Infection: a Cause of and Cure for Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Picture of the Month
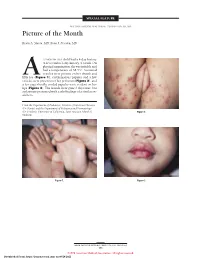
SPECIAL FEATURE SECTION EDITOR: WALTER W. TUNNESSEN, JR, MD Picture of the Month Kevin A. Slavin, MD; Ilona J. Frieden, MD 15-MONTH-OLD child had a 4-day history of fever and a 1-day history of a rash. On physical examination she was irritable and had a temperature of 38.3°C. Scattered vesicles were present on her thumb and Afifth toe (Figure 1), erythematous papules and a few vesicles were present over her perineum (Figure 2), and a few superficially eroded papules were evident on her lips (Figure 3). The lesions were gone 3 days later, but a playmate presented with early findings of a similar ex- anthem. From the Department of Pediatrics, Division of Infectious Diseases (Dr Slavin) and the Department of Pediatrics and Dermatology (Dr Frieden), University of California, San Francisco School of Figure 2. Medicine. Figure 1. Figure 3. ARCH PEDIATR ADOLESC MED/ VOL 152, MAY 1998 505 ©1998 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 09/28/2021 Denouement and Discussion Hand-Foot-and-Mouth Disease Figure 1. Vesicles are present on the thumb and fifth toe. foot-and-mouth disease).1,2,5-9 The lesions on the but- tocks are of the same size and typical of the early forms Figure 2. Multiple erythematous papules and a few scattered vesicles are of the exanthem, but they are not frequently vesicular present over the perineum. in nature. Lesions involving the perineum seem to be more Figure 3. Superficially eroded papules are present on the lips. common in children who wear diapers, suggesting that friction or minor trauma may play a role in the develop- ment of lesions. -

Identification of an Overprinting Gene in Merkel Cell Polyomavirus Provides Evolutionary Insight Into the Birth of Viral Genes
Identification of an overprinting gene in Merkel cell polyomavirus provides evolutionary insight into the birth of viral genes Joseph J. Cartera,b,1,2, Matthew D. Daughertyc,1, Xiaojie Qia, Anjali Bheda-Malgea,3, Gregory C. Wipfa, Kristin Robinsona, Ann Romana, Harmit S. Malikc,d, and Denise A. Gallowaya,b,2 Divisions of aHuman Biology, bPublic Health Sciences, and cBasic Sciences and dHoward Hughes Medical Institute, Fred Hutchinson Cancer Research Center, Seattle, WA 98109 Edited by Peter M. Howley, Harvard Medical School, Boston, MA, and approved June 17, 2013 (received for review February 24, 2013) Many viruses use overprinting (alternate reading frame utiliza- mammals and birds (7, 8). Polyomaviruses leverage alternative tion) as a means to increase protein diversity in genomes severely splicing of the early region (ER) of the genome to generate pro- constrained by size. However, the evolutionary steps that facili- tein diversity, including the large and small T antigens (LT and ST, tate the de novo generation of a novel protein within an ancestral respectively) and the middle T antigen (MT) of murine poly- ORF have remained poorly characterized. Here, we describe the omavirus (MPyV), which is generated by a novel splicing event and identification of an overprinting gene, expressed from an Alter- overprinting of the second exon of LT. Some polyomaviruses can nate frame of the Large T Open reading frame (ALTO) in the early drive tumorigenicity, and gene products from the ER, especially region of Merkel cell polyomavirus (MCPyV), the causative agent SV40 LT and MPyV MT, have been extraordinarily useful models of most Merkel cell carcinomas. -

書 名 等 発行年 出版社 受賞年 備考 N1 Ueber Das Zustandekommen Der
書 名 等 発行年 出版社 受賞年 備考 Ueber das Zustandekommen der Diphtherie-immunitat und der Tetanus-Immunitat bei thieren / Emil Adolf N1 1890 Georg thieme 1901 von Behring N2 Diphtherie und tetanus immunitaet / Emil Adolf von Behring und Kitasato 19-- [Akitomo Matsuki] 1901 Malarial fever its cause, prevention and treatment containing full details for the use of travellers, University press of N3 1902 1902 sportsmen, soldiers, and residents in malarious places / by Ronald Ross liverpool Ueber die Anwendung von concentrirten chemischen Lichtstrahlen in der Medicin / von Prof. Dr. Niels N4 1899 F.C.W.Vogel 1903 Ryberg Finsen Mit 4 Abbildungen und 2 Tafeln Twenty-five years of objective study of the higher nervous activity (behaviour) of animals / Ivan N5 Petrovitch Pavlov ; translated and edited by W. Horsley Gantt ; with the collaboration of G. Volborth ; and c1928 International Publishing 1904 an introduction by Walter B. Cannon Conditioned reflexes : an investigation of the physiological activity of the cerebral cortex / by Ivan Oxford University N6 1927 1904 Petrovitch Pavlov ; translated and edited by G.V. Anrep Press N7 Die Ätiologie und die Bekämpfung der Tuberkulose / Robert Koch ; eingeleitet von M. Kirchner 1912 J.A.Barth 1905 N8 Neue Darstellung vom histologischen Bau des Centralnervensystems / von Santiago Ramón y Cajal 1893 Veit 1906 Traité des fiévres palustres : avec la description des microbes du paludisme / par Charles Louis Alphonse N9 1884 Octave Doin 1907 Laveran N10 Embryologie des Scorpions / von Ilya Ilyich Mechnikov 1870 Wilhelm Engelmann 1908 Immunität bei Infektionskrankheiten / Ilya Ilyich Mechnikov ; einzig autorisierte übersetzung von Julius N11 1902 Gustav Fischer 1908 Meyer Die experimentelle Chemotherapie der Spirillosen : Syphilis, Rückfallfieber, Hühnerspirillose, Frambösie / N12 1910 J.Springer 1908 von Paul Ehrlich und S. -

Hand, Foot, and Mouth Disease (Coxsackievirus) Fact Sheet
Hand, Foot, and Mouth Disease (Coxsackievirus) Fact Sheet Hand, foot, and mouth disease is caused by one of several types of viruses Hand, foot, and mouth disease is usually characterized by tiny blisters on the inside of the mouth and the palms of the hands, fingers, soles of the feet. It is commonly caused by coxsackievirus A16 (an enterovirus), and less often by other types of viruses. Anyone can get hand, foot, and mouth disease Young children are primarily affected, but it may be seen in adults. Most cases occur in the summer and early fall. Outbreaks may occur among groups of children especially in child care centers or nursery schools. Symptoms usually appear 3 to 5 days after exposure. Hand, foot, and mouth disease is usually spread through person-to-person contact People can spread the disease when they are shedding the virus in their feces. It is also spread by the respiratory tract from mouth or respiratory secretions (such as from saliva on hands or toys). The virus has also been found in the fluid from the skin blisters. The infection is spread most easily during the acute phase/stage of illness when people are feeling ill, but the virus can be spread for several weeks after the onset of infection. The symptoms are much like a common cold with a rash The rash appears as blisters or ulcers in the mouth, on the inner cheeks, gums, sides of the tongue, and as bumps or blisters on the hands, feet, and sometimes other parts of the skin. The skin rash may last for 7 to 10 days. -

The Use of Non-Human Primates in Research in Primates Non-Human of Use The
The use of non-human primates in research The use of non-human primates in research A working group report chaired by Sir David Weatherall FRS FMedSci Report sponsored by: Academy of Medical Sciences Medical Research Council The Royal Society Wellcome Trust 10 Carlton House Terrace 20 Park Crescent 6-9 Carlton House Terrace 215 Euston Road London, SW1Y 5AH London, W1B 1AL London, SW1Y 5AG London, NW1 2BE December 2006 December Tel: +44(0)20 7969 5288 Tel: +44(0)20 7636 5422 Tel: +44(0)20 7451 2590 Tel: +44(0)20 7611 8888 Fax: +44(0)20 7969 5298 Fax: +44(0)20 7436 6179 Fax: +44(0)20 7451 2692 Fax: +44(0)20 7611 8545 Email: E-mail: E-mail: E-mail: [email protected] [email protected] [email protected] [email protected] Web: www.acmedsci.ac.uk Web: www.mrc.ac.uk Web: www.royalsoc.ac.uk Web: www.wellcome.ac.uk December 2006 The use of non-human primates in research A working group report chaired by Sir David Weatheall FRS FMedSci December 2006 Sponsors’ statement The use of non-human primates continues to be one the most contentious areas of biological and medical research. The publication of this independent report into the scientific basis for the past, current and future role of non-human primates in research is both a necessary and timely contribution to the debate. We emphasise that members of the working group have worked independently of the four sponsoring organisations. Our organisations did not provide input into the report’s content, conclusions or recommendations. -

Merkel Cell Polyomavirus DNA in Immunocompetent and Immunocompromised Patients with Respiratory Disease
Journal of Medical Virology 83:2220–2224 (2011) Merkel Cell Polyomavirus DNA in Immunocompetent and Immunocompromised Patients With Respiratory Disease Bahman Abedi Kiasari,1,3* Pamela J. Vallely,1 and Paul E. Klapper1,2 1Department of Virology, Genomic Epidemiology Research Group, School of Translational Medicine, University of Manchester, Manchester, United Kingdom 2Clinical Virology, Manchester Medical Microbiology Partnership, Manchester Royal Infirmary, Oxford Road, Manchester, United Kingdom 3Human Viral Vaccine Department, Razi Vaccine & Serum Research Institute, Hesarak, Karaj, Iran Merkel cell polyomavirus (MCPyV) was identi- INTRODUCTION fied originally in association with a rare but aggressive skin cancer, Merkel cell carcinoma. In the past few years, a number of new human poly- The virus has since been found in the respirato- omaviruses, KI, WU, human polyomavirus 6 (HPyV6), ry tract of some patients with respiratory human polyomavirus 7 (HPyV7), trichodysplasia spi- disease. However, the role of MCPyV in the nulosa virus (TSV), human polyomavirus 9 (HPyV9), causation of respiratory disease has not been and Merkel cell polyomavirus (MCPyV) have been established. To determine the prevalence of discovered [Allander et al., 2007; Gaynor et al., 2007; MCPyV in 305 respiratory samples from Feng et al., 2008; Schowalter et al., 2010; van der immunocompetent and immunocompromised Meijden et al., 2010; Scuda et al., 2011]. MCPyV was patients and evaluate their contribution to re- discovered by digital transcriptome subtraction from a spiratory diseases, specimens were screened human skin cancer, Merkel cell carcinoma [Feng for MCPyV using single, multiplex, or real-time et al., 2008]. The finding of MCPyV in human Merkel PCR; co-infection with other viruses was exam- cell carcinoma suggests a role for this virus in the ined. -

An Overview on Human Polyomaviruses Developing Cancer
The Journal of Medical Research 2020; 6(4): 125-127 Review Article An overview on human polyomaviruses developing cancer in JMR 2020; 6(4): 125-127 humans July- August ISSN: 2395-7565 Mohammad Salim1, Mohammad Shahid Masroor2, Shagufta parween3, I.P. Prajapati1 © 2020, All rights reserved 1 Sanjay Gandhi Smriti Govt. Autonomous P.G. College, Sidhi, (affiliated to APS University, Rewa), Madhya Pradesh- www.medicinearticle.com 486661, India Received: 22-06-2020 2 People’s College of Dental Sciences & Research Center, People's University, Bhopal, Madhya Pradesh- 462037, Accepted: 14-07-2020 India 3 All India Institute of Medical sciences (AIIMS), Bhopal, Madhya Pradesh-462020, India Abstract The family Polyomaviridae included about a dozen of human polyomaviruses (HPyVs), of which MCPyV, SV-40, JCV and BKV viruses have been reported to cause cancer in human. Merkel cell carcinoma is a very aggressive type of skin cancer caused by the MCPyV5. Similarly, while SV-40 and JCV viruses developed brain tumor cancer, the BK virus has been linked to renal transplantations and nephropathy producing urinary bladder tumor and prostate cancer in human. In this paper we have tried to summarize the recent information gained in the field of human polyomaviruses causing cancer in human. Keywords: Human polyomaviruses, Cancer, Virus. INTRODUCTION Viruses are among the few causes of cancer contributing to a variety of malignancies. In 1966, when Peyton Rous was awarded a Nobel prize in physiology and medicine for his discovery of Rous chicken sarcoma virus as a cause of cancer, a renewed interest came in the field of microbial origin of cancer. -

Viruses in Transplantation - Not Always Enemies
Viruses in transplantation - not always enemies Virome and transplantation ECCMID 2018 - Madrid Prof. Laurent Kaiser Head Division of Infectious Diseases Laboratory of Virology Geneva Center for Emerging Viral Diseases University Hospital of Geneva ESCMID eLibrary © by author Conflict of interest None ESCMID eLibrary © by author The human virome: definition? Repertoire of viruses found on the surface of/inside any body fluid/tissue • Eukaryotic DNA and RNA viruses • Prokaryotic DNA and RNA viruses (phages) 25 • The “main” viral community (up to 10 bacteriophages in humans) Haynes M. 2011, Metagenomic of the human body • Endogenous viral elements integrated into host chromosomes (8% of the human genome) • NGS is shaping the definition Rascovan N et al. Annu Rev Microbiol 2016;70:125-41 Popgeorgiev N et al. Intervirology 2013;56:395-412 Norman JM et al. Cell 2015;160:447-60 ESCMID eLibraryFoxman EF et al. Nat Rev Microbiol 2011;9:254-64 © by author Viruses routinely known to cause diseases (non exhaustive) Upper resp./oropharyngeal HSV 1 Influenza CNS Mumps virus Rhinovirus JC virus RSV Eye Herpes viruses Parainfluenza HSV Measles Coronavirus Adenovirus LCM virus Cytomegalovirus Flaviviruses Rabies HHV6 Poliovirus Heart Lower respiratory HTLV-1 Coxsackie B virus Rhinoviruses Parainfluenza virus HIV Coronaviruses Respiratory syncytial virus Parainfluenza virus Adenovirus Respiratory syncytial virus Coronaviruses Gastro-intestinal Influenza virus type A and B Human Bocavirus 1 Adenovirus Hepatitis virus type A, B, C, D, E Those that cause -

A Guide to Clinical Management and Public Health Response for Hand, Foot and Mouth Disease (HFMD)
A Guide to Clinical Management and Public Health Response for Hand, Foot and Mouth Disease (HFMD) WHO Western Pacific Region PUBLICATION ISBN-13 978 92 9061 525 5 A Guide to Clinical Management and Public Health Response for Hand, Foot and Mouth Disease (HFMD) WHO Library Cataloguing in Publication Data A Guide to clinical management and public health response for hand, foot and mouth disease (HFMD) 1. Hand, foot and mouth disease – epidemiology. 2. Hand, foot and mouth disease – prevention and control. [ ii ] 3. Disease outbreaks. 4. Enterovirus A, Human. I. Regional Emerging Disease Intervention Center. ISBN 978 92 9061 525 5 (NLM Classification: WC 500) © World Health Organization 2011 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). For WHO Western Pacific Regional Publications, request for permission to reproduce should be addressed to the Publications Office, World Health Organization, Regional Office for the Western Pacific, P.O. Box 2932, 1000, Manila, Philippines, (fax: +632 521 1036, e-mail: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. -

JUAN MANUEL 2016 NOBEL PEACE PRIZE RECIPIENT Culture Friendship Justice
Friendship Volume 135, № 1 Character Culture JUAN MANUEL SANTOS 2016 NOBEL PEACE PRIZE RECIPIENT Justice LETTER FROM THE PRESIDENT Dear Brothers, It is an honor and a privilege as your president to have the challenges us and, perhaps, makes us question our own opportunity to share my message with you in each edition strongly held beliefs. But it also serves to open our minds of the Quarterly. I generally try to align my comments and our hearts to our fellow neighbor. It has to start with specific items highlighted in each publication. This with a desire to listen, to understand, and to be tolerant time, however, I want to return to the theme “living our of different points of view and a desire to be reasonable, Principles,” which I touched upon in a previous article. As patient and respectful.” you may recall, I attempted to outline and describe how Kelly concludes that it is the diversity of Southwest’s utilization of the Four Founding Principles could help people and “treating others like you would want to be undergraduates make good decisions and build better treated” that has made the organization successful. In a men. It occurred to me that the application of our values similar way, Stephen Covey’s widely read “Seven Habits of to undergraduates only is too limiting. These Principles are Highly Effective People” takes a “values-based” approach to indeed critical for each of us at this particularly turbulent organizational success. time in our society. For DU to be a successful organization, we too, must As I was flying back recently from the Delta Upsilon be able to work effectively with our varied constituents: International Fraternity Board of Directors meeting in undergraduates, parents, alumni, higher education Arizona, I glanced through the February 2017 edition professionals, etc. -

Detection and Quantification of Classic and Emerging Viruses by Skimmed
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by CONICET Digital water research xxx (2013) 1e14 Available online at www.sciencedirect.com journal homepage: www.elsevier.com/locate/watres Detection and quantification of classic and emerging viruses by skimmed-milk flocculation and PCR in river water from two geographical areas Byron Calgua a, Tulio Fumian b, Marta Rusin˜ola, Jesus Rodriguez-Manzano a, Viviana A. Mbayed c, Silvia Bofill-Mas a, Marize Miagostovich b, Rosina Girones a,* a Department of Microbiology, Faculty of Biology, University of Barcelona, Av. Diagonal 643, Barcelona 08028, Spain b Laboratory of Comparative and Environmental Virology, Oswaldo Cruz Institute, Avenida Brasil 4365, Rio de Janeiro, Brazil c Laboratory of Virology, Faculty of Pharmacy and Biochemistry, University of Buenos Aires, Junı´n 956, Buenos Aires, Argentina article info abstract Article history: Molecular techniques and virus concentration methods have shown that previously un- Received 24 September 2012 known viruses are shed by humans and animals, and may be transmitted by sewage- Received in revised form contaminated water. In the present study, 10-L river-water samples from urban areas in 16 February 2013 Barcelona, Spain and Rio Janeiro, Brazil, have been analyzed to evaluate the viral Accepted 21 February 2013 dissemination of human viruses, validating also a low-cost concentration method for virus Available online xxx quantification in fresh water. Three viral groups were analyzed: (i) recently reported vi- ruses, klassevirus (KV), asfarvirus-like virus (ASFLV), and the polyomaviruses Merkel cell Keywords: (MCPyV), KI (KIPyV) and WU (WUPyV); (ii) the gastroenteritis agents noroviruses (NoV) and Emerging virus rotaviruses (RV); and (iii) the human fecal viral indicators in water, human adenoviruses Polyomavirus (HAdV) and JC polyomaviruses (JCPyV). -
Guidelines for Occupational Health Follow up of Communicable Diseases for Manager/Supervisors
Winnipeg Regional Health Authority Occupational and Environmental Safety & Health (OESH) Guidelines for Occupational Health Follow Up of Communicable Diseases For Manager/Supervisors Page | 1 2019.02.04 version 2 Winnipeg Regional Health Authority Occupational and Environmental Safety & Health (OESH) INTRODUCTION ................................................................................................................................................................................. 3 WORKERS COMPENSATION BOARD (WCB) CLAIMS ........................................................................................................................... 5 ANTIBIOTIC RESISTANT ORGANISMS (AROS) ..................................................................................................................................... 6 BLOOD AND BODY FLUID EXPOSURES ............................................................................................................................................... 9 CIMEX LECTULARIUS (BED BUGS) .................................................................................................................................................... 10 CREUTZFELDT-JAKOB DISEASE (CJD) ................................................................................................................................................ 11 DIARRHEA (BACTERIAL, CLOSTRIDIUM DIFFICILE (C. DIFFICILE), VIRAL) ........................................................................................... 12 GROUP A STREPTOCOCCUS ............................................................................................................................................................