First Laboratory-Confirmed Outbreak of Human and Animal Rift Valley
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Informal Support for People with Alzheimer's Disease and Related D
Informal Support for People With Alzheimer’s Disease and Related Dementias in Rural Uganda: A Qualitative Study Pia Ngoma Nankinga ( [email protected] ) Mbarara University of Science and Technology Samuel Maling Maling Mbarara University of Science and Technology Zeina Chemali Havard Medical School Edith K Wakida Mbarara University of Science and Technology Celestino Obua Mbarara University of Science and Technology Elialilia S Okello Makerere University Research Keywords: Informal support, dementia and rural communities Posted Date: December 17th, 2019 DOI: https://doi.org/10.21203/rs.2.19063/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/16 Abstract Background: The generation of people getting older has become a public health concern worldwide. People aged 65 and above are the most at risk for Alzheimer’s disease which is associated with physical and behavioral changes. This nurtures informal support needs for people living with dementia where their families together with other community members are the core providers of day to day care for them in the rural setting. Despite global concern around this issue, information is still lacking on informal support delivered to these people with dementia. Objective: Our study aimed at establishing the nature of informal support provided for people with dementia (PWDs) and its perceived usefulness in rural communities in South Western Uganda. Methods: This was a qualitative study that adopted a descriptive design and conducted among 22 caregivers and 8 opinion leaders in rural communities of Kabale, Mbarara and Ibanda districts in South Western Uganda. The study included dementia caregivers who had been in that role for a period of at least six months and opinion leaders in the community. -

Land Use Change and Soil Degradation in the Southwestern Highlands of Uganda
LAND USE CHANGE AND SOIL DEGRADATION IN THE SOUTHWESTERN HIGHLANDS OF UGANDA Simon Bolwig A Contribution to the Strategic Criteria for Rural Investments in Productivity (SCRIP) Program of the USAID Uganda Mission The International Food Policy Research Institute 2033 K Street, N.W. Washington, D.C. 20006 September 2002 Strategic Criteria for Rural Investments in Productivity (SCRIP) is a USAID-funded program in Uganda implemented by the International Food Policy Research Institute (IFPRI) in collaboration with Makerere University Faculty of Agriculture and Institute for Environment and Natural Resources. The key objective is to provide spatially-explicit strategic assessments of sustainable rural livelihood and land use options for Uganda, taking account of geographical and household factors such as asset endowments, human capacity, institutions, infrastructure, technology, markets & trade, and natural resources (ecosystem goods and services). It is the hope that this information will help improve the quality of policies and investment programs for the sustainable development of rural areas in Uganda. SCRIP builds in part on the IFPRI project Policies for Improved Land Management in Uganda (1999-2002). SCRIP started in March 2001 and is scheduled to run until 2006. The origin of SCRIP lies in a challenge that the USAID Uganda Mission set itself in designing a new strategic objective (SO) targeted at increasing rural incomes. The Expanded Sustainable Economic Opportunities for Rural Sector Growth strategic objective will be implemented over the period 2002-2007. This new SO is a combination of previously separate strategies and country programs on enhancing agricultural productivity, market and trade development, and improved environmental management. Contact in Kampala Contact in Washington, D.C. -
Kabale District HRV Profile.Pdf
Kabale District Hazard, Risk and Vulnerability Profi le 2016 KABALE DISTRICT HAZARD, RISK AND VULNERABILITY PROFILE a Acknowledgement On behalf of Office of the Prime Minister, I wish to express my sincere appreciation to all of the key stakeholders who provided their valuable inputs and support to this Multi-Hazard, Risk and Vulnerability mapping exercise that led to the production of comprehensive district Hazard, Risk and Vulnerability (HRV) profiles. I extend my sincere thanks to the Department of Relief, Disaster Preparedness and Management, under the leadership of the Commissioner, Mr. Martin Owor, for the oversight and management of the entire exercise. The HRV assessment team was led by Ms. Ahimbisibwe Catherine, Senior Disaster Preparedness Officer supported by Ogwang Jimmy, Disaster Preparednes Officer and the team of consultants (GIS/DRR specialists); Dr. Bernard Barasa, and Mr. Nsiimire Peter, who provided technical support. Our gratitude goes to UNDP for providing funds to support the Hazard, Risk and Vulnerability Mapping. The team comprised of Mr. Steven Goldfinch – Disaster Risk Management Advisor, Mr. Gilbert Anguyo - Disaster Risk Reduction Analyst, and Mr. Ongom Alfred- Early Warning system Database programmer. My appreciation also goes to Kabale District Team. The entire body of stakeholders who in one way or another yielded valuable ideas and time to support the completion of this exercise. Hon. Hilary O. Onek Minister for Relief, Disaster Preparedness and Refugees KABALE DISTRICT HAZARD, RISK AND VULNERABILITY PROFILE i EXECUTIVE SUMMARY The multi-hazard vulnerability profile outputs from this assessment was a combination of spatial modeling using socio-ecological spatial layers (i.e. DEM, Slope, Aspect, Flow Accumulation, Land use, vegetation cover, hydrology, soil types and soil moisture content, population, socio-economic, health facilities, accessibility, and meteorological data) and information captured from District Key Informant interviews and sub-county FGDs using a participatory approach. -

Supporting Affordable and Green Buildings in Kigali/Rwanda
Kafunzo Merama Kagitumba Lake Mutanda Lake Bunyonyi Rwempasha Lubirizi Rutshuru Kisoro Nyagatare Cyanika Kabale a K b ag BIRUNGA m era u Butaro t NAT'L PARK Muvumba i g Kidaho Lac a Katuna K Lac Burera Rwanyakizinga Ruhengeri Mulindi Gatunda Lac Kirambo Cyamba Busogo Ruhondo Gabiro AKAGERA Byumba Ngarama Lac Kora NORRE NATIONAL Mikindi Mutura NORD PARK Lake Kagali Kinihira Lac Hago Mujunju Goma Nemba Gisenyi Rushashi Kinyami EST Muhura Nyundo Kabaya N Lac y Rutare Ngaru a Mbogo Murambi Kivumba ba Lac Rukara GISHWATI ro ng Shyorongi Muhazi NATURAL Ngororero Lac Ile Ihema Bugarura RESERVE Kiyumba KIGALI OUEST Kigali Rwamagana Ile Wahu Runda Gikoro Bulinga Kayonza Lac Lac Kicukiro Bicumbi Nasho Kivu Mabanza Lac SUPPORTING AFFORDABLE AND Gitarama Butamwa Kigarama Mugesera Lac Lake Ile Kibuye Mpanga Bisongou Birambo Lac Idjwi Mugesera Kibungo Cyambwe Gishyita Bwakira SUD Rilima Rukira Rwamatamu Masango Ruhango Sake Gashora Rusumo Gatagara Bare Nemba Kirehe Kaduha K Nyanza Ngenda ag Ile er Gombo Rwesero a Karaba Lac Lac Rusatira Cyohoha Rweru Kamembe Gisakura Gikongoro Sud Karama Bukavu Cyangugu Rwumba Kitabi Cyimbogo Karengera GREEN BUILDINGS IN KIGALI/RWANDA NYUNGWE Nyakabuye Bugumya NAT'L PARK Butare Ruramba Gisagara u r Busoro a y Bugarama n Munini ka A The boundaries and names shown and the designations used Runyombyi on this map do not imply official endorsement or acceptance by the United Nations. Map No. 3717 Rev. 11 UNITED NATIONS Department of Field Support July 2015 Geospatial Information Section (formerly Cartographic Section) Rwanda’s housing challenge Building materials and their environmental Impact analysis by building material type Rwanda’s National Housing Policy which was rolled out in impacts The impacts of exterior wall construction using nine locally available materials were compared and assessed relative to their share March 2015 aims at fast-tracking affordable housing projects The choice of building materials during the upgrading of of the city-wide flows in 2015. -
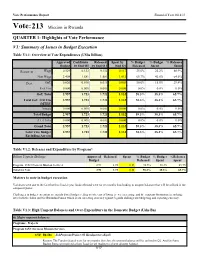
Vote:213 Mission in Rwanda
Vote Performance Report Financial Year 2018/19 Vote:213 Mission in Rwanda QUARTER 1: Highlights of Vote Performance V1: Summary of Issues in Budget Execution Table V1.1: Overview of Vote Expenditures (UShs Billion) Approved Cashlimits Released Spent by % Budget % Budget % Releases Budget by End Q1 by End Q 1 End Q1 Released Spent Spent Recurrent Wage 0.529 0.132 0.132 0.117 25.0% 22.2% 88.9% Non Wage 2.408 1.581 1.581 1.012 65.7% 42.0% 64.0% Devt. GoU 0.020 0.010 0.010 0.003 50.0% 15.0% 29.4% Ext. Fin. 0.000 0.000 0.000 0.000 0.0% 0.0% 0.0% GoU Total 2.957 1.723 1.723 1.132 58.3% 38.3% 65.7% Total GoU+Ext Fin 2.957 1.723 1.723 1.132 58.3% 38.3% 65.7% (MTEF) Arrears 0.000 0.000 0.000 0.000 0.0% 0.0% 0.0% Total Budget 2.957 1.723 1.723 1.132 58.3% 38.3% 65.7% A.I.A Total 0.000 0.000 0.000 0.000 0.0% 0.0% 0.0% Grand Total 2.957 1.723 1.723 1.132 58.3% 38.3% 65.7% Total Vote Budget 2.957 1.723 1.723 1.132 58.3% 38.3% 65.7% Excluding Arrears Table V1.2: Releases and Expenditure by Program* Billion Uganda Shillings Approved Released Spent % Budget % Budget %Releases Budget Released Spent Spent Program: 1652 Overseas Mission Services 2.96 1.72 1.13 58.3% 38.3% 65.7% Total for Vote 2.96 1.72 1.13 58.3% 38.3% 65.7% Matters to note in budget execution Variances were due to the fact that this finacial year funds released were for six months thus leading to unspent balances that will be utilised in the subquent Quater. -

Kabale District Local Government Councils' Scorecard FY 2018/19
KABALE DISTRICT LOCAL GOVERNMENT council SCORECARD assessment FY 2018/19 KABALE DISTRICT LOCAL GOVERNMENT council SCORECARD assessment FY 2018/19 L-R: Ms. Rose Gamwera, Secretary General ULGA; Mr. Ben Kumumanya, PS. MoLG and Dr. Arthur Bainomugisha, Executive Director ACODE in a group photo with award winners at the launch of the 8th Local Government Councils Scorecard Report FY 2018/19 at Hotel Africana in Kampala on 10th March 2020 1.0 Introduction agrarian with majority of the population engaged in Agriculture. Some of the crops grown in the This brief was developed from the scorecard district include Irish potatoes, cereals, beans, report titled, “The Local Government Councils coffee and matooke. Administratively, the district Scorecard FY 2018/19. The Next Big Steps: consists of 3 Counties of Ndorwa East, Ndorwa Consolidating Gains of Decentralization and West and Kabale Municipality. The three counties Repositioning the Local Government Sector in are further sub divided into 12 sub counties. Uganda.” The brief provides key highlights of 1.2 The Local Government Councils the performance of elected leaders and Council Scorecard Initiative (LGCSCI) of Kabale District Local Government during FY 2018/19. The main building blocks in LGCSCI are the principles and core responsibilities of Local 1.1 Brief about Kabale District Governments as set out in Chapter 11 of the Kabale District is located in the Western part of Constitution of the Republic of Uganda, the Uganda and originally was part of Kigezi District Local Governments Act (CAP 243) under before the Districts of Rukungiri, Kanungu and Section 10 (c), (d) and (e). -

Cross-Border Health Integrated Partnership Project
Cross-Border Health Integrated Partnership Project Cross-Border Health Integrated Partnership Project (CB-HIPP) is supported by the U.S. Agency for International Development (USAID) with funding CB-HIPP from the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR). Overview The Cross-Border Health Integrated Partnership Project (CB-HIPP), supported by the U.S. Agency for International Development (USAID) with funding from the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR), is designed to extend quality integrated health services in strategic border areas and other transport corridor sites in East, Central and Southern Africa. In addition to service delivery and the Southern African De- Goal focused on key and vulnerable velopment Community (SADC) The goal of CB-HIPP is to cata- populations, the project (Sep- will play a key leadership and lyze and support sustainable tember 2014-August 2019) partnership role on CB-HIPP. and African-led regional health recognizes the need for alterna- development partnerships Partners tive health financing to increase to improve health outcomes uptake and sustainability of • FHI 360 (Prime) among mobile populations and services within an enabling • Abt Associates vulnerable communities resid- • African Institute for Development policy environment. USAID’s Policy (AFIDEP) ing along Eastern, Central, and design highlights the substan- • (The) African Network for Strategic Southern African transport cor- tial progress made in regional Communication in Health and ridors and cross-border sites. integration, trade, and infra- Development (AfriComNet) structure development through • Development Alternatives Inc. (DAI) This goal will be achieved • Federation of East African Freight Power Africa and Trade Africa Forwarders Associations (FEAFFA) through three Results: (PATA) and other initiatives. -

CURRICULUM VITAE Professor Joy Constance Kwesiga (March 2020)
CURRICULUM VITAE Professor Joy Constance Kwesiga (March 2020) A. PERSONAL INFORMATION: NAME: Joy Constance Kwesiga DATE OF BIRTH: 03rd May 1943 SEX: Female NATIONALITY: Ugandan CONTACT: Kabale University P. O. Box 317 Kabale, Uganda. Tel: +256-772485267 / +256-751812325 E-mail: [email protected] or [email protected] or [email protected] B. BRIEF BIO FOR JOY KWESIGA Professor Joy Constance Kwesiga, Ph.D (London), is an experienced academician, University Administrator and Social Development Analyst and a renowned gender and Women advocate and mentor. She has had an enviable privilege of combining academic work with women’s rights activist work. She has been a Professor of Gender Studies and the Vice Chancellor of Kabale University since November 2005 to date. She oversaw the transformation of Kabale University from a Private Community University to a Public University (since 2015). Even when Kabale University was a private University, she effectively steered it to attain an Operating Licence in 2005, and a University Charter in 2014. Previously, Professor Kwesiga served at various levels as a University Administrator at Makerere University, rising from the ranks to the level of Deputy Academic Registrar. She then switched to the academic arena, serving as the Head of the Department of Women and Gender Studies, and later became the Dean of the Faculty of Social Sciences at Makerere University. Professor Kwesiga was the founding Head of the Gender Mainstreaming Division of the Academic Registrar’s Department at Makerere University. The goal of the Gender Mainstreaming Programme is to make Makerere University an all-inclusive institution. Professor Kwesiga was able to lay its foundation. -

Backparkers-Brochure.Pdf
Accommodation Prices 2018. Accomodation rates in $(USD) Per person per night I N D I Accomodation type Bed only Bed & Breakfast Half Board Full Board B W Self Camping $10PP $15PP $25PP $35PP Min Dormitory (4 Beds) $20PP $25PP $35PP $45PP Big Dormitory (6 Beds and above) $15PP $20PP $30PP $40PP Rent a mobile tent with beddings $15PP $20PP $30PP $40PP B Rent a mobile tent without beddings (pp) $12PP $17PP $27PP $35PP a e ck dg Twin Bed/Double Rooms with shared Bathroom $25PP $30PP $40PP $50PP packers Lo Single Bed room with shared Bathroom $30PP $35PP $45PP $55PP Twin Bed/Double Rooms self contained $40PP $45PP $55PP $65PP Single Bed Room self contained $45PP $50PP $60PP $70PP BWINDI BACKPACKERS LODGE Twin/Double Bedroom cottage $50PP $55PP $65PP $75PP Single Bedroom cottage $60PP $65PP $75PP $85PP LAST MINUTE GORILLA TRACKING PERMITS AND 3 Bedroom cottage $45PP $50PP $60PP $70PP ACTIVE NYIRAGONGO VOLCANO TREKKING/HIKING PERMITS AVAILABLE We accept payment by the following cards at no extra cost or by Mobile money on any of the following telephone numbers; To all clients paying for bed +256772661854, +256752661854, +256774883710 and breakfast, half board and full board, we serve full continental breakfast & for meals they are 3 course meals. Alcarte menu available for single course meals. Note:Prices can change without prio notice Note: half board includes Bed, You can pay by card on our website at no extra fees or Breakfast and Lunch or Dinner request for a card payment link by e-mail.. while full board includes Breakfast, Lunch & Dinner, It Half the price double the Fun!! excludes drinks Lodge shuttle: Departs from Kabale at 10:30am & 4:00pm. -

The Republic of Uganda Ministry of Health Press
THE REPUBLIC OF UGANDA MINISTRY OF HEALTH PRESS STATEMENT UPDATE ON COVID-19 RESPONSE IN UGANDA 22 December 2020 Dr. Joyce Moriku Kaducu Minister of State for Health in charge of Primary Health Care 22nd December 2020 - The Ministry of Health would like to update the general public on the status of the COVID-19Pandemic in Uganda. OVERVIEW OF COVID-19 - THE NEW VARIANT STRAIN The Ministry of Health is closely followingthe global trends of a new variant strain (501. V2) of SARSCoV-2that has been reported in the United Kingdom, other parts of Europe and now South Africa and Nigeria. It has been shown to spread much faster but so far no evidence of high severity than the first strain. So far, we know that the new variant strain is spreading faster than what we experienced in the 1st wave. It is important to note that this new variant strain has NOT been reported in Uganda. The Ministry of Health working with regional partners, Africa CDC through Uganda Virus Research Institute (UVRI)will start genome surveillance for the new strain to determine its prevalence in the country. However, we know that the transmission of the virusxand the control measures remain the same as the virus in the 1st wave. i.e. Consistent mask use, social distancing and good hand hygiene. COVID-19 IN UGANDA As you are all aware, Uganda is in phase 4 of the pandemic. This means that there is intense and widespread community transmission of COVID-19in nearly all districts and with occasional and emerging hotspots. -

Consultancy Services for Feasibility Study and Detailed Engineering
CONSULTANCY SERVICES FOR FEASIBILITY STUDY AND DETAILED ENGINEERING DESIGN FOR UPGRADING OF SELECTED NATIONAL ROADS (8 LOTS): LOT 5: KABALE-BUNYONYI (7.8KM), BUNYONYI-KABEHO (7.3KM) KISORO-MGAHINGA GATE (13.4 KM) AND NYARUSIZA- MUHABURA GATE (5.3 KM) UGANDA NATIONAL ROADS AUTHORITY ENVIRONMENTAL AND SOCIAL IMPACT STATEMENT April 2020 (Revised version) Proposed upgrade of Kabale-Bunyonyi (7.8km), Bunyonyi-Kabeho (7.3km), Kisoro-Mgahinga Gate (13.4km) and Nyarusiza- Mahabura Gate road (5.3km) from Gravel to bituminous standard ESIA TEAM Name Position on Study Team Dr. Charles Koojo Amooti - EIA Specialist Team Leader Mr. Moses Oluka - Natural Resource Specialist Mr. Samuel David Wafula - Land Use Expert Mr. Agaba Muluba Matia - Terrestrial Ecologist Mrs. Betty Dungu - Sociologist Eng. Aaron Nsamba - Civil Engineer Eng. Simone ZOPPELLARI - Traffic Engineer Mr. Marco De Marco - Hydrologist Mr. Alessandro PIAZZA - Road Safety Specialist Eng. Riccardo Centonze - Civil Engineer Dr. Collins Bulafu - Botanist Mr. David Mugisa - Occupational Health Expert Mr. Protazio Rwaburindori - Botanist Mr. Musitwa Paul - Occupational Hygienist Mr. Wycliffe Ogello - GIS Analyst REVIEW AND UPDATE TEAM Department of Environment and Social Safegurds, Directorate of Network Planning and Engineering, UNRA Name Speciality Seruma E. MONICAH Head, ESS Environment and Social Safeguards Karugaba BRIAN Environmental Specialist Physical Environment Lukwago WILBER Senior Environmnt Officer Bological Environment Dr. Bagwana PETER Social Development Specialist Socioeconomics Nabuccu REBECCA Senior Sociologist Socioeconomics Seguya HENRY Social Development Specialist Socioeconomics i Proposed upgrade of Kabale-Bunyonyi (7.8km), Bunyonyi-Kabeho (7.3km), Kisoro-Mgahinga Gate (13.4km) and Nyarusiza- Mahabura Gate road (5.3km) from Gravel to bituminous standard TABLE OF CONTENTS ESIA TEAM ........................................................................................................................................ -

Download International Students' Brochure
Brief Inf ormation Brochure - for - International Students Kabale University. P.O Box 317, Kabale - Uganda Address: Plot 364 Block 3 Kikungiri Hill, Kabale Municipality +256 7 82860259 | +2567486426463 inf [email protected] | [email protected] Brief information Brochure for International Students Experience Education in the Pearl of Africa. Introduction No matter where you come from or what you would like to do when you graduate, Kabale University experience will challenge, inspire, develop and support you. Through a combination of excellent teaching, a rich and varied campus life and a cultured community, you'll have the experience of a lifetime. The University is a home away from home to many international students and we always have nice warm people welcoming you from all around the world. We are sure and confident that life at Kabale University (KAB) is pretty relaxed and you will love the ambiance other students and staff accord to you. Background Information Kabale University is located on Plot 364 Block 3 Kikungiri Hill, in Kabale Municipality, about a kilometre off Kabale-Katuna-Kigali Highway. The Main Campus sits on 50 acres of land. The University can be accessed via Mukombe Road, which connects the Kikungiri Campus to the Highway. An additional Campus is located on Plots 66-76 in Nyabikoni Parish in the Central Division of Kabale Municipality comprising of 3 acres. This houses the Faculty of Engineering, Technology, Applied Design and Fine Art. Kabale University School of Medicine is partially housed on Makanga Hill, in the Kabale Regional Referral Hospital next to the headquarters of Kabale District Local Government.