Pregnancy, Abortion, and Ectopic Pregnancy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
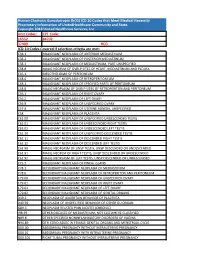
Human Chorionic Gonadotropin (Hcg) ICD 10 Codes That Meet Medical Necessity Proprietary Information of Unitedhealthcare Community and State
Human Chorionic Gonadotropin (hCG) ICD 10 Codes that Meet Medical Necessity Proprietary Information of UnitedHealthcare Community and State. Copyright 2018 United Healthcare Services, Inc Unit Codes: CPT Code: 16552 84702 37409 HCG ICD-10 Codes Covered if selection criteria are met: C38.1 MALIGNANT NEOPLASM OF ANTERIOR MEDIASTINUM C38.2 MALIGNANT NEOPLASM OF POSTERIOR MEDIASTINUM C38.3 MALIGNANT NEOPLASM OF MEDIASTINUM, PART UNSPECIFIED C38.8 MALIG NEOPLM OF OVRLP SITES OF HEART, MEDIASTINUM AND PLEURA C45.1 MESOTHELIOMA OF PERITONEUM C48.0 MALIGNANT NEOPLASM OF RETROPERITONEUM C48.1 MALIGNANT NEOPLASM OF SPECIFIED PARTS OF PERITONEUM C48.8 MALIG NEOPLASM OF OVRLP SITES OF RETROPERITON AND PERITONEUM C56.1 MALIGNANT NEOPLASM OF RIGHT OVARY C56.2 MALIGNANT NEOPLASM OF LEFT OVARY C56.9 MALIGNANT NEOPLASM OF UNSPECIFIED OVARY C57.4 MALIGNANT NEOPLASM OF UTERINE ADNEXA, UNSPECIFIED C58 MALIGNANT NEOPLASM OF PLACENTA C62.00 MALIGNANT NEOPLASM OF UNSPECIFIED UNDESCENDED TESTIS C62.01 MALIGNANT NEOPLASM OF UNDESCENDED RIGHT TESTIS C62.02 MALIGNANT NEOPLASM OF UNDESCENDED LEFT TESTIS C62.10 MALIGNANT NEOPLASM OF UNSPECIFIED DESCENDED TESTIS C62.11 MALIGNANT NEOPLASM OF DESCENDED RIGHT TESTIS C62.12 MALIGNANT NEOPLASM OF DESCENDED LEFT TESTIS C62.90 MALIG NEOPLASM OF UNSP TESTIS, UNSP DESCENDED OR UNDESCENDED C62.91 MALIG NEOPLM OF RIGHT TESTIS, UNSP DESCENDED OR UNDESCENDED C62.92 MALIG NEOPLASM OF LEFT TESTIS, UNSP DESCENDED OR UNDESCENDED C75.3 MALIGNANT NEOPLASM OF PINEAL GLAND C78.1 SECONDARY MALIGNANT NEOPLASM OF MEDIASTINUM C78.6 SECONDARY -

Placental Site Nodule (PSN): an Uncommon Diagnosis with a Common Presentation
ISSN: 2377-9004 Sneha and Ramesh Kumar. Obstet Gynecol Cases Rev 2021, 8:199 DOI: 10.23937/2377-9004/1410199 Volume 8 | Issue 2 Obstetrics and Open Access Gynaecology Cases - Reviews CASE REPORT Placental Site Nodule (PSN): An Uncommon Diagnosis with a Common Presentation 1* 2 Check for Sneha GS and Ramesh Kumar R updates 1Assistant Professor, Department of Obstetrics and Gynaecology, SDM Medical College and Hospital, SDM University, Karnataka, India 2Professor, Department of Obstetrics and Gynaecology, SDM Medical College and Hospital, SDM University, Karnataka, India *Corresponding author: DR. Sneha GS, Assistant Professor, Department of Obstetrics and Gynaecology, SDM Medical College and Hospital, SDM University, 580009, Dharwad, Karnataka, India ferentiated from aggressive lesions of intermediate tro- Abstract phoblast like placental site trophoblastic tumor and epi- Placental site nodule is an uncommon, benign, generally thelioid trophoblastic tumor and from nontrophoblastic asymptomatic lesion of trophoblastic origin, which may of- ten be detected several months to years after the tenancy diseases like squamous cell carcinoma [1,4]. from which it resulted. PSN usually presents as menorrha- gia, intermenstrual bleeding or an abnormal pap smear. Case Report PSN is benign, but it is important to distinguish it from the A 29-yrs-old female patient para 3, living 3, abor- other benign and malignant lesions like decidua, placental polyp, exaggerated placental site and placental site tropho- tion 5, underwent laprotomy and tubectomy 2 yrs back blastic tumor and squamous cell carcinoma. Follow ups of presented with history of irregular menstrual cycles typical PSNs do not show recurrence or malignant potential. with menorrhagia since 6 months preceded by normal PSN is an uncommon condition which should be suspected cycles. -

Histomorphological Study of Chorionic Villi in Products of Conception Following First Trimester Abortions
November, 2018/ Vol 4/ Issue 7 Print ISSN: 2456-9887, Online ISSN: 2456-1487 Original Research Article Histomorphological study of chorionic villi in products of conception following first trimester abortions Shilpa MD1, Supreetha MS2, Varshashree3 1Dr. Shilpa, MD, Assistant Professor, 2Dr. Supreetha, MS, Assistant Professor, 3Dr. Varshashree, Post graduate, all authors are affiliated with Department of Pathology, Sri Devaraj Urs Medical College, Tamaka, Kolar, Karnataka, India. Corresponding Author: Dr. Shilpa, MD, Assistant Professor, Department of Pathology, Sri Devaraj Urs Medical College, Tamaka, Kolar, Karnataka, India. Email id: [email protected] ………………………………………………………………………………………………………………………………... Abstract Background: The common problem which occurs in first trimester of pregnancy is miscarriage. Retained products of conception are commonly received specimen for histopathological examination. Apart from confirmation of pregnancy, a careful examination can provide some additional information about the cause or the conditions associated with abortion. Aim: 1. To study various histopathological changes occurring in chorionic villi in first trimester spontaneous abortions and to know the pathogenesis of abortions. Materials and methods: This was a cross sectional retrospective study carried out for over a period of 3 years from January 2015 to January 2018. A total of 235biopsies were obtained from patient with the diagnosis of the first trimester spontaneous abortions were included in this study. Results: In our study most common age group of the abortion was between 21-30 years (63%). Incomplete abortion was the commonest type of abortion (47.7%). Many dysmorphic features were observed in this study like hydropic change (67%), stromal fibrosis (62%), villi with reduced blood vessels (52.7%) and perivillous fibrin deposition. -

Characteristic Changes in Decidual Gene Expression Signature in Spontaneous Term Parturition
Journal of Pathology and Translational Medicine 2017; 51: 264-283 ▒ ORIGINAL ARTICLE ▒ https://doi.org/10.4132/jptm.2016.12.20 Characteristic Changes in Decidual Gene Expression Signature in Spontaneous Term Parturition Haidy El-Azzamy1,* · Andrea Balogh1,2,* Background: The decidua has been implicated in the “terminal pathway” of human term parturi- Roberto Romero1,3,4,5 · Yi Xu1 tion, which is characterized by the activation of pro-inflammatory pathways in gestational tissues. Christopher LaJeunesse1 · Olesya Plazyo1 However, the transcriptomic changes in the decidua leading to terminal pathway activation have Zhonghui Xu1 · Theodore G. Price1 not been systematically explored. This study aimed to compare the decidual expression of devel- Zhong Dong1 · Adi L. Tarca1,6 opmental signaling and inflammation-related genes before and after spontaneous term labor in Zoltan Papp7 · Sonia S. Hassan1,6 order to reveal their involvement in this process. Methods: Chorioamniotic membranes were 1,6 Tinnakorn Chaiworapongsa obtained from normal pregnant women who delivered at term with spontaneous labor (TIL, n = 14) 1,8,9 Chong Jai Kim or without labor (TNL, n = 15). Decidual cells were isolated from snap-frozen chorioamniotic mem- Nardhy Gomez-Lopez1,6 branes with laser microdissection. The expression of 46 genes involved in decidual development, Nandor Gabor Than1,6,7,10,11 sex steroid and prostaglandin signaling, as well as pro- and anti-inflammatory pathways, was ana- lyzed using high-throughput quantitative real-time polymerase chain reaction (qRT-PCR). Chorio- 1Perinatology Research Branch, NICHD/NIH/DHHS, amniotic membrane sections were immunostained and then semi-quantified for five proteins, and Bethesda, MD, and Detroit, MI, USA; 2Department of Immunology, Eotvos Lorand University, Budapest, immunoassays for three chemokines were performed on maternal plasma samples. -

Medical Abortion Reference Guide INDUCED ABORTION and POSTABORTION CARE at OR AFTER 13 WEEKS GESTATION (‘SECOND TRIMESTER’) © 2017, 2018 Ipas
Medical Abortion Reference Guide INDUCED ABORTION AND POSTABORTION CARE AT OR AFTER 13 WEEKS GESTATION (‘SECOND TRIMESTER’) © 2017, 2018 Ipas ISBN: 1-933095-97-0 Citation: Edelman, A. & Mark, A. (2018). Medical Abortion Reference Guide: Induced abortion and postabortion care at or after 13 weeks gestation (‘second trimester’). Chapel Hill, NC: Ipas. Ipas works globally so that women and girls have improved sexual and reproductive health and rights through enhanced access to and use of safe abortion and contraceptive care. We believe in a world where every woman and girl has the right and ability to determine her own sexuality and reproductive health. Ipas is a registered 501(c)(3) nonprofit organization. All contributions to Ipas are tax deductible to the full extent allowed by law. For more information or to donate to Ipas: Ipas P.O. Box 9990 Chapel Hill, NC 27515 USA 1-919-967-7052 [email protected] www.ipas.org Cover photo: © Ipas The photographs used in this publication are for illustrative purposes only; they do not imply any particular attitudes, behaviors, or actions on the part of any person who appears in the photographs. Printed on recycled paper. Medical Abortion Reference Guide INDUCED ABORTION AND POSTABORTION CARE AT OR AFTER 13 WEEKS GESTATION (‘SECOND TRIMESTER’) Alison Edelman Senior Clinical Consultant, Ipas Professor, OB/GYN Oregon Health & Science University Alice Mark Associate Medical Director National Abortion Federation About Ipas Ipas works globally so that women and girls have improved sexual and reproductive health and rights through enhanced access to and use of safe abortion and contraceptive care. -

Miscarriage Or Early Pregnancy Loss- Diagnosis and Management (Version 5)
Miscarriage or early pregnancy loss- diagnosis and management (Version 5) Guideline Readership This guideline applies to all women diagnosed with miscarriage in early pregnancy (up to 13 completed weeks) within the Heart of England Foundation Trust and to attending clinicians, sonographers and nursing staff on Gynaecology ward and early pregnancy unit. All care is tailored to individual patient needs, with an in-depth discussion of the intended risks and benefits for any intervention offered to woman with early pregnancy loss. Guideline Objectives The objective of this guideline is to enable all clinicians to recognise the different types of miscarriages and to follow a recognised management pathway so that all women with actual or suspected miscarriage receive, an appropriate and individualised care. Other Guidance Ectopic pregnancy and miscarriage: diagnosis and initial management. NICE guidance Dec 2012 Ratified Date: Insert Date Launch Date: 16 March 2018 Review Date: 16 March 2021 Guideline Author: Dr Rajmohan, Dr Cheema Contents & page numbers: 1. Flowcharts Flowchart 1 – Management of complete miscarriage p3 Flowchart 2 – Management of incomplete miscarriage p4 Flowchart 3 – Management of Missed miscarriage p5 Flowchart 4 - Management of Early fetal demise p6 Flowchart 5 – Medical management of miscarriage p7 Flowchart 6 - Surgical management (SMM) pathway p8 2. Executive summary and Overview p9 3. Body of guideline Types of miscarriage p9 Threatened miscarriage p9 Complete miscarriage p9 Incomplete miscarriage p9 Missed miscarriage -

Mammalogy Lecture 12
Mammalogy Lecture 11 - Reproduction I: General Patterns I. Obviously, reproduction is a very important aspect of biology and whole courses are dedicated to it. It’s easy to understand why reproductive traits would be subject to strong selection because of their direct effects on fitness. II. As we might expect, there are three basic types of mammalian reproduction. These correspond to the three major groups of mammals. Differences among these types reflect the degree of intimacy of fetal-maternal contact. A. Monotreme Type - Retain the primitive amniote pattern, but add a period of lactation. - Egg is very large at ovulation, about 3 mm. It moves down the oviduct where it is fertilized, then it’s coated with albumin, then a shell is laid down by a shell gland, and the shell is mineralized (with CaCO3). - Embryo spends 2-3 weeks in the uterus, then it’s laid. It’s large, 15 mm, when it’s laid. - Embryo growth is supported entirely by the yolk that’s enclosed in the egg. B. Metatherian type: - In some superficial ways it’s similar to monotremes, in that metatherians retain a shell membrane around the fertilized egg; a shell gland is present in Müllerian ducts. - However the shell is never mineralized and young are born live after only ca. 12 days, as we’ve seen, they are very altricial (poorly developed). - Initial intrauterine growth is supported by maternally by a placenta. - Metatherian placenta is the choriovitelline type - yolk-sac placenta (Eutherian placenta is called chorioallantoic placenta) C. Placenta Formation - Let’s look at formation of the placenta in Meta- & Eutherians. -

Regulation of Placental Autophagy by the Bcl-2 Family Proteins Myeloid Cell Leukemia Factor 1 (Mcl-1) and Matador/Bcl-2 Related Ovarian Killer (Mtd/Bok)
Regulation of Placental Autophagy by the Bcl-2 Family Proteins Myeloid Cell Leukemia Factor 1 (Mcl-1) and Matador/Bcl-2 Related Ovarian Killer (Mtd/Bok) by Manpreet Kalkat A thesis submitted in conformity with the requirements for the degree of Master of Science Department of Physiology University of Toronto © Copyright by Manpreet Kalkat, 2010 Regulation of Placental Autophagy by the Bcl-2 Family Proteins Myeloid Cell Leukemia Factor 1 (Mcl-1) and Matador/Bcl-2 Related Ovarian Killer (Mtd/Bok) Manpreet Kalkat Master of Science Department of Physiology University of Toronto 2010 Abstract The process of autophagy is defined as the degradation of cellular cytoplasmic constituents via a lysosomal pathway. Herein I sought to examine the regulation of autophagy in the placental pathologies preeclampsia (PE) and intrauterine growth restriction (IUGR). I hypothesized that the Bcl-2 family proteins Mcl-1L and MtdL regulate placental autophagy and contribute towards dysregulated autophagy in PE. My results demonstrate that Mcl-1L acts to repress autophagy via a Beclin 1 interaction, while MtdL induces autophagy when it interacts with Mcl-1L. My data indicate that while autophagy is elevated in PE, a pathology characterized by oxidative stress, it is decreased in IUGR, a hypoxic pathology. Treatment with sodium nitroprusside to mimic PE caused a decrease in Mcl-1L and an increase in MtdL levels in response to oxidative stress, thereby inducing autophagy. Overall, my data provide insight into the molecular mechanisms contributing to the pathogenesis of preeclampsia. ii Acknowledgments I would like to acknowledge the support my supervisor, Dr. Isabella Caniggia, who has provided me with many valuable lessons that have been instrumental in both my professional and personal growth in this early stage of my scientific career. -

Local Immune Regulation in Human Pregnancy with Focus on Decidual Macrophages
Linköping University Medical Dissertations No. 1016 Local immune regulation in human pregnancy with focus on decidual macrophages Charlotte Gustafsson Division of Clinical Immunology and Division of Obstetrics and Gynecology Department of Clinical and Experimental Medicine Faculty of Health Sciences, Linköping University SE-581 85 Linköping, Sweden Linköping 2007 © Charlotte Gustafsson 2007 Cover picture printed with permission from Articulate Graphics; www.articulategraphics.com Published articles have been reprinted with permission of respective copyright holder. Paper I © 2002 Blackwell Munksgaard Paper II © 2003 Blackwell Munksgaard Paper IV © 2006 Elsevier Ireland Ltd ISBN 978-91-85895-85-4 ISSN 0345-0082 Printed by LiU-Tryck, Linköping, Sweden, 2007 "There are no facts, only interpretations." Friedrich Nietzsche ABSTRACT During pregnancy, the woman carries a fetus partly foreign to her immune system, because of the expression of paternal antigens. Despite this, the fetus is normally tolerated and not rejected, as is often the case with organs in allogeneic transplantations. Systemic changes in maternal blood occur during pregnancy but, perhaps of greater importance, are changes in tissues locally in the uterus. The pregnant uterine endometrium, the decidua, is infiltrated by large numbers of leukocytes, mainly natural killer (NK) cells but also macrophages and T lymphocytes. Further, various cytokines are known to be secreted at the fetomaternal interface. However, the functions of these cells and the cytokine networks are not fully understood. The aim of this thesis was to investigate the local immune balance in normal human pregnancy decidua, both in the early phase of pregnancy and at parturition. First trimester decidual mononuclear cells, NK cells and macrophages were all shown to secrete IFN-γ, IL-4 and IL-10, as detected by ELISPOT. -

Implantation Site Intermediate Trophoblasts in Placenta Cretas
Modern Pathology (2004) 17, 1483–1490 & 2004 USCAP, Inc All rights reserved 0893-3952/04 $30.00 www.modernpathology.org Implantation site intermediate trophoblasts in placenta cretas Kyu-Rae Kim1, Sun-Young Jun1, Ji-Young Kim2 and Jae Y Ro1 1Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea and 2Department of Pathology, Cha General Hospital, College of Medicine Pochun Cha University, Seoul, Korea Placenta cretas are defined as abnormal adherences or ingrowths of placental tissue, but their pathogenetic mechanism has not been fully explained. During histologic examination of postpartum uteri, we noticed that the number of implantation site intermediate trophoblasts was increased in the placental bed of placenta cretas. To validate our observation and to address the pathogenetic role of implantation site intermediate trophoblasts in placenta cretas, we examined postpartum uteri with placenta cretas (n ¼ 34) and noncretas (n ¼ 22), obtained from Cesarean or immediate postpartum hysterectomy specimens. Using antibody to CD146, a marker for implantation site intermediate trophoblasts, we found that placenta cretas had significantly thicker layer of implantation site intermediate trophoblasts (230071200 lm) than noncretas (150071200 lm, Po0.025). We also observed that the confluent distribution of cells was more frequent in placenta cretas (97%) than noncretas samples (45%, Po0.001), and that the total number of implantation site intermediate trophoblasts within the superficial myometrium of the placental bed was significantly higher in placenta cretas than noncretas. Using antibodies to Ki-67, Bcl-2 and cleaved caspase-3 to determine the proliferative index and apoptotic rates of implantation site intermediate trophoblasts, we found that they were close to zero in both groups and did not differ significantly. -

Ectopic Pregnancy Management: Tubal and Interstitial SIGNS / SYMPTOMS DIAGNOSIS
8/29/19njm Ectopic Pregnancy Management: Tubal and interstitial SIGNS / SYMPTOMS Pain and vaginal bleeding are the hallmark symptoms of ectopic pregnancy. Pain is almost universal; it is generally lower abdominal and unilateral. Bleeding is also very common following a short period of amenorrhea. Physical exam may reveal a tender adnexal mass, often mentioned in texts, but noted clinically only 20 percent of the time. Furthermore, it may easily be confused with a tender corpus luteum of a normal intrauterine pregnancy. Finally signs and symptoms of hemoperitoneum and shock can occur, including a distended, silent, “doughy” abdomen, shoulder pain, bulging cul de sac into the posterior fornix of the vagina, and hypotension. DIAGNOSIS Initially, serum hCG rises, but then usually plateaus or falls. Transvaginal ultrasound scanning is a key diagnostic tool and can rapidly make these diagnoses: 1. Ectopic is ruled out by the presence of an intrauterine pregnancy with the exception of rare heterotopic pregnancy 2. Ectopic is proven when a gestational sac and an embryo with a heartbeat is seen outside of the uterus 3. Ectopic is highly likely if ANY adnexal mass distinct from the corpus luteum or a significant amount of free pelvic fluid is seen. When ultrasound is not definitive, correlation of serum hCG levels is important. If the hCG is above the “discriminatory zone” of 3000 mIU/ml IRP, a gestational sac should be visible on transvaginal ultrasound. The discriminatory zone varies by ultrasound machine and sonographer. If an intrauterine gestational sac is not visible by the time the hCG is at, or above, this threshold, the pregnancy has a high likelihood of being ectopic. -

Equine Placenta – Marvelous Organ and a Lethal Weapon
Equine placenta – marvelous organ and a lethal weapon Malgorzata Pozor, DVM, PhD, Diplomate ACT Introduction Placenta has been defined as: „an apposition between parent (usually maternal) and fetal tissue in order to establish physiological exchange” (1). Another definition of this important organ was proposed by Steven and Morris: „a device consisting of one or more transport epithelia located between fetal and maternal blood supply” (2). The main function of placenta is to provide an interface between the dam and the the fetus and to allow the metabolic exchange of the the nutrients, oxygen and waste material. The maternal circulation is brought into a close apposition to the fetal circulation, while a separation of these two circulatory systems remain separated (3). A degree and complexity of this „intimate relationship” varies greately between species mostly due to the structural diversity of the extraembryonic membranes of the vertebrates. The early feto-maternal exchange in the equine pregnancy is established as early as on day 22 after fertilization. The fetal and choriovitellin circulations are already present, the capsule ruptures and the allantois is already visible (4). The allantois starts expanding by day 32 and vascularizes approximately 90% of the chorion and fuses with it to form chorioallantois by day 38 of gestation (5). The equine placenta continues increasing its complexity till approximately day 150 of gestation. Equids have epitheliochorial placenta, there are six leyers separating maternal and fetal circulation, and there are no erosion of the luminal, maternal epithelium, like in ruminants (6). Thousands of small chorionic microvilli develop and penetrate into endometrial invaginations.