Breech Baby Patient Information Leaflet
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Childbirth Education Booklet
Childbirth Education Contents Normal Discomforts of Pregnancy 2 Call Your Doctor 4 Late Pregnancy 5 Labor: Stage 1 6 Labor: Stages 2 & 3 8 Breastfeeding in the Hospital 9 Breathing Techniques 10 Birth Plans 10 Labor Positions 11 How Your Partner and Doula Can Help 13 Packing for the Hospital 15 Normal Discomforts of Pregnancy Fatigue Backache • Listen to your body, take naps, get extra rest • Maintain correct posture • Do pelvic tilt exercises while standing and on hands Stuffy Nose and knees • Warm compresses to nose • While on all fours, crawl forwards and backwards, • Cool mist humidifier in your home or rock, and do pelvic tilts bedroom at night • When picking up something lift with your legs to protect your back Shortness of Breath • Don’t stay that way, slow down and catch your breath • For prolonged standing, elevate 1 foot on a step stool • Sleep propped up with pillows or in recliner • Receive back massages • Maintain correct posture Dribble Urine • Moderate intensity exercising (walking, stationary • Do Kegel exercises – at least 50 a day bike, swim, flexibility moves) (do 10 every time you wash your hands) • How can you tell if you are dribbling urine or your Heartburn/Nausea water broke? Call your OB or midwife, and remember • Don’t eat 3 big meals a day, eat 5-6 smaller meals this acronym: • Drink 8 cups of water a day COAT. C=color, O=odor, A=amount, T=time. • Have dry crackers/cereal to nibble on–keep in purse and at bedside • Don’t let stomach become empty • Eat well balanced diet–vitamin B may help to decrease • Avoid -

The Effects of Alcohol in Newborns Efeitos Do Álcool No Recém-Nascido
REVIEW The effects of alcohol in newborns Efeitos do álcool no recém-nascido Maria dos Anjos Mesquita* ABSTRACT alcoólicas leva a prejuízos individuais, para a sua família e para The purpose of this article was to present a review of the effects toda a sociedade. Apesar disso, a dificuldade do seu diagnóstico e of alcohol consumption by pregnant mothers on their newborn. a inexperiência dos profissionais de saúde faz com que o espectro Definitions, prevalence, pathophysiology, clinical features, diagnostic dessas lesões seja pouco lembrado e até desconhecido. As lesões criteria, follow-up, treatment and prevention were discussed. A causadas pela ação do álcool no concepto são totalmente prevenidas search was performed in Medline, LILACS, and SciELO databases se a gestante não consumir bebidas alcoólicas durante a gestação. using the following terms: “fetus”, “newborn”, “pregnant woman”, Assim, é fundamental a detecção das mulheres consumidoras “alcohol”, “alcoholism”, “fetal alcohol syndrome”, and “alcohol- de álcool durante a gravidez e o desenvolvimento de programas related disorders”. Portuguese and English articles published from específicos de alerta sobre as consequências do álcool durante a 2000 to 2009 were reviewed. The effects of alcohol consumed by gestação e amamentação. pregnant women on newborns are extremely serious and occur frequently; it is a major issue in Public Health worldwide. Fetal alcohol Descritores: Bebidas alcoólicas/efeitos adversos; Feto; Recém-nascido; spectrum disorders cause harm to individuals, their families, and the Síndrome alcoólica fetal; Transtornos relacionados ao uso de álcool entire society. Nevertheless, diagnostic difficulties and inexperience of healthcare professionals result in such damage, being remembered rarely or even remaining uncovered. -

Care During Pregnancy and Delivery ACCESSIBLE, QUALITY HEALTH CARE DURING PREGNANCY and DELIVERY
Care during Pregnancy and Delivery ACCESSIBLE, QUALITY HEALTH CARE DURING PREGNANCY AND DELIVERY Why It’s Important Having a healthy pregnancy and access to quality birth facilities are the best ways to promote a healthy birth and have a thriving newborn. Getting early and regular prenatal care is vital. Prenatal care is the health care that women receive during their entire pregnancy. Prenatal care is more than doctor’s visits and ultrasounds; it is an opportunity to improve the overall well-being and health of the mom which directly affects the health of her baby. Prenatal visits give parents a chance to ask questions, discuss concerns, treat complications in a timely manner, and ensure that mom and baby are safe during pregnancy and delivery. Receiving quality prenatal care can have positive effects long after birth for both the mother and baby. When it is time for the mother to give birth, having access to safe, high quality birth facilities is critical. Early prenatal care, starting in the 1st trimester, is crucial to the health of mothers and babies. But more important than just initiating early prenatal care is receiving adequate prenatal care, having the appropriate number of prenatal care visits at the appropriate intervals throughout the pregnancy. Babies of mothers who do not get prenatal care are three times more likely to be born low birth weight and five times more likely to die than those born to mothers who do get care.1 In 2017 in Minnesota, only 77.1 percent of women received prenatal care within their first trimester of pregnancy. -
Turning Your Breech Baby to a Head-Down Position (External Cephalic Version)
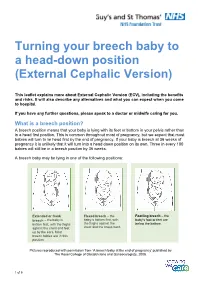
Turning your breech baby to a head-down position (External Cephalic Version) This leaflet explains more about External Cephalic Version (ECV), including the benefits and risks. It will also describe any alternatives and what you can expect when you come to hospital. If you have any further questions, please speak to a doctor or midwife caring for you. What is a breech position? A breech position means that your baby is lying with its feet or bottom in your pelvis rather than in a head first position. This is common throughout most of pregnancy, but we expect that most babies will turn to lie head first by the end of pregnancy. If your baby is breech at 36 weeks of pregnancy it is unlikely that it will turn into a head down position on its own. Three in every 100 babies will still be in a breech position by 36 weeks. A breech baby may be lying in one of the following positions: Extended or frank Flexed breech – the Footling breech – the breech – the baby is baby is bottom first, with baby’s foot or feet are bottom first, with the thighs the thighs against the below the bottom. against the chest and feet chest and the knees bent. up by the ears. Most breech babies are in this position. Pictures reproduced with permission from ‘A breech baby at the end of pregnancy’ published by The Royal College of Obstetricians and Gynaecologists, 2008. 1 of 5 What causes breech? Breech is more common in women who are expecting twins, or in women who have a differently-shaped womb (uterus). -

14. Management of Diabetes in Pregnancy: Standards of Medical
Diabetes Care Volume 42, Supplement 1, January 2019 S165 14. Management of Diabetes in American Diabetes Association Pregnancy: Standards of Medical Care in Diabetesd2019 Diabetes Care 2019;42(Suppl. 1):S165–S172 | https://doi.org/10.2337/dc19-S014 14. MANAGEMENT OF DIABETES IN PREGNANCY The American Diabetes Association (ADA) “Standards of Medical Care in Diabetes” includes ADA’s current clinical practice recommendations and is intended to provide the components of diabetes care, general treatment goals and guidelines, and tools to evaluate quality of care. Members of the ADA Professional Practice Committee, a multidisciplinary expert committee, are responsible for updating the Standards of Care annually, or more frequently as warranted. For a detailed description of ADA standards, statements, and reports, as well as the evidence-grading system for ADA’s clinical practice recommendations, please refer to the Standards of Care Introduction. Readers who wish to comment on the Standards of Care are invited to do so at professional.diabetes.org/SOC. DIABETES IN PREGNANCY The prevalence of diabetes in pregnancy has been increasing in the U.S. The majority is gestational diabetes mellitus (GDM) with the remainder primarily preexisting type 1 diabetes and type 2 diabetes. The rise in GDM and type 2 diabetes in parallel with obesity both in the U.S. and worldwide is of particular concern. Both type 1 diabetes and type 2 diabetes in pregnancy confer significantly greater maternal and fetal risk than GDM, with some differences according to type of diabetes. In general, specific risks of uncontrolled diabetes in pregnancy include spontaneous abortion, fetal anomalies, preeclampsia, fetal demise, macrosomia, neonatal hypoglycemia, and neonatal hyperbilirubinemia, among others. -

If You Are Pregnant: INFORMATION on FETAL DEVELOPMENT, ABORTION and ALTERNATIVES August 2019
If You Are Pregnant: INFORMATION ON FETAL DEVELOPMENT, ABORTION AND ALTERNATIVES August 2019 IF YOU ARE PREGNANT: INFORMATION ON FETAL DEVELOPMENT, ABORTION AND ALTERNATIVES If You Are Pregnant: Information on Fetal Development, Abortion and Alternatives Resources used by the Minnesota Department of Health for this publication are Human Embryology and Developmental Biology, Fifth Edition, 2014; Larsen’s Human Embryology, Fifth Edition, 2014; The Developing Human, 10th Edition, 2016; and In the Womb, 2006. The photographs in this booklet are credited to Lennart Nilsson/TT Images and are used by permission; except for week 38 copyright Minnesota Department of Health. The illustrations found throughout this booklet were created by Peg Gerrity, Houston, Texas. Copyright: http://www.peggerrity.com. Minnesota Department of Health Division of Child and Family Health PO Box 64882 St. Paul, MN 55164-0882 651-201-3580 Women's Right to Know (https://www.health.state.mn.us/people/wrtk/index.html) Upon request, this material will be made available in an alternative format such as large print, Braille or audio recording. Printed on recycled paper. 2 IF YOU ARE PREGNANT: INFORMATION ON FETAL DEVELOPMENT, ABORTION AND ALTERNATIVES Contents If You Are Pregnant: INFORMATION ON FETAL DEVELOPMENT, ABORTION AND ALTERNATIVES............................................................................................................................. 1 Introduction ............................................................................................................................... -

Vaginal Breech Birth Mary Olusile Lecturer in Practice
1 Vaginal Breech birth Mary Olusile Lecturer in Practice Breech: is where the fetal buttocks is the presenting part. Occurs in 15% of pregnancies at 28wks reducing to 3-4% at term Usually associated with: Uterine & pelvic anomalies - bicornuate uterus, lax uterus, fibroids and cysts Fetal anomalies - anencephaly, hydrocephaly, multiple gestation, oligohydraminous and polyhydraminous Cornually placed placenta (probably the commonest cause). Diagnosis: by abdominal examination or vaginal examination and confirmed by ultrasound scan Vaginal Breech VS. Caesarean Section Trial by Hannah et al (2001) found CS to produce better outcomes than vaginal breech but does acknowledge that may be due to lost skills of operators Therefore recommended mode of delivery is CS Limitations of trial by Hannah et al have since been highlighted questioning results and conclusion (Kotaska 2004) Now some advocates for vaginal breech birth when selection is based on clear prelabour and intrapartum criteria (Alarab et al 2004) Breech birth is u sually not an option except at clients choice Important considerations are size of fetus, presentation, attitude, size of maternal pelvis and parity of the woman NICE recommendation: External cephalic version (ECV) to be considered and offered if appropriate Produced by CETL 2007 2 Vaginal Breech birth Anterior posterior diameter of the pelvic brim is 11 cm Oblique diameter of the pelvic brim is 12 cm Transverse diameter of the pelvic brim is 13 cm Anterior posterior diameter of the outlet is 13 cm Produced by CETL 2007 3 -

Maternal Movement and Position Changes to Facilitate Labor Progress Have Been Discussed in the Literature for Decades
ELAINE ZWELLING, PHD, RN, LCCE, FACCE Abstract The benefi ts of maternal movement and position changes to facilitate labor progress have been discussed in the literature for decades. Recent routine interventions such as amniotomy, induction, fetal monitoring, and epidural anesthesia, as well as an increase in maternal obesity, have made position changes during labor challenging. The lack of maternal changes in position throughout labor can contribute to dystocia and increase the risk of cesarean births for failure to progress or descend. This article provides a historical review of the research fi ndings related to the effects of maternal positioning on the labor process and uses six physiological principles as a framework to offer sug- gestions for maternal positioning both before and after epidural anesthesia. Key Words Birth; Childbirth; Labor, fi rst stage; Labor, second stage; Maternity nursing; Obstetrical nursing; Maternal postures; Maternal positioning. Overcoming the Challenges: Maternal Movement 72 volume 35 | number 2 March/April 2010 or centuries laboring women chose to remain dural anesthesia, found that women who were able to mobile and upright, using positions such as change positions regularly or maintain upright positions standing, sitting, kneeling, hands and knees, or during labor were more comfortable and required less Fsquatting (Gupta & Nikodem, 2000; Johnson, pain medication (Atwood, 1976; de Jong et al., 1997; En- Johnson, & Gupta, 1991). Today immobility throughout gelmann, 1977; Johnson et al., 1991). For instance, Ada- the labor process has become a common occurrence for chi, Shimada, and Usul (2003) found in their study of 58 many childbearing women. Increased medical manage- laboring women that a sitting position decreased labor ment, obesity, lack of patient understanding about the pain in contrast with supine positioning. -

Variation in Fetal Presentations and Positions Among Women in Warri, Delta State, Nigeria
World Research Journal of Obstetrics and Gynecology ISSN: 2277-6001, Volume 2, Issue 1, 2013, pp.-10-12. Available online at http://www.bioinfopublication.org/jouarchive.php?opt=&jouid=BPJ0000126 VARIATION IN FETAL PRESENTATIONS AND POSITIONS AMONG WOMEN IN WARRI, DELTA STATE, NIGERIA OLANIYAN O.T.1*, MERAIYEBU A.B.1, ALELE J.Y.1, DARE J.B.2, ATSUKWEI D.1 AND ADELAIYE A.B.1 1Department of Physiology, Bingham University, Karu, Nasarawa, Nigeria. 2Department of Anatomy, Bingham University, Karu, Nasarawa, Nigeria. *Corresponding Author: Email- [email protected] Received: November 21, 2013; Accepted: December 23, 2013 Abstract- This study investigates the various fetal presentations among women in Warri and the various predisposing factors which may have possibly brought about these variations; the major positions considered were cephalic, breech and transverse, with the considered influencing factors being gestational age of the fetus, maternal age, amniotic fluid volume, parity, and method of previous deliveries. A total of 105 ultra- sound fetal biometries with a total of 108 fetuses, between 15-40 weeks of gestational age, and maternal age between 19 and 40 were used for this study. Fetal ultrasound biometry was used to find out information about the fetus including gestational age, amniotic fluid volume, presentation of the fetus and a questionnaire was used to take information about the mother including maternal age, parity, and method of previous delivery (ies). The result showed that a total of 82 fetuses (75.9%) were Cephalic babies, 19 (17.6%) were Breech and 7 (6.5%) are transverse. Out of the 105 women, there were 102 (77.1% cephalic, 18.3% breech, 4.8% transverse) women with adequate amniotic fluid volume and 1 woman (with a cephalic fetus) with average amniotic fluid volume and 2 women (with transverse foetuses) with low amniotic fluid volume. -

Pregnancy-Related Changes You Can Expect Before and After Baby Comes
Pregnancy-related changes you can expect before and after baby comes When you start sharing the news that you’re pregnant, everyBABY single mother you know will inevitably bombard you with opinions, stories and advice on what to do NEWBEAUTY.COM during the nine months of constant change. While the well-meaning do really mean well, not every mom-to- be will experience the same concerns. To sort through 150 the stockpile of information, we asked experts to share their tips on how to keep skin happy through each trimester, and what to do when it’s not. SPRING 2021 SPRING ON BOARDby Tatiana Bido VICTOR DYOMIN/GETTY IMAGES, IMAGE USED FOR ILLUSTRATIVE PURPOSES ONLY ONLY PURPOSES ILLUSTRATIVE FOR USED IMAGE IMAGES, DYOMIN/GETTY VICTOR Maternity vs. Nursing Glow Recipe Bras Turns out, the often talked about “pregnancy glow” is real. “Due to excess sebum production from glandular tissue and increased blood volume, skin swells and Breast changes start happening many women experience what is known as a pregnancy glow,” explains New pretty early on—around six to eight York gynecologist Dr. Monica Grover. However, many women also experience weeks—and many moms-to-be find uncomfortable pregnancy-related skin changes as early as the first trimester, that they outgrow their everyday while others don’t until their second or third. “This is why it’s so important to bras very quickly. Normal weight use skin-care products that are clean and clinical because they will support gain and an expanding rib cage are the most common pregnancy-related skin issues and have the highest-quality to blame for the first set of changes, standards and be made in a sterile environment with the most carefully followed by expanding mammary sourced ingredients,” advises master aesthetician Abigail Zsenai. -

OB/GYN – Childbirth/Labor/Delivery Protocol 6 - 2
Section SECTION: Obstetrical and Gynecological Emergencies REVISED: 06/2015 6 1. Physiologic Changes with Pregnancy Protocol 6 - 1 2. OB/GYN – Childbirth/Labor/Delivery Protocol 6 - 2 3. Medical – Newborn/Neonatal Protocol 6 - 3 OB / GYN Resuscitation 4. OB/GYN – Pregnancy Related Protocol 6 - 4 Emergencies (Delivery – Shoulder Dystocia) 5. OB/GYN – Pregnancy Related Protocol 6 - 5 Emergencies (Delivery – Breech Presentation) 6. OB/GYN – Pregnancy Related Protocol 6 - 6 Emergencies (Ectopic Pregnancy/Rupture) 7. OB/GYN – Pregnancy Related Protocol 6 - 7 EMERGENCIES Emergencies (Abruptio Placenta) 8. OB/GYN – Pregnancy Related Protocol 6 - 8 Emergencies (Placenta Previa) 9. OB/GYN – Pregnancy Related Protocol 6 - 9 Emergencies (Umbilical Cord Prolapse) 10. OB/GYN - Eclampsia Protocol 6 - 10 (Hypertension/Eclampsia/HELLPS) 11. OB/GYN – Pregnancy Related Protocol 6 - 11 Emergencies (Premature Rupture of Membranes (PROM)) 12. OB/GYN - Pre-term Labor Protocol 6 - 12 (Pre-term Labor) 13. OB/GYN – Post-partum Hemorrhage Protocol 6 - 13 Created, Developed, and Produced by the Old Dominion EMS Alliance Section 6 Continued This page intentionally left blank. OB / GYN EMERGENCIES Created, Developed, and Produced by the Old Dominion EMS Alliance Protocol SECTION: Obstetrical/Gynecological Emergencies PROTOCOL TITLE: Physiologic Changes with Pregnancy 6-1 REVISED: 06/2017 OVERVIEW: Many changes occur in the pregnant woman’s body, starting from the time of conception and throughout the pregnancy. The most obvious body system to undergo change is the reproductive system, but all of the others will change as well. Brief summaries of the physiologic changes that occur during pregnancy have been listed by system. Most of these physiologic changes will resolve during the postpartum period. -

Psycho-Socio-Cultural Risk Factors for Breech Presentation Caroline Peterson University of South Florida
University of South Florida Scholar Commons Graduate Theses and Dissertations Graduate School 7-2-2008 Psycho-Socio-Cultural Risk Factors for Breech Presentation Caroline Peterson University of South Florida Follow this and additional works at: https://scholarcommons.usf.edu/etd Part of the American Studies Commons Scholar Commons Citation Peterson, Caroline, "Psycho-Socio-Cultural Risk Factors for Breech Presentation" (2008). Graduate Theses and Dissertations. https://scholarcommons.usf.edu/etd/451 This Dissertation is brought to you for free and open access by the Graduate School at Scholar Commons. It has been accepted for inclusion in Graduate Theses and Dissertations by an authorized administrator of Scholar Commons. For more information, please contact [email protected]. Psycho-Socio-Cultural Risk Factors for Breech Presentation by Caroline Peterson A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy Department of Anthropology College of Arts and Science University of South Florida Major Professor: Lorena Madrigal, Ph.D. Wendy Nembhard, Ph.D. Nancy Romero-Daza, Ph.D. David Himmelgreen, Ph.D. Getchew Dagne, Ph.D. Date of Approval: July 2, 2008 Keywords: Maternal Fetal Attachment, Evolution, Developmental Plasticity, Logistic Regression, Personality © Copyright 2008, Caroline Peterson Dedication This dissertation is dedicated to all the moms who long for answers about their babys‟ presentation and to the babies who do their best to get here. Acknowledgments A big thank you to the following folks who made this dissertation possible: Jeffrey Roth who convinced ACHA to let me use their Medicaid data then linked it with the birth registry data. David Darr who persuaded the Florida DOH to let me use the birth registry data for free.