B4754.Pdf (2.181Mb)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

National Knowledge Commission Report to the Nation 2007
dg Kkue~ Kkue~ Kku ±ò ±ò Kku k« H È O ±ò Kku dg Kkue~ Kkue~ Kku ±ò ±ò Kku dg Kkue~ Kkue~ Kku ±ò ±ò Kku k« H È O ±ò Kku dg Kkue~ Kkue~ Kku ±ò eÛk«Ú ¾HœÈä¢ Oã]¶ sÐ_ :±ò Kku Knowledge Kkue~ Kkue~ Kku ‹≈‰’≈∆ :±ò º°æfi»¢ :±ò Kku iëëÞ eÛk«Ú ¾HœÈä¢ Oã]¶ sÐ_ :±ò Kku Knowledge Kkue~ Kkue~Kku iëëÞ eÛk«Ú ¾HœÈä¢ Oã]¶ sÐ_ :±ò Kku Knowledge Kkue~ Kkue~ Kku ‹≈‰’≈∆ :±ò º°æfi»¢ :±ò Kku iëëÞ eÛk«Ú ¾HœÈä¢ Oã]¶ sÐ_ :±ò Kku Knowledge Kkue~ ‹≈‰’≈∆ :±ò º°æfi»¢ :±ò Kku iëëÞ eÛk«Ú ¾HœÈä¢ Oã]¶ sÐ_ :±ò Kku Knowledge Kkue~ Kkue~ Kku ‹≈‰’≈∆ :±ò º°æfi»¢ :±ò Kku iëëÞ eÛk«Ú ¾HœÈä¢ Oã]¶ sÐ_Kkue~ Kku ‹≈‰’≈∆ :±ò º°æfi»¢ :±ò Kku iëëÞ eÛk«Ú ¾HœÈä¢ Oã]¶ sÐ_ :±ò Kku Knowledge Kkue~ Kkue~ Kku ‹≈‰’≈∆ :±ò º°æfi»¢ :±ò Kku iëëÞ eÛk«Ú ¾HœÈä¢ u Knowledge Kkue~ Kkue~ Kku ‹≈‰’≈∆ :±ò º°æfi»¢ :±ò Kku iëëÞ eÛk«Ú ¾HœÈä¢ Oã]¶ sÐ_ :±ò Kku Knowledge Kkue~ Kkue~ Kku ‹≈‰’≈∆ :±ò º°æfi»¢Oã]¶ sÐ_ :±ò Kku Knowledge Kkue~ Kkue~ Kku ‹≈‰’≈∆ :±ò º°æfi»¢ :±ò Kku iëëÞ eÛk«Ú ¾HœÈä¢ Oã]¶ sÐ_ :±ò Kku Knowledge Kkue~ Kkue~ Kku ku iëëÞ eÛk«Ú ¾HœÈä¢ Oã]¶ sÐ_ :±ò Kku Knowledge Kkue~ Kkue~ Kku ‹≈‰’≈∆ :±ò º°æfi»¢ :±ò Kku iëëÞ eÛk«Ú ¾HœÈä¢ Oã]¶ sÐ_ :±ò Kku Knowledge Kkue~ ‹≈‰’≈∆ :±ò º°æfi»¢ :±ò Kku iëëÞ eÛk«Ú ¾HœÈä¢ Oã]¶ sÐ_ :±ò Kku Knowledge Kkue~ Kkue~ Kku ‹≈‰’≈∆ :±ò º°æfi»¢ :±ò Kku iëëÞ eÛk«Ú ¾HœÈä¢ Oã]¶ sÐ_ Kkue~ Kku ‹≈‰’≈∆ :±ò º°æfi»¢ :±ò Kku iëëÞ eÛk«Ú ¾HœÈä¢ Oã]¶ sÐ_ :±ò Kku Knowledge Kkue~ Kkue~ Kku ‹≈‰’≈∆ :±ò º°æfi»¢ :±ò Kku iëëÞ eÛk«Ú ¾HœÈä¢Kku Knowledge Kkue~ Kkue~ Kku ‹≈‰’≈∆ :±ò º°æfi»¢ :±ò Kku iëëÞ eÛk«Ú ¾HœÈä¢ Oã]¶ sÐ_ :±ò Kku Knowledge Kkue~ Kkue~ Kku ‹≈‰’≈∆ :±ò º°æ ¶ sÐ_ :±ò Kku Knowledge Kkue~ Kkue~ Kku ‹≈‰’≈∆ -

Part 05.Indd
PART MISCELLANEOUS 5 TOPICS Awards and Honours Y NATIONAL AWARDS NATIONAL COMMUNAL Mohd. Hanif Khan Shastri and the HARMONY AWARDS 2009 Center for Human Rights and Social (announced in January 2010) Welfare, Rajasthan MOORTI DEVI AWARD Union law Minister Verrappa Moily KOYA NATIONAL JOURNALISM A G Noorani and NDTV Group AWARD 2009 Editor Barkha Dutt. LAL BAHADUR SHASTRI Sunil Mittal AWARD 2009 KALINGA PRIZE (UNESCO’S) Renowned scientist Yash Pal jointly with Prof Trinh Xuan Thuan of Vietnam RAJIV GANDHI NATIONAL GAIL (India) for the large scale QUALITY AWARD manufacturing industries category OLOF PLAME PRIZE 2009 Carsten Jensen NAYUDAMMA AWARD 2009 V. K. Saraswat MALCOLM ADISESHIAH Dr C.P. Chandrasekhar of Centre AWARD 2009 for Economic Studies and Planning, School of Social Sciences, Jawaharlal Nehru University, New Delhi. INDU SHARMA KATHA SAMMAN Mr Mohan Rana and Mr Bhagwan AWARD 2009 Dass Morwal PHALKE RATAN AWARD 2009 Actor Manoj Kumar SHANTI SWARUP BHATNAGAR Charusita Chakravarti – IIT Delhi, AWARDS 2008-2009 Santosh G. Honavar – L.V. Prasad Eye Institute; S.K. Satheesh –Indian Institute of Science; Amitabh Joshi and Bhaskar Shah – Biological Science; Giridhar Madras and Jayant Ramaswamy Harsita – Eengineering Science; R. Gopakumar and A. Dhar- Physical Science; Narayanswamy Jayraman – Chemical Science, and Verapally Suresh – Mathematical Science. NATIONAL MINORITY RIGHTS MM Tirmizi, advocate – Gujarat AWARD 2009 High Court 55th Filmfare Awards Best Actor (Male) Amitabh Bachchan–Paa; (Female) Vidya Balan–Paa Best Film 3 Idiots; Best Director Rajkumar Hirani–3 Idiots; Best Story Abhijat Joshi, Rajkumar Hirani–3 Idiots Best Actor in a Supporting Role (Male) Boman Irani–3 Idiots; (Female) Kalki Koechlin–Dev D Best Screenplay Rajkumar Hirani, Vidhu Vinod Chopra, Abhijat Joshi–3 Idiots; Best Choreography Bosco-Caesar–Chor Bazaari Love Aaj Kal Best Dialogue Rajkumar Hirani, Vidhu Vinod Chopra–3 idiots Best Cinematography Rajeev Rai–Dev D Life- time Achievement Award Shashi Kapoor–Khayyam R D Burman Music Award Amit Tivedi. -
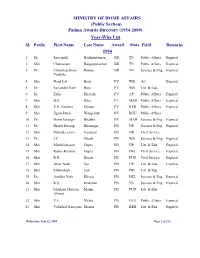
(Public Section) Padma Awards Directory (1954-2009) Year-Wise List Sl
MINISTRY OF HOME AFFAIRS (Public Section) Padma Awards Directory (1954-2009) Year-Wise List Sl. Prefix First Name Last Name Award State Field Remarks 1954 1 Dr. Sarvapalli Radhakrishnan BR TN Public Affairs Expired 2 Shri Chakravarti Rajagopalachari BR TN Public Affairs Expired 3 Dr. Chandrasekhara Raman BR TN Science & Eng. Expired Venkata 4 Shri Nand Lal Bose PV WB Art Expired 5 Dr. Satyendra Nath Bose PV WB Litt. & Edu. 6 Dr. Zakir Hussain PV AP Public Affairs Expired 7 Shri B.G. Kher PV MAH Public Affairs Expired 8 Shri V.K. Krishna Menon PV KER Public Affairs Expired 9 Shri Jigme Dorji Wangchuk PV BHU Public Affairs 10 Dr. Homi Jehangir Bhabha PB MAH Science & Eng. Expired 11 Dr. Shanti Swarup Bhatnagar PB UP Science & Eng. Expired 12 Shri Mahadeva Iyer Ganapati PB OR Civil Service 13 Dr. J.C. Ghosh PB WB Science & Eng. Expired 14 Shri Maithilisharan Gupta PB UP Litt. & Edu. Expired 15 Shri Radha Krishan Gupta PB DEL Civil Service Expired 16 Shri R.R. Handa PB PUN Civil Service Expired 17 Shri Amar Nath Jha PB UP Litt. & Edu. Expired 18 Shri Malihabadi Josh PB DEL Litt. & Edu. 19 Dr. Ajudhia Nath Khosla PB DEL Science & Eng. Expired 20 Shri K.S. Krishnan PB TN Science & Eng. Expired 21 Shri Moulana Hussain Madni PB PUN Litt. & Edu. Ahmed 22 Shri V.L. Mehta PB GUJ Public Affairs Expired 23 Shri Vallathol Narayana Menon PB KER Litt. & Edu. Expired Wednesday, July 22, 2009 Page 1 of 133 Sl. Prefix First Name Last Name Award State Field Remarks 24 Dr. -

Pravasi Bharatiya Divas 2013
Pravasi Bharatiya Divas 2013 Tag Line – Engaging Diaspora – The Indian Growth Story Sl. No. Sessions Topic Speakers 1. Plenary India’s Growth : Greater Shri Vayalar Ravi Minister of Overseas Indian India Session-I Opportunities Affairs 2. Dr. Montek Singh Deputy Chairman, Planning India Ahluwalia Commission 3. Shri Kamal Nath Minister of Urban India Development and Parliamentary Affairs 4. Shri Anand Sharma Minister of Commerce and India Industry 5. Shri P. K. Kunhalikutty Minister of Industries and India Information Technology 6. Shri K.M. Mani Minister of Finance, Law and India Housing, Government of Kerala 7. Ms. Naina Lal Kidwai President FICCI and Country India Head India, Director, HSBC Asia Pacific 8. Plenary Heritage and Diaspora Dr. Shashi Tharoor Minister of State for Human India Session-II Resource Development 9. Rt. Hon’ble Sir Anand Former Governor General, New Satyanand New Zealand Zealand 10. H.E. Dato Seri Dr S. Minister of Human Resource Malaysia Subramaniam 11. Hon’ble Jason Kenny, PC, Minister of Citizenship, Canada MP Immigration and Multiculturalism 12. Rt. Hon’ble Sandip Verma Parliamentary Under UK Secretary of State 13. Ms. Abike Dabiri Erewa Chairperson of the Nigerian Nigeria House of Representatives Committee 14. Shri Pavan K. Varma Author and former Bhutan Ambassador of India to Bhutan 15. Shri Gopinath Pillai Ambassador-at-Large, Singapore Singapore 16. Shri Ashook Ramsaran President, GOPIO International 17. Shri Yanktesh Permal Chairman, Reddy Group of Reddy Companies 18. Dr. Vidya Yeravdekar Director Symbiosis India International University, Pune 19. Shri Sant Singh Chatwal Chairman and CEO, Hampshire Hotels and Resorts 20. Plenary Engaging Young Overseas Shri Salman Khurshid Minister of External Affairs India 21. -
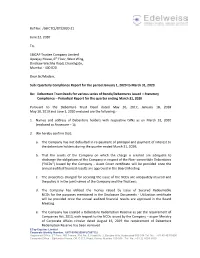
Ref No: /SBICTCL/DT/2020-21 June 22, 2020 To, SBICAP Trustee
Ref No: /SBICTCL/DT/2020-21 June 22, 2020 To, SBICAP Trustee Company Limited Apeejay House, 6th Floor, West Wing, Dinshaw Wachha Road, Churchgate, Mumbai - 400 020 Dear Sir/Madam, Sub: Quarterly Compliance Report for the period January 1, 2020 to March 31, 2020. Re: Debenture Trust Deeds for various series of Bonds/Debentures issued – Statutory Compliance – Periodical Report for the quarter ending March 31, 2020 Pursuant to the Debenture Trust Deed dated May 26, 2017, January 18, 2018 May 10, 2019 and June 1, 2020 enclosed are the following:- 1. Names and address of Debenture holders with respective ISINs as on March 31, 2020 (enclosed as Annexure – 1); 2. We hereby confirm that: a. The Company has not defaulted in re-payment of principal and payment of interest to the debenture holders during the quarter ended March 31, 2020; b. That the assets of the Company on which the charge is created are adequate to discharge the obligations of the Company in respect of the Non- convertible Debentures (“NCDs”) issued by the Company - Asset Cover certificate will be provided once the annual audited financial results are approved in the Board Meeting. c. The properties charged for securing the issue of the NCDs are adequately insured and the policy is in the joint names of the Company and the Trustees; d. The Company has utilized the money raised by issue of Secured Redeemable NCDs for the purposes mentioned in the Disclosure Documents - Utilization certificate will be provided once the annual audited financial results are approved in the Board Meeting. e. -

INLAND WATERWAYS AUTHORITY of INDIA A-13, Sector-1, Noida, U.P.-201 301 LIBRARY BOOK LIST Sr
INLAND WATERWAYS AUTHORITY OF INDIA A-13, Sector-1, Noida, U.P.-201 301 LIBRARY BOOK LIST Sr. Accession Name of the Book Author Edition Language Publication Pages No. No. No. 1 4385 Infrastructure at Haldea Gajenra 1 English Oxford 263 crossroads: challenges of University press governance 2 4386 Essential knowledge. Quiz Briens Derek 1 English Penguin Books 365 book. 3 4387 Sefety convention 2011: Rajpoot, R.N. 1 English The Institute of 195 sefety transportation Engineers 4 4389 To kill a mocking bird Lee, Harper 2010 English Arrow books 309 5 4390 Its kind of a funny story Vizzini, Ned 2007 English Micromax 444 6 4391 Memories of a teenege Zevin Gabrille. 2010 English Squir Fish. 284 amnesiac 7 4392 Bell jar. Plath, Sylvia 2005 English Fader and Fader 234 8 4393 The catcher in the rye. Salinger, J.D. 2010 English Penguin Books 192 9 4394 Paper towns. Green, John 2009 English Speak Penguin 305 Books 10 4395 Going bovine Bray, Libba 2009 English Ember. 480 11 4396 Lock and key. Dessen, Sarah. 2008 English Penguin groups 421 12 4397 The backbenchers. oberai, sidharth 2011 English Grapevine india 190 Pub. Pvt., Ltd. 13 4406 Illustrated guide to revised Ghosh, T.P. 2009 English Taxmann Pub. 526 schesule. VI Pvt. Ltd. 14 4412 CPWD quality assurance CPWD 2009 English CPWD 110 circulars 15 4413 Analysis of rates for Delhi. CPWD 2010 English Director, 582 General(works) CPWD Nirman Bhawan 16 4414 Analysis of rates for Delhi. Director General 2010 English Director, 660 (works) CPWD, General(works) Nirman Bhawan. CPWD Nirman Bhawan 17 4415 CPWD specification CPWD 2009 English Director, 532 General(works) CPWD Nirman Bhawan 18 4416 CPWD specification Director General 2009 English Director, 500 (works) CPWD General(works) Nirman Bhawan CPWD Nirman Bhawan 19 4417 Delhi schedule of rates- CPWD 2012 English Director, 432 2012 General(works) CPWD Nirman Bhawan 20 4418 Work manual. -
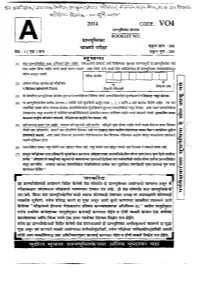
CODE: V04 Qpr Y
2014 CODE: V04 rrmgfiazm* * BOOKLET NO. dm 'qjvm : 100 - qpr y : 200 2 &jrmr / SPACE FOR ROUGH WORK 1. Which of the following elements increases the corrosion resistance of steel ? (1) Chromium and Nickel (2) Cobalt and Manganese (3) Aluminium (4) Zinc 2. flow thermo-electric projects generate electricity ? (1) by heating one junction of a thermo-couple (2) by cooling one junction of a thermo-couple (3) by heating or cooling one junction of a thermo-couple (4) none of these 3. Who formulated the science of diagnosis based on accurate description of the symptoms of various diseases ? (1) Robert Boyle (2) Aristottle (3) Hippocrates (4) None of these 4. Select the correct sentence : (1) Brass is an alloy of copper and iron. (2) Brass is an alloy of copper and zinc. (3) Brass is an alloy of copper and nickel. (4) Brass is an alloy of copper and tin. 5. Which of the following statements is correct ? (1) Magnetic lines of force start from south pole and end on north pole (2) No two magnetic lines of force can intersect each other. (3) Magnetic lines of force are crowded where magnetic field is weak. (4) Magnetic lines of force are far from each other where magnetic field is strong. SPACE FOR ROUGH WORK P.T.O. 6. Ultrasonic waves have been found very useful for dental cutting because (1) they made the cutting almost painless (2) they cut the hard material very easily (3) they do not require any mechanical device for cutting purpose (4) all of the above 7. -

Report 109 Commttee on Health and Family Welfare
REPORT NO. 109 PARLIAMENT OF INDIA RAJYA SABHA DEPARTMENT-RELATED PARLIAMENTARY STANDING COMMITTEE ON HEALTH AND FAMILY WELFARE ONE HUNDRED NINTH REPORT The National Medical Commission Bill, 2017 (Presented to the Rajya Sabha on20 th March, 2018 ) (Laid on the Table of Lok Sabha on20 th March, 2018 ) Rajya Sabha Secretariat, New Delhi March, 2018/Phalguna, 1939 (Saka) Website : http://rajyasabha.nic.in E-mail : [email protected] 117 Hindi version of this publication is also available PARLIAMENT OF INDIA RAJYA SABHA DEPARTMENT-RELATED PARLIAMENTARY STANDING COMMITTEE ON HEALTH AND FAMILY WELFARE ONE HUNDRED NINTH REPORT The National Medical Commission Bill, 2017 (Presented to the Rajya Sabha on 20th March, 2018) (Laid on the Table of Lok Sabha on 20th March, 2018) Rajya Sabha Secretariat, New Delhi March, 2018/ Phalguna, 1939 (Saka) CONTENTS PAGES 1. COMPOSITION OF THE COMMITTEE ....................................................................................... (i)-(ii) 2. INTRODUCTION ...................................................................................................................... (iii)-(iv) 3. ACRONYMS ............................................................................................................................ (v)-(vii) 4. REPORT ................................................................................................................................. 1-67 5. RECOMMENDATIONS/OBSERVATIONS — AT A GLANCE .......................................................... 68-82 6. MINUTES .............................................................................................................................. -

April 2021 Management Times
AIMA’S MONTHLY E-MAGAZINE AIMA | SNAPSHOTS | APRIL 2021 MANAGEMENT TIMES APRIL 2021 AIMA OFFICE BEARERS PRESIDENT Mr Harsh Pati Singhania Vice Chairman & Managing Director Dear Readers, It gives me great pleasure to present the next issue of AIMA News. JK Paper Ltd These past few weeks have proven to be very difficult for all of us, with the sudden rise in cases and compounding healthcare problems. It is a challenge we must all collectively face, while continuing to maintain social distancing with strict observance SENIOR VICE PRESIDENT of all necessary precautions. I wish good health and safety to all AIMA members, students, associates and their families. Mr C K Ranganathan On the work front, AIMA continued its endeavour to spread management thought Chairman & Managing Director despite the challenges of the prevailing conditions. CavinKare Pvt Ltd AIMA recently held its 6th National Leadership Conclave on the theme ‘The Big Disruption: Leadership in the post-Covid world’, on a specially curated digital platform. Dr S Jaishankar, Minister of External Affairs, Government of India, was the Guest of Honour on the occasion. Mr Sunil Kant Munjal, Chairman, Hero Enterprise and Mr Sanjiv VICE PRESIDENT Goneka, Chairman, RP Sanjiv Goenka Group were the Conclave Co-Chairs; while Mr Harsh Pati Singhania, President, AIMA & Vice Chairman & Managing Director, JK Paper Shrinivas V Dempo Ltd delivered the welcome address. Several other thought leaders and renowned experts also addressed the 2 day Conclave Chairman including Mr N Chandrasekaran, Chairman, Tata Sons; Mr Sanjiv Puri, Chairman and Dempo Group of Companies MD, ITC Ltd; Dr Shashi Tharoor, Member of Parliament (INC); Mr TV Narendran, CEO and MD, Tata Steel Ltd; Mr CK Ranganathan, Sr Vice President, AIMA & Chairman and MD, CavinKare Pvt Ltd; Dr Krishna Ella, Chairman & Managing Director, Bharat Biotech International Ltd; Mr Rakesh Jhunjhunwala, CEO, Rare Enterprises; Mr Shrinivas Dempo, IMMEDIATE PAST PRESIDENT Vice President, AIMA & Chairman, Dempo Group of Companies amongst many others. -

Report of the National Commission on Macroeconomics and Health Report of the National Commission on Macroeconomics and Health
Report of the National Commission on Macroeconomics and Health Report of the National Commission on Macroeconomics and Health Report of the National Commission on Macroeconomics and Health Report of the Report of the National Commission on Macroeconomics and Health Report of the National Commission on Macroeconomics and Health National Commission on Report of the Macroeconomics and Health National Commission on Macroeconomics and Health MINISTRY OF HEALTH AND FAMILY WELFARE GOVERNMENT OF INDIA, 2005 EQUITABLE DEVELOPMENT • HEALTHY FUTURE Report of the National Commission on Macroeconomics and Health National Commission on Macroeconomics and Health Ministry of Health & Family Welfare Government of India, New Delhi August 2005 © Ministry of Health & Family Welfare, Government of India September 2005 ISBN 81-7525-633-8 This Report does not address tertiary care and related areas such as super speciality hospital development in the public or private sector, telemedicine, medical tourism, environmental pollution or food safety etc. though they are all equally important. The Commission Report is based on background papers which can be accessed from the NCMH website www.mohfw.nic.in. They have also been published in two companion volumes. This report was written during the period April 1, 2004 - March 31, 2005. Printed at: Cirrus Graphics Private Limited B 261, Phase I, Naraina Industrial Area, New Delhi 110 028 Tel: + 91 11 51411507/1508 Fax: +91 11 51417575 email: [email protected] Editors: Pranay G. Lal and Byword Editorial Consultants Cover design: Quote Design Studio ii REPORT OF THE NATIONAL COMMISSION ON MACROECONOMICS AND HEALTH Members of the National Commission on Macroeconomics & Health Shri P. -

List of Fellows (Name-Wise) Upto 2016
LIST OF FELLOWS (NAME-WISE) UPTO 2016 0. Description Year 1. Abdul Kalam, A.P.J. Biomedical Engineering July 1995 DMIT. Former President, Republic of India. Res: 10 Rajaji Marg, New Delhi-110001. Permanent Address: No. 2, Mosque Street, Rameswaram, Ramanathapuram District, Tamil Nadu-623526. Tel: Off: (011) 3015321, 3014930, Res: (04567) 6493708, Fax: 2300756, E-mail: [email protected] (b 1931) (d.2015) Gen. Amir Chand Oration (NAMS, 1997-98) Padma Bhushan (1981); Padma Vibhushan (1990); Bharat Ratna (1997); D.Sc (h.c.) from several Universities; National Design Award; Dr. Biren Roy Space Award; Om Prakash Bhasin Award; National Nehru Award by Govt. of Madhya Pradesh; GM Modi Award for Science 1996; HK Firodia Award for Excellence in S&T 1996; Veer Savarkar Award 1998; Hon Fellow-Institution of Electronics and Telecommunication Engineers. 2. Abraham, Jacob Neurosurgery 1984 MS, MS (Neuro), FACS, FACA. Res: 10, 15th Avenue, Harrington Road, Chennai- 600031. Tel: Res: (044) 28363211, 42849258, Mobile: 09940118382, E-mail: [email protected] (b.1931). Basanti Devi Amir Chand Prize (ICMR, 1984); Sachs Memorial Lecturer, USA (1989). 3. Achari, Kamala Obstetrics and Gynecology 1982 MS, FRCOG, FICS, FACS. Emeritus Professor, Patna Medical College, Patna-800001 (Bihar). Res: 'Tirumalai', 21/D Road No.10, Rajendra Nagar, Patna- 800016. (b.1924) (d. 2014). 4. Adithan, C. Pharmacology July 2003 MD, PhD, FIMSA, FIPS. Former Professor & Head, Department of Pharmacology, Jawaharlal Institute of Postgraduate Medical Education & Research, Pondicherry- 605006. Currently: Director-CIDRF and Professor of Pharmacology, Mahatma Gandhi Medical College and Research Institute, Pondicherry-607403. Res: Flat No. 1, Srinivas Towers, Vazhudavour Road, Kathirkamam, Pondicherry-605009. -

Siyahi-Catalogue-2015-16.Pdf
Siyahi, in Urdu means ‘ink’, the dye that stains the shape of our thoughts. Tell us your story. And we’ll help you tell it to the world. Here at Siyahi, we’re with you right from the beginning. From assessing and editing the manuscript to finding the right publisher and promoting the book after publication, we stand firm by our authors through it all. While we deal primarily with manuscripts in English, we are actively involved in facilitating translation of books to and from various languages. We also organize literary events – everything from intimate readings to international literary festivals. RIGHTS LIST ALL RIGHTS AVAILABLE WORLD RIGHTS AVAILABLE LANGUAGE RIGHTS AVAILBLE AUTHORS FORTHCOMING PUBLISHED EVENTS TEAM RIGHTS LIST ALL RIGHTS AVAILABLE FICTION All Our Days by Keya Ghosh An Excess of Sanity by Anshumani Ruddra In Another Time by Keya Ghosh Indophrenia by Sudeep Chakravarti Men Without God by Meghna Pant Mohini’s Wedding by Selina Hossain (English Translation by Arunava Sinha) No More Tomorrows by Keya Ghosh Poskem by Wendell Rodricks The Ceaseless Chatter of Demons by Ashok Ferrey You Who Never Arrived by Anshumani Ruddra NON-FICTION Dream Catchers: Business Innovators of Bollywood by Priyanka Sinha Jha Dream Moghuls: Business Leaders of Bollywood by Priyanka Sinha Jha Folk Music and Musical Instruments of Punjab by Alka Pande Indian Street Food by Rocky Singh, Mayur Sharma Like Cotton from the Kapok Tree by Kalpana Mohan Managing Success...and Some Seriously Good Food by Rocky Singh, Mayur Sharma Magician in the Desert