Role of the PTPRD Locus and Limited Pleiotropy with Other Neuropathologies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Interactome of KRAB Zinc Finger Proteins Reveals the Evolutionary History of Their Functional Diversification
Resource The interactome of KRAB zinc finger proteins reveals the evolutionary history of their functional diversification Pierre-Yves Helleboid1,†, Moritz Heusel2,†, Julien Duc1, Cécile Piot1, Christian W Thorball1, Andrea Coluccio1, Julien Pontis1, Michaël Imbeault1, Priscilla Turelli1, Ruedi Aebersold2,3,* & Didier Trono1,** Abstract years ago (MYA) (Imbeault et al, 2017). Their products harbor an N-terminal KRAB (Kru¨ppel-associated box) domain related to that of Krüppel-associated box (KRAB)-containing zinc finger proteins Meisetz (a.k.a. PRDM9), a protein that originated prior to the diver- (KZFPs) are encoded in the hundreds by the genomes of higher gence of chordates and echinoderms, and a C-terminal array of zinc vertebrates, and many act with the heterochromatin-inducing fingers (ZNF) with sequence-specific DNA-binding potential (Urru- KAP1 as repressors of transposable elements (TEs) during early tia, 2003; Birtle & Ponting, 2006; Imbeault et al, 2017). KZFP genes embryogenesis. Yet, their widespread expression in adult tissues multiplied by gene and segment duplication to count today more and enrichment at other genetic loci indicate additional roles. than 350 and 700 representatives in the human and mouse Here, we characterized the protein interactome of 101 of the ~350 genomes, respectively (Urrutia, 2003; Kauzlaric et al, 2017). A human KZFPs. Consistent with their targeting of TEs, most KZFPs majority of human KZFPs including all primate-restricted family conserved up to placental mammals essentially recruit KAP1 and members target sequences derived from TEs, that is, DNA trans- associated effectors. In contrast, a subset of more ancient KZFPs posons, ERVs (endogenous retroviruses), LINEs, SINEs (long and rather interacts with factors related to functions such as genome short interspersed nuclear elements, respectively), or SVAs (SINE- architecture or RNA processing. -
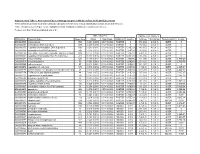
Association of Gene Ontology Categories with Decay Rate for Hepg2 Experiments These Tables Show Details for All Gene Ontology Categories
Supplementary Table 1: Association of Gene Ontology Categories with Decay Rate for HepG2 Experiments These tables show details for all Gene Ontology categories. Inferences for manual classification scheme shown at the bottom. Those categories used in Figure 1A are highlighted in bold. Standard Deviations are shown in parentheses. P-values less than 1E-20 are indicated with a "0". Rate r (hour^-1) Half-life < 2hr. Decay % GO Number Category Name Probe Sets Group Non-Group Distribution p-value In-Group Non-Group Representation p-value GO:0006350 transcription 1523 0.221 (0.009) 0.127 (0.002) FASTER 0 13.1 (0.4) 4.5 (0.1) OVER 0 GO:0006351 transcription, DNA-dependent 1498 0.220 (0.009) 0.127 (0.002) FASTER 0 13.0 (0.4) 4.5 (0.1) OVER 0 GO:0006355 regulation of transcription, DNA-dependent 1163 0.230 (0.011) 0.128 (0.002) FASTER 5.00E-21 14.2 (0.5) 4.6 (0.1) OVER 0 GO:0006366 transcription from Pol II promoter 845 0.225 (0.012) 0.130 (0.002) FASTER 1.88E-14 13.0 (0.5) 4.8 (0.1) OVER 0 GO:0006139 nucleobase, nucleoside, nucleotide and nucleic acid metabolism3004 0.173 (0.006) 0.127 (0.002) FASTER 1.28E-12 8.4 (0.2) 4.5 (0.1) OVER 0 GO:0006357 regulation of transcription from Pol II promoter 487 0.231 (0.016) 0.132 (0.002) FASTER 6.05E-10 13.5 (0.6) 4.9 (0.1) OVER 0 GO:0008283 cell proliferation 625 0.189 (0.014) 0.132 (0.002) FASTER 1.95E-05 10.1 (0.6) 5.0 (0.1) OVER 1.50E-20 GO:0006513 monoubiquitination 36 0.305 (0.049) 0.134 (0.002) FASTER 2.69E-04 25.4 (4.4) 5.1 (0.1) OVER 2.04E-06 GO:0007050 cell cycle arrest 57 0.311 (0.054) 0.133 (0.002) -

Genetic Interactions Between ANLN and KDR Are Prognostic for Breast Cancer Survival
ONCOLOGY REPORTS 42: 2255-2266, 2019 Genetic interactions between ANLN and KDR are prognostic for breast cancer survival XIAOFENG DAI1*, XIAO CHEN2*, OLIVIER HAKIZIMANA2 and YI MEI2 1Wuxi School of Medicine, 2School of Biotechnology, Jiangnan University, Wuxi, Jiangsu 214122, P.R. China Received April 3, 2019; Accepted August 7, 2019 DOI: 10.3892/or.2019.7332 Abstract. Single nucleotide polymorphisms (SNPs) are the of ~627,000 annually estimated in 2018 (2). Uncontrolled most common genetic variation in mammalian cells with proliferative growth and angiogenesis are two basic cancer prognostic potential. Anillin-actin binding protein (ANLN) hallmarks governing the critical transitions towards malig- has been identified as being involved in PI3K/PTEN signaling, nancy during carcinogenesis (3). PI3K/PTEN signaling, which is critical in cell life/death control, and kinase insert frequently altered in breast carcinoma (4), confers a survival domain receptor (KDR) encodes a key receptor mediating advantage to tumor cells (5). Anillin, encoded by anillin the cancer angiogenesis/metastasis switch. Knowledge of actin-binding protein (ANLN), is an actin-binding protein, the intrinsic connections between PI3K/PTEN and KDR which has been identified as being involved in the PI3K/PTEN signaling, which represent two critical transitions in carcino- pathway (6,7). It is an F‑actin binding protein, which maintains genesis, led the present study to investigate the effects of the podocyte cytoskeletal dynamics, cell motility and signaling potential synergy between ANLN and KDR on breast cancer through its interaction with CD2-associated protein, which outcome and identify relevant SNPs driving such a synergy stimulates the phosphorylation of AKT at serine 473 (6,8). -
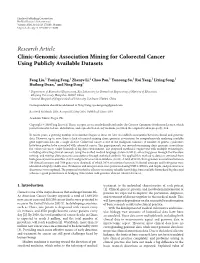
Research Article Clinic-Genomic Association Mining for Colorectal Cancer Using Publicly Available Datasets
Hindawi Publishing Corporation BioMed Research International Volume 2014, Article ID 170289, 10 pages http://dx.doi.org/10.1155/2014/170289 Research Article Clinic-Genomic Association Mining for Colorectal Cancer Using Publicly Available Datasets Fang Liu,1 Yaning Feng,1 Zhenye Li,2 Chao Pan,1 Yuncong Su,1 Rui Yang,1 Liying Song,1 Huilong Duan,1 and Ning Deng1 1 Department of Biomedical Engineering, Key Laboratory for Biomedical Engineering of Ministry of Education, Zhejiang University, Hangzhou 310027, China 2 General Hospital of Ningxia Medical University, Yinchuan 750004, China Correspondence should be addressed to Ning Deng; [email protected] Received 30 March 2014; Accepted 12 May 2014; Published 2 June 2014 Academic Editor: Degui Zhi Copyright © 2014 Fang Liu et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. In recent years, a growing number of researchers began to focus on how to establish associations between clinical and genomic data. However, up to now, there is lack of research mining clinic-genomic associations by comprehensively analysing available gene expression data for a single disease. Colorectal cancer is one of the malignant tumours. A number of genetic syndromes have been proven to be associated with colorectal cancer. This paper presents our research on mining clinic-genomic associations for colorectal cancer under biomedical big data environment. The proposed method is engineered with multiple technologies, including extracting clinical concepts using the unified medical language system (UMLS), extracting genes through the literature mining, and mining clinic-genomic associations through statistical analysis. -

Immunomic Analysis of Human Renal Cell Carcinoma
Immunomic analysis of human renal cell carcinoma Zur Erlangung des akademischen Grades eines DOKTORS DER NATURWISSENSCHAFTEN (Dr. rer. nat.) der Fakultät für Chemie und Biowissenschaften der Universität Karlsruhe (TH) vorgelegte DISSERTATION von Gerard Devitt aus Cork, Irland Dekan: Prof. Dr. Manfred Kappes Referent: Prof. Dr. Margot Zöller Korreferent: Prof. Dr. Jonathan Sleeman Tag der mündlichen Prüfung: 19th July 2004 For James, Roseanne, Niall, Owen and Nadia Zusammenfassung - 3 – Das Nierenzellkarzinom ist der am häufigsten in den Nieren vorkommende Tumor. Er macht bis zu 3% aller malignen Erkrankungen bei Erwachsenen aus. Die Zahl der Nierenzellkarzinompatienten steigt jährlich. Bisher gibt es keine international standardisierte Therapie für das metastasierende Nierenzellkarzinom und die vollständige Entfernung der betroffenen Niere ist zur Zeit die einzige Behandlungsmöglichkeit. Das Nierenzellkarzinom ist sehr resistent gegen Bestrahlung und Chemotherapie, zeigt aber in manchen Untersuchungen eine spontane Regression, die auf Immunogenität des Tumors schließen lässt. Die Identifikation von nierenzellkarzinomassoziierten immunogenen Molekülen ist daher wichtig, um 1.) die grundlegenden Mechanismen der Immunogenität des Nierenzellkarzinoms zu verstehen, 2.) für mögliche neue Ansätze in Diagnose, Prognose und Therapie. In dieser Arbeit wurden drei Techniken eingesetzt, um nierenzellkarzinomassoziierte Gene und Antigene zu erkennen: 1) Suppression substractive hybridization (SSH), 2) Serological analysis of recombinant cDNA expression -

The DNA Sequence and Comparative Analysis of Human Chromosome 20
articles The DNA sequence and comparative analysis of human chromosome 20 P. Deloukas, L. H. Matthews, J. Ashurst, J. Burton, J. G. R. Gilbert, M. Jones, G. Stavrides, J. P. Almeida, A. K. Babbage, C. L. Bagguley, J. Bailey, K. F. Barlow, K. N. Bates, L. M. Beard, D. M. Beare, O. P. Beasley, C. P. Bird, S. E. Blakey, A. M. Bridgeman, A. J. Brown, D. Buck, W. Burrill, A. P. Butler, C. Carder, N. P. Carter, J. C. Chapman, M. Clamp, G. Clark, L. N. Clark, S. Y. Clark, C. M. Clee, S. Clegg, V. E. Cobley, R. E. Collier, R. Connor, N. R. Corby, A. Coulson, G. J. Coville, R. Deadman, P. Dhami, M. Dunn, A. G. Ellington, J. A. Frankland, A. Fraser, L. French, P. Garner, D. V. Grafham, C. Grif®ths, M. N. D. Grif®ths, R. Gwilliam, R. E. Hall, S. Hammond, J. L. Harley, P. D. Heath, S. Ho, J. L. Holden, P. J. Howden, E. Huckle, A. R. Hunt, S. E. Hunt, K. Jekosch, C. M. Johnson, D. Johnson, M. P. Kay, A. M. Kimberley, A. King, A. Knights, G. K. Laird, S. Lawlor, M. H. Lehvaslaiho, M. Leversha, C. Lloyd, D. M. Lloyd, J. D. Lovell, V. L. Marsh, S. L. Martin, L. J. McConnachie, K. McLay, A. A. McMurray, S. Milne, D. Mistry, M. J. F. Moore, J. C. Mullikin, T. Nickerson, K. Oliver, A. Parker, R. Patel, T. A. V. Pearce, A. I. Peck, B. J. C. T. Phillimore, S. R. Prathalingam, R. W. Plumb, H. Ramsay, C. M. -

Evolutionary Analysis of Viral Sequences in Eukaryotic Genomes
Evolutionary analysis of viral sequences in eukaryotic genomes Sean Schneider A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy University of Washington 2014 Reading Committee: James H. Thomas, Chair Willie Swanson Phil Green Program Authorized to Offer Degree: Genome Sciences ©Copyright 2014 Sean Schneider University of Washington Abstract Evolutionary analysis of viral sequences in eukaryotic genomes Sean Schneider Chair of the supervisory committee: Professor James H. Thomas Genome Sciences The focus of this work is several evolutionary analyses of endogenous viral sequences in eukaryotic genomes. Endogenous viral sequences can provide key insights into the past forms and evolutionary history of viruses, as well as the responses of host organisms they infect. In this work I have examined viral sequences in a diverse assortment of eukaryotic hosts in order to study coevolution between hosts and the organisms that infect them. This research consisted of two major lines of investigation. In the first portion of this work, I outline the hypothesis that the C2H2 zinc finger gene family in vertebrates has evolved by birth-death evolution in response to sporadic retroviral infection. The hypothesis suggests an evolutionary model in which newly duplicated zinc finger genes are retained by selection in response to retroviral infection. This hypothesis is supported by a strong association (R2=0.67) between the number of endogenous retroviruses and the number of zinc fingers in diverse vertebrate genomes. Based on this and other evidence, the zinc finger gene family appears to act as a “genomic immune system” against retroviral infections. The other major line of investigation in this work examines endogenous virus sequences utilized by parasitic wasps to disable hosts that they infect. -

Identification of Potential Core Genes in Sevoflurance Induced Myocardial
Identication of Potential core genes in Sevourance induced Myocardial Energy Metabolism in Patients Undergoing Off-pump Coronary Artery Bypass Graft Surgery using Bioinformatics analysis Hua Lin ( [email protected] ) Tianjin Medical University General Hospital Airport Site Research article Keywords: sevourane, Myocardial Energy Metabolism, Off-pump Coronary Artery Bypass Graft Surgery Posted Date: November 18th, 2019 DOI: https://doi.org/10.21203/rs.2.17434/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/15 Abstract Background: Myocardial ischemia-reperfusion injury always happened after Off-pump coronary artery bypass graft(OPCABG), and this can not be avoided altogether. In this study, we tried to detect potential genes of sevourane-induced myocardial energy metabolism in patients undergoing OPCABG using bioinformatics analysis. Methods: We download and analyze the gene expression prole data from the Gene Expression Omnibus(GEO) database using bioinformatics methods. We downloded the gene expression data from the Gene Expression Omnibus(GEO) database using bioinformatics methods. Gene Ontology(GO) functional annotation analysis and Kyoto Encyclopedia of Genes and Genomes(KEGG) pathway enrichment analysis were used to analysis the screened differentially expressed genes(DEGs). Then, we established a protein–protein interaction (PPI) network to nd hub genes associated with myocardial energy metabolism. Results: Through PPI network, we nd ten hub genes, including JUN, EGR1, ATF3, FOSB, JUNB, DUSP1, EGR2, NR4A1, BTG2, NR4A2. Conclusions: In conclusion, the proteins encoded by EGR1ATF3c-FosBtg2JunBDUSP1NR4A1BTG2 and NR4A2 were related to cardiac function. ATF3, FOSB, JUNB, DUSP1, NR4A1, NR4A2 are related to apoptosis of cardiomyocytes. The protein encoded by BTG2 is related to hypertrophy. -

UNIVERSITY of CALIFORNIA Los Angeles Identification of a Multisubunit E3 Ubiquitin Ligase Required for Heterotrimeric G-Protein
UNIVERSITY OF CALIFORNIA Los Angeles Identification of a multisubunit E3 ubiquitin ligase required for heterotrimeric G-protein beta-subunit ubiquitination and cAMP signaling A dissertation submitted in partial satisfaction of the requirements for the degree Doctor of Philosophy in Molecular Biology by Brian Daniel Young 2018 © Copyright by Brian Daniel Young 2018 ABSTRACT OF THE DISSERTATION Identification of a multisubunit E3 ubiquitin ligase required for heterotrimeric G-protein beta-subunit ubiquitination and cAMP signaling by Brian Daniel Young Doctor of Philosophy in Molecular Biology University of California, Los Angeles, 2018 Professor James Akira Wohlschlegel, Chair GPCRs are stimulated by extracellular ligands and initiate a range of intracellular signaling events through heterotrimeric G-proteins. Upon activation, G-protein α- subunits (Gα) and the stable βγ-subunit dimer (Gβγ) bind and alter the activity of diverse effectors. These signaling events are fundamental and subject to multiple layers of regulation. In this study, we used an unbiased proteomic mass spectrometry approach to uncover novel regulators of Gβγ. We identified a subfamily of potassium channel tetramerization domain (KCTD) proteins that specifically bind Gβγ. Several KCTD proteins are substrate adaptor proteins for CUL3–RING E3 ubiquitin ligases. Our studies revealed that a KCTD2-KCTD5 hetero-oligomer associates with CUL3 through KCTD5 subunits and recruits Gβγ through both subunits. Using in vitro ubiquitination reactions, we demonstrated that these KCTD proteins promote monoubiquitination of lysine-23 within Gβ1/2. This ubiquitin modification of Gβ1/2 is also observed in human ii cells and is dependent on these substrate adaptor proteins. Because these KCTD proteins bind Gβγ in response to G-protein activation, we investigated their role in GPCR signaling. -

Expression, Purification and Molecular Analysis of the Human ZNF706
Colombo et al. Biological Procedures Online 2013, 15:10 http://www.biologicalproceduresonline.com/content/15/1/10 Biological Procedures Online RESEARCH Open Access Expression, purification and molecular analysis of the human ZNF706 protein Jucimara Colombo1†, Paola Jocelan Scarin Provazzi1†, Marilia Freitas Calmon1, Lilian Campos Pires1, Nathália Campos Rodrigues2, Paulo Petl Jr1, Marcelo Andrés Fossey3, Fátima Pereira de Souza3, Fernanda Canduri2 and Paula Rahal1* Abstract Background: The ZNF706 gene encodes a protein that belongs to the zinc finger family of proteins and was found to be highly expressed in laryngeal cancer, making the structure and function of ZNF706 worthy of investigation. In this study, we expressed and purified recombinant human ZNF706 that was suitable for structural analysis in Escherichia coli BL21(DH3). Findings: ZNF706 mRNA was extracted from a larynx tissue sample, and cDNA was ligated into a cloning vector using the TOPO method. ZNF706 protein was expressed according to the E. coli expression system procedures and was purified using a nickel-affinity column. The structural qualities of recombinant ZNF706 and quantification alpha, beta sheet, and other structures were obtained by spectroscopy of circular dichroism. ZNF706's structural modeling showed that it is composed of α-helices (28.3%), β-strands (19.4%), and turns (20.9%), in agreement with the spectral data from the dichroism analysis. Conclusions: We used circular dichroism and molecular modeling to examine the structure of ZNF706. The results suggest that human recombinant ZNF706 keeps its secondary structures and is appropriate for functional and structural studies. The method of expressing ZNF706 protein used in this study can be used to direct various functional and structural studies that will contribute to the understanding of its function as well as its relationship with other biological molecules and its putative role in carcinogenesis. -

Downloaded from Ensembl
UCSF UC San Francisco Electronic Theses and Dissertations Title Detecting genetic similarity between complex human traits by exploring their common molecular mechanism Permalink https://escholarship.org/uc/item/1k40s443 Author Gu, Jialiang Publication Date 2019 Peer reviewed|Thesis/dissertation eScholarship.org Powered by the California Digital Library University of California by Submitted in partial satisfaction of the requirements for degree of in in the GRADUATE DIVISION of the UNIVERSITY OF CALIFORNIA, SAN FRANCISCO AND UNIVERSITY OF CALIFORNIA, BERKELEY Approved: ______________________________________________________________________________ Chair ______________________________________________________________________________ ______________________________________________________________________________ ______________________________________________________________________________ ______________________________________________________________________________ Committee Members ii Acknowledgement This project would not have been possible without Prof. Dr. Hao Li, Dr. Jiashun Zheng and Dr. Chris Fuller at the University of California, San Francisco (UCSF) and Caribou Bioscience. The Li lab grew into a multi-facet research group consist of both experimentalists and computational biologists covering three research areas including cellular/molecular mechanism of ageing, genetic determinants of complex human traits and structure, function, evolution of gene regulatory network. Labs like these are the pillar of global success and reputation -

Autocrine IFN Signaling Inducing Profibrotic Fibroblast Responses By
Downloaded from http://www.jimmunol.org/ by guest on September 23, 2021 Inducing is online at: average * The Journal of Immunology , 11 of which you can access for free at: 2013; 191:2956-2966; Prepublished online 16 from submission to initial decision 4 weeks from acceptance to publication August 2013; doi: 10.4049/jimmunol.1300376 http://www.jimmunol.org/content/191/6/2956 A Synthetic TLR3 Ligand Mitigates Profibrotic Fibroblast Responses by Autocrine IFN Signaling Feng Fang, Kohtaro Ooka, Xiaoyong Sun, Ruchi Shah, Swati Bhattacharyya, Jun Wei and John Varga J Immunol cites 49 articles Submit online. Every submission reviewed by practicing scientists ? is published twice each month by Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts http://jimmunol.org/subscription Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html http://www.jimmunol.org/content/suppl/2013/08/20/jimmunol.130037 6.DC1 This article http://www.jimmunol.org/content/191/6/2956.full#ref-list-1 Information about subscribing to The JI No Triage! Fast Publication! Rapid Reviews! 30 days* Why • • • Material References Permissions Email Alerts Subscription Supplementary The Journal of Immunology The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2013 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. This information is current as of September 23, 2021. The Journal of Immunology A Synthetic TLR3 Ligand Mitigates Profibrotic Fibroblast Responses by Inducing Autocrine IFN Signaling Feng Fang,* Kohtaro Ooka,* Xiaoyong Sun,† Ruchi Shah,* Swati Bhattacharyya,* Jun Wei,* and John Varga* Activation of TLR3 by exogenous microbial ligands or endogenous injury-associated ligands leads to production of type I IFN.