The Efficacy and Long-Term Outcome of Microcoil Embolotherapy For
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Spontaneous Hemothorax Caused by a Ruptured Intercostal Artery Aneurysm in Von Recklinghausen’S Neurofibromatosis
W.C. Chang, H.H. Hsu, H. Chang, et al BRIEF COMMUNICATION SPONTANEOUS HEMOTHORAX CAUSED BY A RUPTURED INTERCOSTAL ARTERY ANEURYSM IN VON RECKLINGHAUSEN’S NEUROFIBROMATOSIS Wei-Chou Chang,1 Hsian-He Hsu,1 Hung Chang,2 and Cheng-Yu Chen1 Abstract: Aneurysms arising from an intercostal artery are very rare vascular malformations in von Recklinghausen’s neurofibromatosis, which often have a silent clinical presentation and are difficult to diagnose before rupture. We report a case of von Recklinghausen’s neurofibromatosis with massive hemothroax caused by spontaneous rupture of an intercostal artery aneurysm in a 29-year-old man. The diagnosis was eventually confirmed by percutaneous angiography and treated with endovascular embolization. During a 10-month follow-up period, the patient had a satisfactory recovery. This case illustrates that angiography and possible endovascular embolization should be the first strategy in managing hemothorax in patients with von Recklinghausen’s disease. Key words: Aneurysm, ruptured; Embolization, therapeutic; Hemothorax; Neurofibromatosis 1; Thoracic arteries J Formos Med Assoc 2005;104:286-9 Von Recklinghausen’s neurofibromatosis, also named neurofibromatosis type 1 (NF-1), is a well-recognized Case Report entity that is characterized by numerous neuro- fibromas, spots of abnormal cutaneous pigmentation, A 29-year-old man presented at the emergency room and a variety of other dysplastic abnormalities of with sudden onset shortness of breath and severe the skin, nervous system, bones, endocrine organs and retrosternal pain radiating to his back. One week prior blood vessels.1,2 Vascular abnormalities in patients to admission, dull discomfort upon breathing was with NF-1 have been described for large, medium- noted, which was not affected by position or physical sized and small muscular arteries in the intracranial, activity. -
Urinary System
OUTLINE 27.1 General Structure and Functions of the Urinary System 818 27.2 Kidneys 820 27 27.2a Gross and Sectional Anatomy of the Kidney 820 27.2b Blood Supply to the Kidney 821 27.2c Nephrons 824 27.2d How Tubular Fluid Becomes Urine 828 27.2e Juxtaglomerular Apparatus 828 Urinary 27.2f Innervation of the Kidney 828 27.3 Urinary Tract 829 27.3a Ureters 829 27.3b Urinary Bladder 830 System 27.3c Urethra 833 27.4 Aging and the Urinary System 834 27.5 Development of the Urinary System 835 27.5a Kidney and Ureter Development 835 27.5b Urinary Bladder and Urethra Development 835 MODULE 13: URINARY SYSTEM mck78097_ch27_817-841.indd 817 2/25/11 2:24 PM 818 Chapter Twenty-Seven Urinary System n the course of carrying out their specific functions, the cells Besides removing waste products from the bloodstream, the uri- I of all body systems produce waste products, and these waste nary system performs many other functions, including the following: products end up in the bloodstream. In this case, the bloodstream is ■ Storage of urine. Urine is produced continuously, but analogous to a river that supplies drinking water to a nearby town. it would be quite inconvenient if we were constantly The river water may become polluted with sediment, animal waste, excreting urine. The urinary bladder is an expandable, and motorboat fuel—but the town has a water treatment plant that muscular sac that can store as much as 1 liter of urine. removes these waste products and makes the water safe to drink. -
The Urinary System Dr
The urinary System Dr. Ali Ebneshahidi Functions of the Urinary System • Excretion – removal of waste material from the blood plasma and the disposal of this waste in the urine. • Elimination – removal of waste from other organ systems - from digestive system – undigested food, water, salt, ions, and drugs. + - from respiratory system – CO2,H , water, toxins. - from skin – water, NaCl, nitrogenous wastes (urea , uric acid, ammonia, creatinine). • Water balance -- kidney tubules regulate water reabsorption and urine concentration. • regulation of PH, volume, and composition of body fluids. • production of Erythropoietin for hematopoieseis, and renin for blood pressure regulation. Anatomy of the Urinary System Gross anatomy: • kidneys – a pair of bean – shaped organs located retroperitoneally, responsible for blood filtering and urine formation. • Renal capsule – a layer of fibrous connective tissue covering the kidneys. • Renal cortex – outer region of the kidneys where most nephrons is located. • Renal medulla – inner region of the kidneys where some nephrons is located, also where urine is collected to be excreted outward. • Renal calyx – duct – like sections of renal medulla for collecting urine from nephrons and direct urine into renal pelvis. • Renal pyramid – connective tissues in the renal medulla binding various structures together. • Renal pelvis – central urine collecting area of renal medulla. • Hilum (or hilus) – concave notch of kidneys where renal artery, renal vein, urethra, nerves, and lymphatic vessels converge. • Ureter – a tubule that transport urine (mainly by peristalsis) from the kidney to the urinary bladder. • Urinary bladder – a spherical storage organ that contains up to 400 ml of urine. • Urethra – a tubule that excretes urine out of the urinary bladder to the outside, through the urethral orifice. -
![L8-Urine Conc. [PDF]](https://docslib.b-cdn.net/cover/4402/l8-urine-conc-pdf-1384402.webp)
L8-Urine Conc. [PDF]
The loop of Henle is referred to as countercurrent multiplier and vasa recta as countercurrent exchange systems in concentrating and diluting urine. Explain what happens to osmolarity of tubular fluid in the various segments of the loop of Henle when concentrated urine is being produced. Explain the factors that determine the ability of loop of Henle to make a concentrated medullary gradient. Differentiate between water diuresis and osmotic diuresis. Appreciate clinical correlates of diabetes mellitus and diabetes insipidus. Fluid intake The total body water Antidiuretic hormone is controled by : Renal excretion of water Hyperosmolar medullary Changes in the osmolarity of tubular fluid : interstitium 1 2 3 Low osmolarity The osmolarity High osmolarity because of active decrease as it goes up because of the transport of Na+ and because of the reabsorbation of water co-transport of K+ and reabsorption of NaCl Cl- 4 5 Low osmolarity because of High osmolarity because of reabsorption of NaCl , also reabsorption of water in reabsorption of water in present of ADH , present of ADH reabsorption of urea Mechanisms responsible for creation of hyperosmolar medulla: Active Co- Facilitated diffusion transport : transport : diffusion : of : Na+ ions out of the Only of small thick portion of the K+ , Cl- and other amounts of water ascending limb of ions out of the thick from the medullary the loop of henle portion of the Of urea from the tubules into the into the medullary ascending limb of inner medullary medullary interstitium the loop of henle collecting -
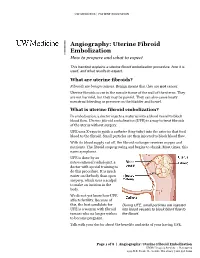
Uterine Fibroid Embolization Procedure, How It Is Used, and What Results to Expect
UW MEDICINE | PATIENT EDUCATION | | Angiography: Uterine Fibroid | Embolization | How to prepare and what to expect This handout explains a uterine fibroid embolization procedure, how it is used, and what results to expect. What are uterine fibroids? Fibroids are benign tumors. Benign means that they are not cancer. Uterine fibroids occur in the muscle tissue of the wall of the uterus. They are not harmful, but they may be painful. They can also cause heavy menstrual bleeding or pressure on the bladder and bowel. What is uterine fibroid embolization? In embolization, a doctor injects a material into a blood vessel to block blood flow. Uterine fibroid embolization (UFE) is a way to treat fibroids DRAFTof the uterus without surgery. UFE uses X-rays to guide a catheter (tiny tube) into the arteries that feed blood to the fibroid. Small particles are then injected to block blood flow. With its blood supply cut off, the fibroid no longer receives oxygen and nutrients. The fibroid stops growing and begins to shrink. Most times, this eases symptoms. UFE is done by an interventional radiologist, a doctor with special training to do this procedure. It is much easier on the body than open surgery, which uses a scalpel to make an incision in the body. We do not yet know how UFE affects fertility. Because of this, the best candidate for During UFE, small particles are injected UFE is a woman with fibroid into blood vessels to block blood flow to tumors who no longer wishes the fibroid. to become pregnant. Talk with your doctor about the benefits and risks of your having UFE. -

Embolization of Brain Aneurysms and Arteriovenous
Embolization of Brain Aneurysms and Arteriovenous Malformations/Fistulas Embolization of brain aneurysms and arteriovenous malformations (AVM) uses imaging guidance to place small, soft metal coils into an aneurysm to block the flow of blood and prevent the aneurysm from rupturing. It also is used to fill AVMs – abnormal connections between arteries and veins – with liquid embolic agents (similar to fast-sealing glue). AVMs may prevent oxygenated blood from completely circulating throughout the brain and can cause a variety of problems, including headache, weakness, and other neurological symptoms. Embolization treats cerebral aneurysms and AVMs previously thought inoperable and is much less invasive than open surgery. Your doctor will instruct you on how to prepare, including any changes to your medication schedule. Tell your doctor if there's a possibility you are pregnant and discuss any recent illnesses, medical conditions, allergies and medications you're taking, including herbal supplements and aspirin. You may be advised to stop taking aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs) or blood thinners several days prior to your procedure. You also may be told not to eat or drink anything after midnight before your procedure. Plan to stay at the hospital overnight. Leave jewelry at home and wear loose, comfortable clothing. You will be asked to wear a gown. What is Embolization of Brain Aneurysms and Fistulas? Embolization of brain aneurysms and arteriovenous malformations (AVM)/fistulas is a minimally invasive treatment for aneurysms and other blood vessel malformations that occur in the brain. These problems are typically identified in adults; however, aneurysms and AVMs can also occur in children. -

The Distal Convoluted Tubule and Collecting Duct
Chapter 23 *Lecture PowerPoint The Urinary System *See separate FlexArt PowerPoint slides for all figures and tables preinserted into PowerPoint without notes. Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Introduction • Urinary system rids the body of waste products. • The urinary system is closely associated with the reproductive system – Shared embryonic development and adult anatomical relationship – Collectively called the urogenital (UG) system 23-2 Functions of the Urinary System • Expected Learning Outcomes – Name and locate the organs of the urinary system. – List several functions of the kidneys in addition to urine formation. – Name the major nitrogenous wastes and identify their sources. – Define excretion and identify the systems that excrete wastes. 23-3 Functions of the Urinary System Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Diaphragm 11th and 12th ribs Adrenal gland Renal artery Renal vein Kidney Vertebra L2 Aorta Inferior vena cava Ureter Urinary bladder Urethra Figure 23.1a,b (a) Anterior view (b) Posterior view • Urinary system consists of six organs: two kidneys, two ureters, urinary bladder, and urethra 23-4 Functions of the Kidneys • Filters blood plasma, separates waste from useful chemicals, returns useful substances to blood, eliminates wastes • Regulate blood volume and pressure by eliminating or conserving water • Regulate the osmolarity of the body fluids by controlling the relative amounts of water and solutes -

Pulmonary Embolism A-Nd Thrombosis R
Postgrad Med J: first published as 10.1136/pgmj.38.435.13 on 1 January 1962. Downloaded from POSTGRAD MED. J. (I962), 38, 13 PULMONARY EMBOLISM A-ND THROMBOSIS R. MARSHALL, M.D., M.R.C.P. Nuffield Department of Surgery, Radcliffe Infirmary, Oxford SUDDEN death following a call for a bedpan is a chest pain and ECG changes when the balloon classical mode of presentation of pulmonary em- was inflated in a smaller artery (Brofman, Charms, bolism, but it is probable that cases of this severity Kohn, Elder, Newman and Rizika, I957). On the form only a small proportion of the total. Pul- other hand, it is a common practice to impact the monary embolism may be caused by blood clot, tip of a cardiac catheter in branches of the pul- fat, cells or foreign bodies, but most commonly by monary artery of about 2 mm. diameter with no blood clot. ill effects. In spite of the undoubted ability of emboli to produce reflex effects under certain cir- cumstances, there is a growing body of evidence The Physiological Effects that the effects of pulmonary embolism by inert The physiological effects ofpulmonary embolism particles are produced by the magnitude of the depend upon the size and number of the emboli mechanical blockage of the pulmonary vessels and and they may produce these effects either by are not dependent upon the size of the emboli or mechanical blockage of the circulation when they reflex vasoconstriction (Daley, I957; McEvoy, are of sufficient size or number, or by the initiation Harder and Dale, 1958; Williams, 1956). -

Guidelines for the Use of Echocardiography in the Evaluation of a Cardiac Source of Embolism
ASE GUIDELINES AND STANDARDS Guidelines for the Use of Echocardiography in the Evaluation of a Cardiac Source of Embolism Muhamed Saric, MD, PhD, FASE, Chair, Alicia C. Armour, MA, BS, RDCS, FASE, M. Samir Arnaout, MD, Farooq A. Chaudhry, MD, FASE, Richard A. Grimm, DO, FASE, Itzhak Kronzon, MD, FASE, Bruce F. Landeck, II, MD, FASE, Kameswari Maganti, MD, FASE, Hector I. Michelena, MD, FASE, and Kirsten Tolstrup, MD, FASE, New York, New York; Durham, North Carolina; Beirut, Lebanon; Cleveland, Ohio; Aurora, Colorado; Chicago, Illinois; Rochester, Minnesota; and Albuquerque, New Mexico Embolism from the heart or the thoracic aorta often leads to clinically significant morbidity and mortality due to transient ischemic attack, stroke or occlusion of peripheral arteries. Transthoracic and transesophageal echo- cardiography are the key diagnostic modalities for evaluation, diagnosis, and management of stroke, systemic and pulmonary embolism. This document provides comprehensive American Society of Echocardiography guidelines on the use of echocardiography for evaluation of cardiac sources of embolism. It describes general mechanisms of stroke and systemic embolism; the specific role of cardiac and aortic sour- ces in stroke, and systemic and pulmonary embolism; the role of echocardiography in evaluation, diagnosis, and management of cardiac and aortic sources of emboli including the incremental value of contrast and 3D echocardiography; and a brief description of alternative imaging techniques and their role in the evaluation of cardiac sources of emboli. Specific guidelines are provided for each category of embolic sources including the left atrium and left atrial appendage, left ventricle, heart valves, cardiac tumors, and thoracic aorta. In addition, there are recommen- dation regarding pulmonary embolism, and embolism related to cardiovascular surgery and percutaneous procedures. -
Introduction to the Urinary System
Tips for Success 1. Show up 2. Participate in lab 3. Show up 4. Turn in assignments (completed, refer to #6) 5. Show up 6. Communicate with me, e-mail is best 7. Show up Every point counts! Business Homework due in lab Label the handout provided today Front and back Use your book! There should be at least 18 items labeled Part 1 Urinary System Wastes Gases versus fluids Urinary system Dispose of water soluble wastes Electrolyte regulation Acid-base regulation Urinary System Other functions Kidneys Renin Erythropoietin Vitamin D activation Nitrogenous Wastes Urine is about 95% water Second largest component is urea Urea derived from breakdown of amino acids Nitrogenous Wastes TOXIC! + 1. Dietary amino acids → NH2 removed → NH2 + H → NH3 500 ml of urine removes only 1 gram of nitrogen as ammonia 2. Ammonia can be converted to urea Requires energy 50 ml of urine removes 1 gram of nitrogen as urea 3. Ammonia can be converted to uric acid Requires lots of energy 10 ml of urine removes 1 gram of nitrogen as uric acid Urinary System Organs Kidneys Major excretory organs Urinary bladder Temporary storage reservoir for urine Ureters Transport urine from the kidneys to the bladder Urethra Transports urine out of the body Hepatic veins (cut) Esophagus (cut) Inferior vena cava Renal artery Adrenal gland Renal hilum Aorta Renal vein Kidney Iliac crest Ureter Rectum (cut) Uterus (part of female reproductive Urinary system) bladder Urethra Figure 25.1 Kidney: Urinary System page 6 Anterior Inferior vena cava Peritoneal -
Guidelines for Peripheral and Visceral Vascular Embolization Training
Guidelines for Peripheral and Visceral Vascular Embolization Training Joint Writing Groups of the Standards of Practice Committees for the Society of Interventional Radiology (SIR), Cardiovascular and Interventional Radiological Society of Europe (CIRSE), and Canadian Interventional Radiology Association (CIRA) Jafar Golzarian, MD, Marc R. Sapoval, MD, PhD, Sanjoy Kundu, MD, David W. Hunter, MD, Elias N. Brountzos, MD, Jean-Francois H. Geschwind, MD, Timothy P. Murphy, MD, James B. Spies, MD, Michael J. Wallace, MD, Thierry de Baere, MD, and John F. Cardella, MD J Vasc Interv Radiol 2010; 21:436–441 EMBOLOTHERAPY or embolization 1. Vascular malformations: occlusion 3. Trauma: for control of dramatic hem- has rapidly developed in recent years of congenital or acquired aneu- orrhage, for example, related to and now represents an integral part of rysms (cerebral, visceral, extremi- splenic laceration or pelvic fractures. interventional radiology practice. Em- ties), pseudoaneurysms, vascular 4. Uterine artery embolization: devascu- bolotherapy is defined as the percuta- malformations, or other vascular larization of benign uterine leiomyo- neous endovascular application of one abnormalities that have potential mas and adenomyosis for symptom or more of a variety of agents or ma- to cause adverse health effects (1–18). alleviation or to reduce operative terials to accomplish vascular occlu- 2. Nontraumatic hemorrhage: treat- blood loss (3,4,14,54–57). sion. ment of acute or recurrent hem- 5. Oncologic embolization: to relieve Embolotherapy has evolved since its orrhage (eg, hemoptysis, gastro- symptoms, prevent or treat hem- clinical introduction to include a wide intestinal bleeding, postpartum orrhage, reduce operative blood loss, or improve survival and variety of applications that can be and iatrogenic hemorrhage, and quality of life (3,4,14,54–57). -

Endovascular Interventional Radiology of the Urogenital Tract
medicina Review Endovascular Interventional Radiology of the Urogenital Tract Fabio Pozzi Mucelli 1,*, Roberta A. Pozzi Mucelli 1, Cristina Marrocchio 2, Saverio Tollot 2 and Maria A. Cova 2 1 Department of Radiology, ASUGI, Ospedale di Cattinara, 34149 Trieste, Italy; [email protected] 2 Department of Radiology, University of Trieste, ASUGI, Ospedale di Cattinara, 34149 Trieste, Italy; [email protected] (C.M.); [email protected] (S.T.); [email protected] (M.A.C.) * Correspondence: [email protected] Abstract: Interventional radiology of the male urogenital system includes percutaneous and en- dovascular procedures, and these last consist mostly of transcatheter arterial embolizations. At the kidney level, arterial embolizations are performed mainly for palliative treatment of parenchymal tumors, for renal traumas and, less frequently, for arteriovenous fistulas and renal aneurysms and pseudoaneurysms. These latter may often require emergency intervention as they can cause renal or peri-renal hematomas or significant hematuria. Transcatheter arterial embolization is also an effective therapy for intractable severe bladder hematuria secondary to a number of neoplastic and inflammatory conditions in the pelvis, including unresectable bladder cancer and radiation-induced or cyclophosphamide-induced hemorrhagic cystitis. Endovascular interventional procedures for the penis are indicated for the treatment of post-traumatic priapism. In this article, we review the main endovascular radiological interventions of the male urogenital system, describing the technical aspects, results, and complications of each procedure at the various anatomical districts. Citation: Pozzi Mucelli, F.; Pozzi Keywords: embolization; angiography; urogenital system; kidney; bladder; priapism Mucelli, R.A.; Marrocchio, C.; Tollot, S.; Cova, M.A.