A Patient's Guide to Biceps Tendon Tears at the Elbow
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bone Limb Upper
Shoulder Pectoral girdle (shoulder girdle) Scapula Acromioclavicular joint proximal end of Humerus Clavicle Sternoclavicular joint Bone: Upper limb - 1 Scapula Coracoid proc. 3 angles Superior Inferior Lateral 3 borders Lateral angle Medial Lateral Superior 2 surfaces 3 processes Posterior view: Acromion Right Scapula Spine Coracoid Bone: Upper limb - 2 Scapula 2 surfaces: Costal (Anterior), Posterior Posterior view: Costal (Anterior) view: Right Scapula Right Scapula Bone: Upper limb - 3 Scapula Glenoid cavity: Glenohumeral joint Lateral view: Infraglenoid tubercle Right Scapula Supraglenoid tubercle posterior anterior Bone: Upper limb - 4 Scapula Supraglenoid tubercle: long head of biceps Anterior view: brachii Right Scapula Bone: Upper limb - 5 Scapula Infraglenoid tubercle: long head of triceps brachii Anterior view: Right Scapula (with biceps brachii removed) Bone: Upper limb - 6 Posterior surface of Scapula, Right Acromion; Spine; Spinoglenoid notch Suprspinatous fossa, Infraspinatous fossa Bone: Upper limb - 7 Costal (Anterior) surface of Scapula, Right Subscapular fossa: Shallow concave surface for subscapularis Bone: Upper limb - 8 Superior border Coracoid process Suprascapular notch Suprascapular nerve Posterior view: Right Scapula Bone: Upper limb - 9 Acromial Clavicle end Sternal end S-shaped Acromial end: smaller, oval facet Sternal end: larger,quadrangular facet, with manubrium, 1st rib Conoid tubercle Trapezoid line Right Clavicle Bone: Upper limb - 10 Clavicle Conoid tubercle: inferior -

Trapezius Origin: Occipital Bone, Ligamentum Nuchae & Spinous Processes of Thoracic Vertebrae Insertion: Clavicle and Scapul
Origin: occipital bone, ligamentum nuchae & spinous processes of thoracic vertebrae Insertion: clavicle and scapula (acromion Trapezius and scapular spine) Action: elevate, retract, depress, or rotate scapula upward and/or elevate clavicle; extend neck Origin: spinous process of vertebrae C7-T1 Rhomboideus Insertion: vertebral border of scapula Minor Action: adducts & performs downward rotation of scapula Origin: spinous process of superior thoracic vertebrae Rhomboideus Insertion: vertebral border of scapula from Major spine to inferior angle Action: adducts and downward rotation of scapula Origin: transverse precesses of C1-C4 vertebrae Levator Scapulae Insertion: vertebral border of scapula near superior angle Action: elevates scapula Origin: anterior and superior margins of ribs 1-8 or 1-9 Insertion: anterior surface of vertebral Serratus Anterior border of scapula Action: protracts shoulder: rotates scapula so glenoid cavity moves upward rotation Origin: anterior surfaces and superior margins of ribs 3-5 Insertion: coracoid process of scapula Pectoralis Minor Action: depresses & protracts shoulder, rotates scapula (glenoid cavity rotates downward), elevates ribs Origin: supraspinous fossa of scapula Supraspinatus Insertion: greater tuberacle of humerus Action: abduction at the shoulder Origin: infraspinous fossa of scapula Infraspinatus Insertion: greater tubercle of humerus Action: lateral rotation at shoulder Origin: clavicle and scapula (acromion and adjacent scapular spine) Insertion: deltoid tuberosity of humerus Deltoid Action: -

Biceps Anatomical Aberration in a Cadaveric Study
CaseReport32 Indian Journalof Anatomy Volume 7Number 3, May -June 2018 DOI: http://dx.doi.org/10.21088/ija.2320.0022.7318.24 BicepsAnatomicalAberrationinaCadavericStudy ViayAnanth K. Abstract InaroutinecadavericdissectionsinacadavertheshortheadofBicepsBrachiitendon(SBT)showedbifurcated inattachmentwiththebellyofthePronatorTeresmuscleseenalongwithitsusualcourseofattachmentwiththe radialtuberosity. Thiswas seenbilaterally on boththe upperlimbs inthesame bodyduringthe anatomical dissection.erethebicepsbrachiiwasoriginatingfromthelongheadfromthesupraglenoidtuberclefromthe capusularjointandtheshortheadfromthecoracoidprocessofscapula. KeywordsBicepsBrachiiandPronatorTeresMuscleExtrarticularInsertionCadaver. Introduction Intheupperextremitytheanteriorcompartment formstheflexorgroupmusclesofwhichalongwith thecoracobrachialistheBicepsBrachiiplaysamajor roleinflexingthearmsandtheelbowjoint.It compensatestheactionwiththeTricepsBrachiithe posteriorcompartmentmuscleofthebrachiumwhich formstheextensors. Itisalargefusiformmuscleofthatcompartment 3,8andaprimarysupinatoroftheforearm.Biceptal aponeurosis,atriangularbandformedfromthedeep fasciaoriginatesfromthebicepstendon.This aponeurosisgivesprotectiontothecubitalfossa.A thirdhead is also reportedseen posterior to the brachialartery8. Itoriginatesfromlongandshortheadsfrom supraglenoidtubercleandcoracoidsprocessof scapularespectively. Andboththeheadsconvergewiththetwobelles andgetsinsertedintotheposteriorpartofthe tuberosityofradiusbone9. Fi.Rt.SideArm Authors AffiliationLecturer,DepartmentofAnatomy, igure1showsBicepsBrachiiinthefrontof -

The Anatomy of the Bicipital Tuberosity and Distal Biceps Tendon
The anatomy of the bicipital tuberosity and distal biceps tendon Augustus D. Mazzocca, MD,a Mark Cohen, MD,b Eric Berkson, MD,b Gregory Nicholson, MD,b Bradley C. Carofino, MD,a Robert Arciero, MD,a and Anthony A. Romeo, MDb Farmington, CT, and Chicago, IL The anatomy of the distal biceps tendon and bicipi- and the mean BT-radial styloid angle is 123° Ϯ 10°. tal tuberosity (BT) is important in the pathophysiol- None of the measurements correlated with patient ogy of tendon rupture, as well as surgical repair. age, sex, or race. We concluded that the morphology Understanding the dimensions of the BT and its an- of the BT ridge is variable. The insertion footprint of gular relationship to the radial head and radial the distal biceps tendon is on the ulnar aspect of the styloid will facilitate surgical procedures such as re- BT ridge. The dimensions of the radius and BT are ap- construction of the distal biceps tendon, radial head plicable to several surgical procedures about the el- prosthesis implantation, and reconstruction of proxi- bow. (J Shoulder Elbow Surg 2007;16:122-127.) mal radius trauma. We examined 178 dried cadav- eric radii, and the following measurements were col- The recognition and treatment of distal biceps ten- lected: radial length, length and width of the BT, don ruptures have increased over time. Previously, diameter of the radius just distal to the BT, distance this injury was considered rare; only 65 cases were from the radial head to the BT, radial head diame- reported before 1941.2,4 However, a more recent ter, width of the radius at the BT, radial neck-shaft retrospective study identified the incidence to be 1.2 10 angle, and styloid angle. -

RADIOULNAR JOINTS the Radius and Ulna Articulate by –
RADIOULNAR JOINTS The radius and ulna articulate by – • Synovial 1. Superior radioulnar joint 2. Inferior radioulnar joint • Non synovial Middle radioulnar union Superior Radioulnar Joint This articulation is a trochoid or pivot-joint between • the circumference of the head of the radius • ring formed by the radial notch of the ulna and the annular ligament. The Annular Ligament (orbicular ligament) This ligament is a strong band of fibers, which encircles the head of the radius, and retains it in contact with the radial notch of the ulna. It forms about four-fifths of the osseo- fibrous ring, and is attached to the anterior and posterior margins of the radial notch a few of its lower fibers are continued around below the cavity and form at this level a complete fibrous ring. Its upper border blends with the capsule of elbow joint while from its lower border a thin loose synovial membrane passes to be attached to the neck of the radius The superficial surface of the annular ligament is strengthened by the radial collateral ligament of the elbow, and affords origin to part of the Supinator. Its deep surface is smooth, and lined by synovial membrane, which is continuous with that of the elbow-joint. Quadrate ligament A thickened band which extends from the inferior border of the annular ligament below the radial notch to the neck of the radius is known as the quadrate ligament. Movements The movements allowed in this articulation are limited to rotatory movements of the head of the radius within the ring formed by the annular ligament and the radial notch of the ulna • rotation forward being called pronation • rotation backward, supination Middle Radioulnar Union The shafts of the radius and ulna are connected by Oblique Cord and Interosseous Membrane The Oblique Cord (oblique ligament) The oblique cord is a small, flattened band, extending downward and laterally, from the lateral side of the ulnar tuberosity to the radius a little below the radial tuberosity. -

Shoulder Anatomy
ShoulderShoulder AnatomyAnatomy www.fisiokinesiterapia.biz ShoulderShoulder ComplexComplex BoneBone AnatomyAnatomy ClavicleClavicle – Sternal end – Acromion end ScapulaScapula Acromion – Surfaces end Sternal Costal end Dorsal – Borders – Angles ShoulderShoulder ComplexComplex BoneBone AnatomyAnatomy Scapula 1. spine 2. acromion 3. superior border 4. supraspinous fossa 5. infraspinous fossa 6. medial (vertebral) border 7. lateral (axillary) border 8. inferior angle 9. superior angle 10. glenoid fossa (lateral angle) 11. coracoid process 12. superior scapular notch 13 subscapular fossa 14. supraglenoid tubercle 15. infraglenoid tubercle ShoulderShoulder ComplexComplex BoneBone AnatomyAnatomy HumerousHumerous – head – anatomical neck – greater tubercle – lesser tubercle – greater tubercle – lesser tubercle – intertubercular sulcus (AKA bicipital groove) – deltoid tuberosity ShoulderShoulder ComplexComplex BoneBone AnatomyAnatomy HumerousHumerous – Surgical Neck – Angle of Inclination 130-150 degrees – Angle of Torsion 30 degrees posteriorly ShoulderShoulder ComplexComplex ArticulationsArticulations SternoclavicularSternoclavicular JointJoint – Sternal end of clavicle with manubrium/ 1st costal cartilage – 3 degree of freedom – Articular Disk – Ligaments Capsule Anterior/Posterior Sternoclavicular Ligament Interclavicular Ligament Costoclavicular Ligament ShoulderShoulder ComplexComplex ArticulationsArticulations AcromioclavicularAcromioclavicular JointJoint – 3 degrees of freedom – Articular Disk – Ligaments Superior/Inferior -
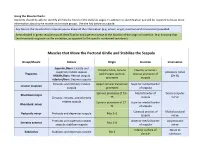
Muscle Charts: Students Should Be Able to Identify All Muscles Listed on the Daily Lab Pages
Using the Muscle Charts: Students should be able to identify all muscles listed on the daily lab pages. In addition to identification you will be required to know more information about some muscle and muscle groups. Use the key below as a guide. Any box on the muscle chart requires you to know all the information (e.g. action, origin, insertion and innervation) provided. Areas shaded in green require muscle identification and a general sense of the location of the origin or insertion. (e.g. knowing that the rhomboids originate on the vertebrae, as opposed to the specific numbered vertebrae). Muscles that Move the Pectoral Girdle and Stabilize the Scapula Group/Muscle Actions Origin Insertion Innervation Superior fibers: Elevate and Occipital bone, cervical Clavicle; acromion superiorly rotate scapula Accessory nerve Trapezius and thoracic spinous process and spine of Middle fibers: Retract scapula (CN XI) processes scapula Inferior fibers: Depress scapula Elevates and inferiorly rotates Upper cervical transverse Superior medial border Levator scapulae scapula processes of scapula Spinous processes of T2– Medial border of Dorsal scapular Rhomboid major Elevates, retracts, and inferiorly T5 scapula nerve rotates scapula Spinous processes of C7– Superior medial border Rhomboid minor T1 of scapula Coracoid process of Medial pectoral Pectoralis minor Protracts and depresses scapula Ribs 3–5 scapula nerve Protracts and superiorly rotates Anterior medial border Long thoracic Serratus anterior Ribs 1–8 scapula; stabilizes scapula of scapula nerve -

Case Report Mineralisation of the Biceps Brachii Tendon in a 6-Year-Old Cob Mare S
74 EQUINE VETERINARY EDUCATION / AE / March 2007 Case Report Mineralisation of the biceps brachii tendon in a 6-year-old Cob mare S. J. BOYS SMITH† AND E. R. SINGER* Philip Leverhulme Large Animal Hospital, Leahurst, University of Liverpool, Chester High Road, Neston, Cheshire CH64 7TE, UK. Keywords: horse; biceps brachii tendon; mineralisation; calcification Introduction Diagnostic techniques: The lameness did not change following regional analgesia using 2% mepivicaine Mineralisation of the biceps brachii tendon is an uncommon hydrochloride (Intra-Epicaine)1 of the palmar digital nerves, condition in horses (Adams and Blevins 1989a) and may be palmar nerves at the level of the proximal sesamoid bones, associated with bicipital bursitis and osseous pathology palmar and palmar metacarpal nerves at the level of the distal (Fugaro and Adams 2002). Calcifying tendonopathy has been metacarpus, palmar metacarpal nerves at the level of the reported previously in dogs and man (Muir et al. 1992). proximal metacarpus and the median and ulnar nerves; or This case report describes the presentation, following intrasynovial anaesthesia of the middle carpal, diagnosis and pathological findings in a mare with antebrachiocarpal, elbow and shoulder joints and mineralisation of the biceps brachii tendon. These intertubercular bursa (Bassage and Ross 2003). findings demonstrate advanced pathology despite mild Nuclear scintigraphy was performed 2 weeks following clinical signs on initial presentation. diagnostic analgesia as a result of the negative findings. On re-examination, the lameness had deteriorated by one grade. Case details The mare was given 10 MBq/kg bwt i.v. 99mtechnetium methylene-diphosphonate (99Tc-MDP)2 through a 14 gauge History catheter (Intraflon 2)3. -

Applied Anatomy of the Elbow
Applied anatomy of the elbow CHAPTER CONTENTS functions are flexion/extension, which is performed at the Joints and ligaments e91 humeroulnar and humeroradial joints, and pronation/supina- tion, which takes place at the upper radioulnar joint in close Joints. e91 association with the lower radioulnar joint. Ligaments . e92 The three joints work closely together and make pronation Biomechanical aspects e92 and supination movements possible whatever the extent of flexion or extension of the elbow: Flexion–extension . e93 Pronation–supination . e94 • The humeroulnar joint acts as a hinge. The articular surfaces on the humerus are the spool-shaped trochlea Muscles and tendons e94 with, proximal to it, the coronoid fossa (ventral aspect) Flexor muscles. e94 (see Gosling et al, Fig. 3.89) and the olecranon fossa Extensor muscles . e94 (dorsal aspect) (see Gosling et al, Fig. 3.90). The other Supinator muscles . e96 part of the joint is formed by the olecranon, with its trochlear notch and its olecranon (proximal) and coronoid Pronator muscles . e96 (distal) processes. Muscles controlling wrist movement . e98 • The humeroradial joint – a ball-and-socket joint – consists Nerves e99 of (a) the spheroidal capitulum of the humerus and Ulnar nerve. e99 (b) the proximal surface of the head of the radius. Median nerve . e99 Proximal to the capitulum lies the radial fossa and beside it a capitulotrochlear sulcus (between capitulum Medial cutaneous nerve of the forearm . e100 and trochlea). The articular facet of the radius, with Radial nerve . e100 which the proximal part of the humeroradial joint Bursae e101 articulates, is at the top of the head of the radius. -
Olecranon Fractures – a Case Based Approach to Understanding Management
Olecranon Fractures – A Case Based Approach to Understanding Management Jonathan M. Gross, MD Director of Orthopedic Trauma Staten Island University Hospital Core Curriculum V Introduction and Objectives • Design: Interactive Case Based • Objectives – Review pertinent bone and soft tissue anatomy to understand fracture patterns and associated instability – Review indications and strategies to stabilize fractures and restore stability – Provide pearls to help minimize risk of surgical complications and illustrate key points of management Core Curriculum V Elbow Anatomy • Three distinct joints – humeral(trochlea) – ulnar – humeral(capitellar) – radial – proximal radial-ulnar(PRUJ) Core Curriculum V Factors Responsible for Elbow Stability: Bony Anatomy • Normal muscle forces drive elbow posteriorly – Brachialis: base coronoid – Biceps: radial tuberosity • Boney restraints that Resist posteriorly directed forces: – Coronoid process – Radial Head Core CurriculumJMG 2020 V Factors Responsible for Elbow Stability: Bony Anatomy • Varus/Valgus – Radial Head – Trochlea – Medial coronoid facet Core Curriculum V Ligamentous structures responsible for static stability… Lateral view • Laterally –ulna collateral Annular ligament ligament • Medial – anterior bands Lateral collateral (LCL) of MCL Anterior bundle of MCL Medial view Annular ligament • Anteriorly – capsular Coronoid process tissues can be used to Anterior bundle of MCL JAAOS - Journal of the American Academyprovide of Orthopaedic to stability Surgeons16(9):519-529, September 2008. Posterior bundle of MCL Sublime tubercle Core Curriculum V Surgical Anatomy • Articular cartilage – Sigmoid notch of ulna: bare spot centrally between tip and coronoid – Pearl: Beware of narrowing sigmoid fossa when treating 30° comminuted olecranon fx’s. 2x • Coronoid process: preserve 1x height – Coronoid Height ~ 2 x Olecranon height – Tip of Coronoid to tip of Olecranon subtends angle of ~30 degrees from long axis of ulnar Beser, C.G. -

Chapter 6 the Elbow and Radioulnar Joints
The Elbow & Radioulnar Joints • Most upper extremity movements involve the elbow & radioulnar joints • Usually grouped together due to close Chapter 6 anatomical relationship The Elbow and Radioulnar Joints • Elbow joint movements may be clearly distinguished from those of the radioulnar joints Manual of Structural Kinesiology • Radioulnar joint movements may be R.T. Floyd, EdD, ATC, CSCS distinguished from those of the wrist © 2007 McGraw-Hill Higher Education. All rights reserved. 6-1 © 2007 McGraw-Hill Higher Education. All rights reserved. 6-2 Bones Bones • Ulna is much larger • Scapula, humerus, & ulna serve as proximally than radius proximal attachments for muscles that • Radius is much larger pronate & supinate the radioulnar joints distally than ulna • Distal attachments of radioulnar joint • Scapula & humerus serve as muscles are located on radius proximal attachments for muscles that flex & extend • Bony landmarks the elbow – medial condyloid ridge • Ulna & radius serve as distal – olecranon process attachments for these same – coranoid process muscles – radial tuberosity © 2007 McGraw-Hill Higher Education. All rights reserved. 6-3 © 2007 McGraw-Hill Higher Education. All rights reserved. 6-4 Bones Joints • Key bony landmarks • Ginglymus or hinge-type joint for wrist & hand • Allows only flexion & extension muscles • 2 interrelated joints – medial epicondyle – humeroulnar joint – lateral epicondyle – radiohumeral joints – lateral supracondylar ridge © 2007 McGraw-Hill Higher Education. All rights reserved. 6-5 © 2007 McGraw-Hill -

The Appendicular Skeleton 11 Bones of the Pectoral Girdle and Upper Extremity
ighapmLre11pg163_170 5/12/04 1:02 PM Page 163 impos03 302:bjighapmL:ighapmLrevshts:layouts: NAME ___________________________________ LAB TIME/DATE _______________________ REVIEW SHEET exercise The Appendicular Skeleton 11 Bones of the Pectoral Girdle and Upper Extremity 1. Match the bone names or markings in column B with the descriptions in column A. Column A Column B g; deltoid tuberosity 1. raised area on lateral surface of humerus to which deltoid muscle a. acromion attaches b. capitulum i; humerus 2. arm bone c. carpals d; clavicle, p; scapula 3. bones of the shoulder girdle d. clavicle o; radius, t; ulna 4. forearm bones e. coracoid process a; acromion 5. scapular region to which the clavicle connects f. coronoid fossa p; scapula 6. shoulder girdle bone that is unattached to the axial skeleton g. deltoid tuberosity d; clavicle 7. shoulder girdle bone that transmits forces from the upper limb to the bony thorax h. glenoid cavity h; glenoid cavity 8. depression in the scapula that articulates with the humerus i. humerus e; coracoid process 9. process above the glenoid cavity that permits muscle attachment j. metacarpals d; clavicle 10. the “collarbone” k. olecranon fossa s; trochlea 11. distal condyle of the humerus that articulates with the ulna l. olecranon process t; ulna 12. medial bone of forearm in anatomical position m. phalanges b; capitulum 13. rounded knob on the humerus; adjoins the radius n. radial tuberosity f; coronoid fossa 14. anterior depression, superior to the trochlea, which receives part of the o. radius ulna when the forearm is flexed p. scapula t; ulna 15.