healthcare clinic of an endocrinologist in Nashik. Type-2-DM patients Revised: 11 October 2019 of both sexes were selected and a total of 199 patients were enrolled in the Accepted: 14 October 2019 study. The consented patients were interviewed and prescription copies were collected. After studying them; statistical analysis was done and results and *Correspondence to: conclusions were drawn. Dr. Prashant P. Shivgunde, Results: Out of total prescribed drugs, 58.77% of drugs were anti-diabetics. It Email: prashantshivgunde@ was observed that the biguanides were most frequently (25.32%) prescribed gmail.com while the least prescribed drugs were meglitinide analogues (0.08%). -

September 2017 ~ Resource #330909
−This Clinical Resource gives subscribers additional insight related to the Recommendations published in− September 2017 ~ Resource #330909 Medications Stored in the Refrigerator (Information below comes from current U.S. and Canadian product labeling and is current as of date of publication) Proper medication storage is important to ensure medication shelf life until the manufacturer expiration date and to reduce waste. Many meds are recommended to be stored at controlled-room temperature. However, several meds require storage in the refrigerator or freezer to ensure stability. See our toolbox, Medication Storage: Maintaining the Cold Chain, for helpful storage tips and other resources. Though most meds requiring storage at temperatures colder than room temperature should be stored in the refrigerator, expect to see a few meds require storage in the freezer. Some examples of medications requiring frozen storage conditions include: anthrax immune globulin (Anthrasil [U.S. only]), carmustine wafer (Gliadel [U.S. only]), cholera (live) vaccine (Vaxchora), dinoprostone vaginal insert (Cervidil), dinoprostone vaginal suppository (Prostin E2 [U.S.]), varicella vaccine (Varivax [U.S.]; Varivax III [Canada] can be stored in the refrigerator or freezer), zoster vaccine (Zostavax [U.S.]; Zostavax II [Canada] can be stored in the refrigerator or freezer). Use the list below to help identify medications requiring refrigerator storage and become familiar with acceptable temperature excursions from recommended storage conditions. Abbreviations: RT = room temperature Abaloparatide (Tymlos [U.S.]) Aflibercept (Eylea) Amphotericin B (Abelcet, Fungizone) • Once open, may store at RT (68°F to 77°F • May store at RT (77°F [25°C]) for up to Anakinra (Kineret) [20°C to 25°C]) for up to 30 days. -

Nonobese, Nonketotic Childhood Onset Diabetes: Look for Lipodystrophies Partha P
CASE STUDIES Nonobese, Nonketotic Childhood Onset Diabetes: Look for Lipodystrophies Partha P. Chakraborty,1 Sayantan Ray,2 Subhodip Pramanik,2 Rana Bhattacharjee,2 Sujoy Ghosh,2 and Subhankar Chowdhury2 iabetes in children and youth agnosed as having type 2 diabetes (3). poses a unique diagnostic We describe here two patients with Dand therapeutic challenge. childhood-onset diabetes secondary Although type 1 and type 2 diabetes to congenital lipodystrophies and are undoubtedly the most frequently discuss their clinical and diagnostic encountered forms of diabetes, oth- features. er forms are not uncommon in this Case Presentations age-group. Many young patients with a so-called “specific types of diabetes Case 1 due to other causes” may be misdi- A 6-year-old girl born of a consan- agnosed as having type 1 or type 2 guineous union had been detected diabetes because of a lack of awareness to have diabetes while undergoing of the various diagnostic possibilities evaluation for failure to gain weight. (1). The group of patients with other She was placed on insulin by her pri- forms of diabetes constitutes <5% of mary care physician and referred to all patients diagnosed with diabetes us for unsatisfactory glycemic control before the age of 25 years and in- despite receiving a high dosage of in- cludes a variety of conditions (2). sulin (3.7 units/kg; total daily dose: Lipodystrophy, a group of disor- 52 units). She did not notice osmot- ders characterized by loss or abnormal ic symptoms and had no history of distribution of body fat, is associated hospitalization. Her birth weight was with insulin resistance and resul- 2.1 kg, and she had been unusually tant abnormal glucose homeostasis. -

Outpatient Education Referral Form
Outpatient Education Referral Form 805 Dixie Street – Carrollton, GA 30117 Telephone: 770.812.5954 Fax: 770.812.5776 We are pleased to provide same-day walk-in appointments at our location above. Please send your patient to our office to be seen today! Patient Name: _______________________________ Date of Birth: ____/____/_____ Patient Phone: ___________________________ Insurance: ______________________________ Diagnosis (including ICD-10 code) ________________________________________________________________________ *Special needs due to impairment of: □ vision □ hearing □ language □ reading □ other__________ Patients with special needs are eligible for 10 hours of individual 1 on 1 training (please check appropriate boxes for service) □ Pre-Diabetes/Metabolic Syndrome □ Diabetes Self-Management Education Current Diabetes Medication: □ Insulin regimen □ Oral agents □ Other injectables □ Gestational Diabetes: # weeks gestation: ____________ Estimated Delivery Date: _______________ □ Medical Nutrition Therapy (MNT) – with Registered Dietitian □ Living Well with Chronic Disease □ Tobacco Cessation □ Get Healthy Kids The following are MEDICARE criteria for DIABETES only services -must have occurred within the last 12 months; must have documentation of the labs before accepting the referral. Fasting blood sugar greater than or equal to 126 mg/dl on two different occasions (or) Two hour post-glucose challenge greater than or equal to 200 mg/dl on two different occasions (or) Random glucose test over 200 mg/dl for a person with symptoms of uncontrolled diabetes Change in Medical Condition, diagnosis or treatment i.e., chronic renal insufficiency and diabetes Please fax this referral, along with relevant labs (blood glucose, A1c, lipids, creatinine, basic metabolic panel, or relevant physician notes) to 770.812.5776. The American Diabetes Association Recognized Diabetes Patient Education Program / Medical Nutrition Therapy is integral to the care of my patient.