From Trophoblast to Human Placenta
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

3 Embryology and Development
BIOL 6505 − INTRODUCTION TO FETAL MEDICINE 3. EMBRYOLOGY AND DEVELOPMENT Arlet G. Kurkchubasche, M.D. INTRODUCTION Embryology – the field of study that pertains to the developing organism/human Basic embryology –usually taught in the chronologic sequence of events. These events are the basis for understanding the congenital anomalies that we encounter in the fetus, and help explain the relationships to other organ system concerns. Below is a synopsis of some of the critical steps in embryogenesis from the anatomic rather than molecular basis. These concepts will be more intuitive and evident in conjunction with diagrams and animated sequences. This text is a synopsis of material provided in Langman’s Medical Embryology, 9th ed. First week – ovulation to fertilization to implantation Fertilization restores 1) the diploid number of chromosomes, 2) determines the chromosomal sex and 3) initiates cleavage. Cleavage of the fertilized ovum results in mitotic divisions generating blastomeres that form a 16-cell morula. The dense morula develops a central cavity and now forms the blastocyst, which restructures into 2 components. The inner cell mass forms the embryoblast and outer cell mass the trophoblast. Consequences for fetal management: Variances in cleavage, i.e. splitting of the zygote at various stages/locations - leads to monozygotic twinning with various relationships of the fetal membranes. Cleavage at later weeks will lead to conjoined twinning. Second week: the week of twos – marked by bilaminar germ disc formation. Commences with blastocyst partially embedded in endometrial stroma Trophoblast forms – 1) cytotrophoblast – mitotic cells that coalesce to form 2) syncytiotrophoblast – erodes into maternal tissues, forms lacunae which are critical to development of the uteroplacental circulation. -

CCM2 and CCM3 Proteins Contribute to Vasculogenesis and Angiogenesis in Human Placenta
Histol Histopathol (2009) 24: 1287-1294 Histology and http://www.hh.um.es Histopathology Cellular and Molecular Biology CCM2 and CCM3 proteins contribute to vasculogenesis and angiogenesis in human placenta Gamze Tanriover1, Yasemin Seval1, Leyla Sati1, Murat Gunel2 and Necdet Demir1 1Department of Histology and Embryology, Akdeniz University, School of Medicine, Antalya, Turkey and 2 Department of Neurosurgery, Yale University, School of Medicine, New Haven, CT, USA Summary. Placenta as an ideal model to study Introduction angiogenic mechanisms have been established in previous studies. There are two processes, The placenta is a multifaceted organ that plays a vasculogenesis and angiogenesis, involved in blood critical role in maintaining and protecting the developing vessel formation during placental development. fetus. Normal development and function of the placenta Therefore, blood vessel formation is a crucial issue that requires extensive vasculogenesis and subsequent might cause vascular malformations. One of the vascular angiogenesis, in both maternal and fetal tissues. malformations is cerebral cavernous malformation Vasculogenesis is the formation of the primitive vascular (CCM) in the central nervous system, consisting of network de novo from progenitor cells, and angiogenesis endothelium-lined vascular channels without intervening is identified as the extension of blood vessels from normal brain parenchyma. Three CCM loci have been preexisting vascular structures (Demir et al., 1989, 2006; mapped as Ccm1, Ccm2, Ccm3 genes in CCM. In order Geva et al., 2002; Charnock-Jones et al., 2004). Many to investigate whether CCM proteins participate in blood factors, such as vascular endothelial growth factor vessel formation, we report here the expression patterns (VEGF), angiopoietins (Angpt-1 and -2) and their of CCM2 and CCM3 in developing and term human receptors are involved in the molecular regulation of placenta by means of immunohistochemistry and these diverse developmental steps. -
Fetal Brain Vascularity Visualized by Conventional 2D and 3D Power
DSJUOG Fetal Brain Vascularity Visualized by Conventional 2D and 3D Power Doppler Technology REVIEW ARTICLE Fetal Brain Vascularity Visualized by Conventional 2D and 3D Power Doppler Technology 1Ritsuko K Pooh, 2Asim Kurjak 1CRIFM Clinical Research Institute of Fetal Medicine PMC, Osaka, Japan 2Department of Obstetrics and Gynecology, University of Zagreb, School of Medicine, Zagreb, Croatia Correspondence: Ritsuko K Pooh, CRIFM Clinical Research Institute of Fetal Medicine PMC 7-3-7, Uehommachi, Tennoji Osaka #543-0001, Japan, Phone: +81-6-6775-8111, Fax: +81-6-6775-8122, e-mail: [email protected] Abstract Significant advances have been made in accurate and reliable visualization of the cerebral circulation in normal and abnormal pregnancies. They provided the non-invasive studies of fetal cerebral angiogenesis and further development that filled some of the gaps made by neuroanatomical studies alone. The first breakthrough in the assessment of fetal circulation was development of Doppler system with purpose to obtain velocity waveforms. Continuing technical advances in Doppler ultrasound equipment, especially highly sensitive color flow imagining techniques have made it possible to study smaller anatomical parts of fetal circulation system including cerebral vascularization. Before examination of brain vascularity, anatomical vascular structure and development on the different appearance at each gestational age should be remembered as the basic knowledge. Since the development of the embryo is rapid and significant changes occur during even one week it is important to specify the stage of the embryo or fetus both by age (postmenstrual weeks and days) and by size (crownrump length (CRL) and biparietal diameter (BPD). Introduction of three-dimensional (3D) sonography and 3D power Doppler techniques have enabled visualization of intracranial vessels. -

Defective Decidualization During and After Severe Preeclampsia Reveals a Possible Maternal Contribution to the Etiology
Defective decidualization during and after severe preeclampsia reveals a possible maternal contribution to the etiology Tamara Garrido-Gomeza,b,c,d, Francisco Dominguezb, Alicia Quiñonerob, Patricia Diaz-Gimenob, Mirhan Kapidzicc,d, Matthew Gormleyc,d, Katherine Onac,d, Pablo Padilla-Isertee, Michael McMasterf, Olga Genbacevc,d, Alfredo Peralese,g, Susan J. Fisherc,d,h,i,1,2, and Carlos Simóna,b,g,j,1,2 aFundación Igenomix, 46980 Valencia, Spain; bInstituto Universitario IVI, Instituto de Investigación Sanitaria Hospital Clinico de Valencia INCLIVA, 46010 Valencia, Spain; cCenter for Reproductive Sciences, University of California, San Francisco, CA 94143; dDepartment of Obstetrics, Gynecology, and Reproductive Sciences, University of California, San Francisco, CA 94143; eDepartment of Obstetrics and Gynecology, Hospital Universitario La Fe, 46026 Valencia, Spain; fDepartment of Cell and Tissue Biology, University of California, San Francisco, CA 94143; gDepartment of Obstetrics and Gynecology, School of Medicine, Valencia University, 46010 Valencia, Spain; hThe Eli & Edythe Broad Center for Regeneration Medicine and Stem Cell Research, University of California, San Francisco, CA 94143; iDepartment of Anatomy, University of California, San Francisco, CA 94143; and jDepartment of Obstetrics and Gynecology, School of Medicine, Stanford University, Palo Alto, CA 94305 Edited by R. Michael Roberts, University of Missouri-Columbia, Columbia, MO, and approved August 11, 2017 (received for review April 20, 2017) In preeclampsia (PE), cytotrophoblast (CTB) invasion of the uterus in studying the CTB subpopulation that invades the uterine wall in and spiral arteries is often shallow. Thus, the placenta’s role has the context of this syndrome. Targeted analyses of particular mo- been a focus. In this study, we tested the hypothesis that decidual lecular families, such as the vascular-type adhesion molecules that defects are an important determinant of the placental phenotype. -
PRG2 and AQPEP Are Misexpressed in Fetal Membranes in Placenta Previa and Percreta Elisa T. Zhang1, Roberta L. Hannibal1,6, Keyl
bioRxiv preprint doi: https://doi.org/10.1101/2020.08.14.248807; this version posted August 14, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-ND 4.0 International license. 1 PRG2 and AQPEP are misexpressed in fetal membranes in placenta previa and percreta 2 3 Elisa T. Zhang1, Roberta L. Hannibal1,6, Keyla M. Badillo Rivera1,7, Janet H.T. Song1,8, Kelly 4 McGowan1, Xiaowei Zhu1,2, Gudrun Meinhardt3, Martin Knöfler3, Jürgen Pollheimer3, Alexander 5 E. Urban1,2, Ann K. Folkins4, Deirdre J. Lyell5, Julie C. Baker1,5* 6 7 1DepartMent of Genetics, Stanford University School of Medicine, Stanford, California, United 8 States of AMerica. 9 2DepartMent of Psychiatry and Behavioral Sciences, Stanford University School of 10 Medicine, Stanford, California, United States of AMerica. 11 3DepartMent of Obstetrics and Gynaecology, Reproductive Biology Unit, Medical University of 12 Vienna, Vienna, Austria. 13 4DepartMent of Pathology, Stanford University School of Medicine, Stanford, California, United 14 States of AMerica. 15 5DepartMent of Obstetrics and Gynecology, Stanford University School of Medicine, Stanford, 16 California, United States of AMerica. 17 6Present address: Second GenoMe, Inc., Brisbane, California, United States of AMerica. 18 7Present address: Eversana Consulting, South San Francisco, California, United States of 19 AMerica. 20 8Present address: Division of Genetics and GenoMics, Boston Children’s Hospital, Harvard 21 Medical School, Boston, Massachusetts, United States of AMerica. 22 23 *Correspondence: [email protected] 24 300 Pasteur Dr. -

Placental Site Nodule (PSN): an Uncommon Diagnosis with a Common Presentation
ISSN: 2377-9004 Sneha and Ramesh Kumar. Obstet Gynecol Cases Rev 2021, 8:199 DOI: 10.23937/2377-9004/1410199 Volume 8 | Issue 2 Obstetrics and Open Access Gynaecology Cases - Reviews CASE REPORT Placental Site Nodule (PSN): An Uncommon Diagnosis with a Common Presentation 1* 2 Check for Sneha GS and Ramesh Kumar R updates 1Assistant Professor, Department of Obstetrics and Gynaecology, SDM Medical College and Hospital, SDM University, Karnataka, India 2Professor, Department of Obstetrics and Gynaecology, SDM Medical College and Hospital, SDM University, Karnataka, India *Corresponding author: DR. Sneha GS, Assistant Professor, Department of Obstetrics and Gynaecology, SDM Medical College and Hospital, SDM University, 580009, Dharwad, Karnataka, India ferentiated from aggressive lesions of intermediate tro- Abstract phoblast like placental site trophoblastic tumor and epi- Placental site nodule is an uncommon, benign, generally thelioid trophoblastic tumor and from nontrophoblastic asymptomatic lesion of trophoblastic origin, which may of- ten be detected several months to years after the tenancy diseases like squamous cell carcinoma [1,4]. from which it resulted. PSN usually presents as menorrha- gia, intermenstrual bleeding or an abnormal pap smear. Case Report PSN is benign, but it is important to distinguish it from the A 29-yrs-old female patient para 3, living 3, abor- other benign and malignant lesions like decidua, placental polyp, exaggerated placental site and placental site tropho- tion 5, underwent laprotomy and tubectomy 2 yrs back blastic tumor and squamous cell carcinoma. Follow ups of presented with history of irregular menstrual cycles typical PSNs do not show recurrence or malignant potential. with menorrhagia since 6 months preceded by normal PSN is an uncommon condition which should be suspected cycles. -

Human Pluripotent Stem Cells As a Model of Trophoblast Differentiation in Both Normal Development and Disease
Human pluripotent stem cells as a model of trophoblast differentiation in both normal development and disease Mariko Horiia,b,1, Yingchun Lia,b,1, Anna K. Wakelanda,b,1, Donald P. Pizzoa, Katharine K. Nelsona,b, Karen Sabatinib,c, Louise Chang Laurentb,c, Ying Liud,e,f, and Mana M. Parasta,b,2 aDepartment of Pathology, University of California, San Diego, La Jolla, CA 92093; bSanford Consortium for Regenerative Medicine, University of California, San Diego, La Jolla, CA 92093; cDepartment of Reproductive Medicine, University of California, San Diego, La Jolla, CA 92093; dDepartment of Neurosurgery, Center for Stem Cell and Regenerative Medicine, University of Texas Health Sciences Center, Houston, TX 77030; eThe Senator Lloyd and B. A. Bentsen Center for Stroke Research, University of Texas Health Sciences Center, Houston, TX 77030; and fThe Brown Foundation Institute of Molecular Medicine for the Prevention of Human Diseases, University of Texas Health Sciences Center, Houston, TX 77030 Edited by R. Michael Roberts, University of Missouri–Columbia, Columbia, MO, and approved May 25, 2016 (received for review March 24, 2016) Trophoblast is the primary epithelial cell type in the placenta, a Elf5 (Ets domain transcription factor) and Eomes (Eomeso- transient organ required for proper fetal growth and develop- dermin), also have been shown to be required for maintenance of ment. Different trophoblast subtypes are responsible for gas/nutrient the TSC fate in the mouse (8, 9). exchange (syncytiotrophoblasts, STBs) and invasion and maternal Significantly less is known about TE specification and the TSC vascular remodeling (extravillous trophoblasts, EVTs). Studies of niche in the human embryo (10, 11). -

Decidua Produces a Protein That Inhibits Choriogonadotrophin Release from Human Trophoblasts
Decidua produces a protein that inhibits choriogonadotrophin release from human trophoblasts. S G Ren, G D Braunstein J Clin Invest. 1991;87(1):326-330. https://doi.org/10.1172/JCI114990. Research Article To test the hypothesis that uterine decidua may modulate trophoblast function, trophoblasts and decidual cells were isolated from term placentas by enzymatic digestion and Percoll gradient centrifugation. Placental trophoblasts were cocultured with decidual cells and trophoblasts or JEG-3 choriocarcinoma cells were incubated with medium conditioned by decidual cells (DCM) for 72-96 h. In cocultures decidual cells inhibited choriogonadotropin (hCG) release from trophoblasts by 75% in comparison with controls (P less than 0.001). The DCM contained a factor that markedly inhibited hCG release from trophoblasts and JEG cells in vitro compared with controls. The inhibitory effect of the factor on hCG release was dose dependent, and could be eliminated by boiling the DCM for 30 min or proteolytic enzyme treatment. Ultrafiltration and Sephadex G-50 fractionation of the DCM indicated that the apparent molecular mass was 7,000-10,000 D. DCM also inhibited the stimulatory effect of exogenous cAMP on hCG secretion by JEG-3 cells, suggesting that DCM may interfere with activation of the cAMP-dependent protein kinases or transcription of hCG genes. These results suggest that the release of trophoblast hCG is under local paracrine control, regulated in part by a protein released by decidual cells. Find the latest version: https://jci.me/114990/pdf Decidua Produces a Protein that Inhibits Choriogonadotrophin Release from Human Trophoblasts Song-Guang Ren and Glenn D. -

Characteristic Changes in Decidual Gene Expression Signature in Spontaneous Term Parturition
Journal of Pathology and Translational Medicine 2017; 51: 264-283 ▒ ORIGINAL ARTICLE ▒ https://doi.org/10.4132/jptm.2016.12.20 Characteristic Changes in Decidual Gene Expression Signature in Spontaneous Term Parturition Haidy El-Azzamy1,* · Andrea Balogh1,2,* Background: The decidua has been implicated in the “terminal pathway” of human term parturi- Roberto Romero1,3,4,5 · Yi Xu1 tion, which is characterized by the activation of pro-inflammatory pathways in gestational tissues. Christopher LaJeunesse1 · Olesya Plazyo1 However, the transcriptomic changes in the decidua leading to terminal pathway activation have Zhonghui Xu1 · Theodore G. Price1 not been systematically explored. This study aimed to compare the decidual expression of devel- Zhong Dong1 · Adi L. Tarca1,6 opmental signaling and inflammation-related genes before and after spontaneous term labor in Zoltan Papp7 · Sonia S. Hassan1,6 order to reveal their involvement in this process. Methods: Chorioamniotic membranes were 1,6 Tinnakorn Chaiworapongsa obtained from normal pregnant women who delivered at term with spontaneous labor (TIL, n = 14) 1,8,9 Chong Jai Kim or without labor (TNL, n = 15). Decidual cells were isolated from snap-frozen chorioamniotic mem- Nardhy Gomez-Lopez1,6 branes with laser microdissection. The expression of 46 genes involved in decidual development, Nandor Gabor Than1,6,7,10,11 sex steroid and prostaglandin signaling, as well as pro- and anti-inflammatory pathways, was ana- lyzed using high-throughput quantitative real-time polymerase chain reaction (qRT-PCR). Chorio- 1Perinatology Research Branch, NICHD/NIH/DHHS, amniotic membrane sections were immunostained and then semi-quantified for five proteins, and Bethesda, MD, and Detroit, MI, USA; 2Department of Immunology, Eotvos Lorand University, Budapest, immunoassays for three chemokines were performed on maternal plasma samples. -

Self-Organized Amniogenesis by Human Pluripotent Stem Cells in a Biomimetic Implantation-Like Niche
LETTERS PUBLISHED ONLINE: 12 DECEMBER 2016 | DOI: 10.1038/NMAT4829 Self-organized amniogenesis by human pluripotent stem cells in a biomimetic implantation-like niche Yue Shao1†, Kenichiro Taniguchi2†, Katherine Gurdziel3, Ryan F. Townshend2, Xufeng Xue1, Koh Meng Aw Yong1, Jianming Sang1, Jason R. Spence2, Deborah L. Gumucio2* and Jianping Fu1,2,4* Amniogenesis—the development of amnion—is a critical factors seen in the in vivo amniogenic niche: a three-dimensional developmental milestone for early human embryogenesis (3D) extracellular matrix (ECM) that is provided by the basement and successful pregnancy1,2. However, human amniogenesis membrane surrounding the epiblast during implantation11; and a is poorly understood due to limited accessibility to peri- soft tissue bed provided by the uterine wall and trophoblast to implantation embryos and a lack of in vitro models. Here support the developing amnion (Fig. 1a,b). Since amniogenesis ini- we report an ecient biomaterial system to generate human tiates from the expanding pluripotent epiblast, we utilized mTeSR1 amnion-like tissue in vitro through self-organized development medium and basement membrane matrix (Geltrex) to render the of human pluripotent stem cells (hPSCs) in a bioengineered culture permissive for pluripotency maintenance. niche mimicking the in vivo implantation environment. We In this culture system, H9 human embryonic stem cells (hESCs) show that biophysical niche factors act as a switch to toggle were plated as single cells at 30,000 cells cm−2 onto a thick, hPSC self-renewal versus amniogenesis under self-renewal- soft gel bed of Geltrex (with thickness ≥100 µm, bulk Young's permissive biochemical conditions. We identify a unique modulus ∼900 Pa, coated on a glass coverslip), in mTeSR1 medium molecular signature of hPSC-derived amnion-like cells and supplemented with the ROCK inhibitor Y27632 (Fig. -

BMP-Treated Human Embryonic Stem Cells Transcriptionally Resemble Amnion Cells in the Monkey Embryo
bioRxiv preprint doi: https://doi.org/10.1101/2021.01.21.427650; this version posted January 22, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC 4.0 International license. BMP-treated human embryonic stem cells transcriptionally resemble amnion cells in the monkey embryo Sapna Chhabra1,2,3, Aryeh Warmflash2,4* 1Systems Synthetic and Physical Biology graduate program, 2Department of Biosciences, 4Department of Bioengineering, Rice University, Houston, TX 77005 3Present address: Developmental Biology Unit, EMBL Heidelberg. *Correspondence to AW: [email protected] Abstract Human embryonic stem cells (hESCs) possess an immense potential to generate clinically relevant cell types and unveil mechanisms underlying early human development. However, using hESCs for discovery or translation requires accurately identifying differentiated cell types through comparison with their in vivo counterparts. Here, we set out to determine the identity of much debated BMP-treated hESCs by comparing their transcriptome to the recently published single cell transcriptomes of early human embryos in the study Xiang et al 2019. Our analyses reveal several discrepancies in the published human embryo dataset, including misclassification of putative amnion, intermediate and inner cell mass cells. These misclassifications primarily resulted from similarities in pseudogene expression, highlighting the need to carefully consider gene lists when making comparisons between cell types. In the absence of a relevant human dataset, we utilized the recently published single cell transcriptome of the early post implantation monkey embryo to discern the identity of BMP-treated hESCs. -
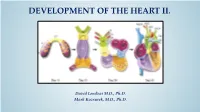
Development of Right Ventricle
DEVELOPMENT OF THE HEART II. David Lendvai M.D., Ph.D. Mark Kozsurek, M.D., Ph.D. • Septation of the common atrioventricular (AV) orifice. • Formation of the interatrial septum. • Formation of the muscular interventricular septum. • Appearance of the membranous interventricular septum and the spiral aorticopulmonary septum. right left septum primum septum primum septum primum septum primum septum primum septum primum foramen primum foramen primum septum primum septum primum foramen primum foramen primum septum primum septum primum foramen secundum foramen secundum foramen primum foramen primum septum primum foramen secundum septum primum foramen secundum foramen primum foramen primum septum primum septum primum foramen secundum foramen secundum septum secundum septum secundum foramen secundum foramen ovale foramen ovale septum primum septum primum septum secundum septum secundum foramen secundum foramen ovale foramen ovale septum primum septum primum septum secundum septum secundum foramen secundum septum primum foramen ovale foramen ovale septum primum SUMMARY • The septation of the common atrium starts with the appearance of the crescent-shaped septum primum. The opening of this septum, the foramen primum, becomes progressively smaller. • Before the foramen primum completly closes, postero-superiorly several small openings appear on the septum primum. These perforations coalesce later and form the foramen secundum. • On the right side of the septum primum a new septum, the septum secundum, starts to grow. The orifice of the septum secundum is the foramen ovale. • Finally two crescent-like, incomplete, partially overlapping septa exist with one hole on each. Septum secundum is more rigid and the septum primum on its left side acts as a valve letting the blood flow exclusively from the right to the left.