Trust Headquarters, Doncaster
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Doncaster Green Infrastructure Strategy 2014- 2028
The Doncaster Green Infrastructure Strategy 2014- 2028 Creating a Greener, Healthier & more Attractive Borough Adoption Version April 2014 Doncaster Council Service Improvement & Policy (Regeneration & Environment) 0 1 the potential of the Limestone Valley, which runs through the west of the borough. Did you know that Doncaster has 65 different woodlands which cover an area in excess of 521 hectares? That’s about the equivalent to over 1,000 football pitches. There are 88 different formal open spaces across the borough, which include football, rugby and cricket pitches, greens, courts and athletics tracks. Doncaster is also home to 12 golf courses. The Trans-Pennine Trail passes through Doncaster and is integral to the extensive footpath and cycle network that link the borough’s communities with the countryside, jobs and recreation opportunities. There are so Foreword from the many more features across Doncaster and these are covered within this Strategy document. Portfolio Holder… Despite this enviable position that communities in Doncaster enjoy, there is always so much more that can be done to make the borough’s GI even greater. The Strategy sets out a framework As Portfolio Holder for Environment & Waste at for ensuring maximum investment and funding Doncaster Council, I am delighted to introduce is being channelled, both by the Council and the the Doncaster Green Infrastructure Strategy vast array of important partners who invest so 2014-2028: Creating a Greener, Healthier & much time and resources, often voluntarily, into more Attractive Borough. making our GI as good as it can be. As the largest metropolitan Borough in the This Strategy will help deliver a better country, covering over 220 square miles, connected network of multi-purpose spaces and Doncaster has an extensive green infrastructure provide the opportunity for the coordination (GI) network which includes numerous assets and delivery of environmental improvements and large areas that are rural in character. -

Local Environment Agency Plan
6 o x I local environment agency plan SOUTH YORKSHIRE & NORTH EAST DERBYSHIRE FIRST ANNUAL REVIEW May 1999 BARNSLEY ROTHERHAM SHEFFIELD CHEST ELD E n v ir o n m e n t Ag e n c y NATIONAL LIBRARY & INFORMATION SERVICE HEAD OFFICE Rio House, Waterside Drive, Aztec West. Almondsbury, Bristol BS32 4UD South Yorkshire & North East Derbyshire LEA P First Annua! Review SOUTH YORKSHIRE AND NORTH EAST DERBYSHIRE AREA ADMINISTRATIVE BOUNDARIES W . 'H D i SwllhoJ* j Oram iRNSLEY DONCASTER ) ROTHERHAM SHEFFIELD (DERBYSHIRE DALES) KEY CHESTERF.IEUD) BOLSOVER - CATCWENT BOUNDARY RIVER ADMINISTRATIVE BOUNDARY MAIN ROAD SGRTH EAST \ 0 2 4 6 8 10km ___1 i_________ i_________ i_________ i_________ i Scale ENVIRONMENT AGENCY 032505 South Yorkshire & North East Derbyshire LEAP First Annual Review EXECUTIVE SUMMARY The South Yorkshire & North East Derbyshire LEAP First Annual Review reports on the progress made during the last year against LEAP actions. The actions published in the LEAP are supplemental to our everyday work on monitoring, surveying and regulating to protect the environment. Some of the key achievements on our everyday work include: i) In September 1998 Michael Clapham MP officially opened the Bullhouse Minewater Treatment Plant. The scheme is a pioneering £1.2m partnership project funded by European Commission, Coal Authority, Environment Agency, Hepworths Building Products, Barnsley MBC and Yorkshire Water. Within one week a visible reduction could be seen in ochre levels in the River Don, after more than 100 years of pollution. ii) Monckton Coke and Chemical Company have successfully commissioned a combined heat and power plant, costing approximately £7 million. -

HOUSING B) ECONOMIC TRANSFORMATION C) SHOPPING, SERVICES and TOWN and DISTRICT CENTRES D) ENVIRONMENT D) ACCESS and TRANPORTATION E) OTHER INFRASTRUCTURE
DONCASTER CORE STRATEGY CONSULTATION DRAFT October 2008 CONTENTS INTRODUCTION AND SUMMARY GLOSSARY THE ROLE OF THE LDF AND CORE STRATEGY KEY ELEMENTS DONCASTER’S CHARACTERISTICS AND ISSUES DONCASTER’S VISION AND STRATEGIC OBJECTIVES BUILDING IN FLEXIBILITY IN THE CORE STRATEGY KEY DIAGRAM SPATIAL STRATEGY FOR DONCASTER a) SUSTAINABILITY STRATEGY b) SUSTAINABLE SETTLEMENT STRATEGY c) AREA SPATIAL STRATEGIES BOROUGH WIDE POLICIES a) HOUSING b) ECONOMIC TRANSFORMATION c) SHOPPING, SERVICES AND TOWN AND DISTRICT CENTRES d) ENVIRONMENT d) ACCESS AND TRANPORTATION e) OTHER INFRASTRUCTURE RESPONSE FORM APPENDICES - APPENDIX 1: PLANS - APPENDIX 2: IMPLENTATION, FLEXIBILITY, MONITORING AND MANAGEMENT - APPENDIX 3: OTHER POLICIES, STRATEGIES AND PLANS - APPENDIX 4: UDP POLICIES TO BE REPLACED BY CORE STRATEGY 1 DONCASTER CORE STRATEGY CONSULTATION DRAFT October 2008 INTRODUCTION AND SUMMARY 1. Why this document is needed Doncaster’s Core Strategy is part of the new Local Development Framework (LDF), which will replace the Unitary Development Plan which was adopted in 1998. The Core Strategy will set out broadly how it is proposed that Doncaster will develop over the 16 year period from its adoption in 2010 to 2025. The LDF will be the spatial expression of the Borough Strategy. The Core Strategy will set out major planning strategy and policy and locations for different types of development like housing, offices, mineral working and waste treatment plants across the borough – to transform Doncaster into an ‘Eco Borough’ based on a range -

Neutral and Wet Grassland (NWG)
Neutral and Wet Grassland (NWG) Habitat Action Plan Doncaster Local Biodiversity Action Plan January 2007 Table of Contents Page 1. Description 1 2. National status 5 3. Local status 6 4. Legal status 9 5. Links to associated habitats & species 10 6. Current factors causing loss or decline 11 7. Current local action 14 8. Objectives, targets & proposed actions 17 9. Indicative Habitat distribution & Opportunities map 29 Doncaster Biodiversity Action Partnership Doncaster Council, Environmental Planning, 2nd Floor, Danum House, St Sepulchre Gate, Doncaster, DN1 1UB. Telephone: 01302 862896 Email: [email protected] For further information please visit www.doncaster.gov.uk or contact; Doncaster Biodiversity Actionwww.doncaster.gov.uk/biodiversity Partnership, c/o Doncaster Metropolitan Borough Council, Environmental Planning, Spatial Planning and Economic Development, Directorate of Development, 2nd Floor, Danum House, St Sepulchre Gate, Doncaster, DN1 1UB, Tel: 01302 862896, E-mail: [email protected] MM67-120 DONCASTER LOCAL BIODIVERSITY ACTION PLAN 1. Description 1.1 The low-lying clay and alluvial soils of the Humberhead Levels provide excellent conditions for intensive agricultural production. This landscape tends to be dominated by arable cultivation, improved grazing pastures and rye- grass leys, but some small pockets unimproved and semi-improved neutral grassland still survive. 1.2 The most diverse of these neutral grasslands are typically flower-rich hay meadows or pastures with a diversity of grasses and sedges such as common bent (Agrostis capillaries), sweet vernal-grass (Anthoxanthum oderatum), quaking grass (Briza media), crested dog's-tail (Cynosurus cristatus), red fescue (Festuca rubra), Yorkshire fog (Holcus lanatus), cock's-foot (Dactylis glomerata), spring sedge (Carex caryophyllea), glaucous sedge (Carex flacca), and varying proportions of perennial ryegrass (Lolium perenne). -
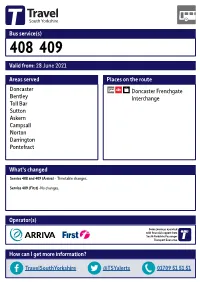
Valid From: 28 June 2021 Bus Service(S
Bus service(s) 408 409 Valid from: 28 June 2021 Areas served Places on the route Doncaster Doncaster Frenchgate Bentley Interchange Toll Bar Sutton Askern Campsall Norton Darrington Pontefract What’s changed Service 408 and 409 (Arriva) - Timetable changes. Service 409 (First) -No changes. Operator(s) Some journeys operated with financial support from South Yorkshire Passenger Transport Executive How can I get more information? TravelSouthYorkshire @TSYalerts 01709 51 51 51 Bus route map for services 408 and 409 27/07/2018# Ferrybridge Kellingley Knottingley Eggborough Hensall Pontefract, Bus Stn 408 409 Cridling Stubbs Great Heck Darrington, Darrington Hotel/ Whitley Pontefract, Crest Dr/ Manor Park Rise Woodland View Darrington Womersley, Main St Carleton, Carleton Rd/Green Ln 409 Womersley East Hardwick 409 Balne 408Ï 408Ð Wentbridge, Went Edge Rd/Jackson Ln Kirk Smeaton, Cemetery Wentbridge,Low Ackworth Wentbridge Rd/Wentbridge Ln Walden Stubbs Thorpe Audlin, Fox & Hounds/Thorpe Ln Wentbridge Kirk Smeaton Norton, West End Rd/Broc-O-Bank Fenwick Thorpe Audlin 408 408 409 Askern, Selby Rd/Campsall Rd Norton Badsworth Askern, Station Rd/High St Campsall, Old Bells/High St 408 Moss Upton Askern, Eden Dr/ Hemsworth 408 Instoneville, Coniston Rd Barnsdale Bar, Woodfield Rd/Warren House Sutton Rd/Alfred Rd North Elmsall Sutton Skelbrooke Burghwallis Instoneville, Sutton Rd/Manor Way Owston South Kirkby South Elmsall Skellow Carcroft Hampole Toll Bar Toll Bar, Doncaster Rd/Bentley Moor Ln Clayton Hooton Pagnell Woodlands Arksey Pickburn Brodsworth -
Robin Hood As Much As Possible
Issue 34 ∙ April-May 2010 . LeftLion Magazine Issue 34 contents April - May 2010 editorial Youths and ducks, If you’ve read any of the thirty-three previous issues of LeftLion, you’ll know that we’ve avoided covering the subject of Robin Hood as much as possible. There’s a good reason for that; because, like you, we’ve always known that there is far more to the Motherland than some bloke arsing about in Sherwood Forest, and we’d sooner give the less bigged-up avenues of Nottingham culture a shine. There are many reasons why we decided to cave in and roll out a massive tribute to the Hooded Man this ish. For one, it’s because of the resurgence of pride in our mythical lore. For two, it’s a reaction to the disgusting attempt by 9 16 28 the North to nick our local hero (hey, Yorkshire; we gave the world the greatest and most enduring goodies-versus- baddies story ever. You gave us Emmerdale. End of). For May Contain Notts CSI: Sherwood Music Reviews three, it’s because people ‘round here have finally realised 04 The local news diary that pays your 12 Carl Fellstrom on the link between the 21 Beck Stacey, Fists, Feelings By Design, that it’s time to firmly reclaim the legend for Nottingham, Nana and her mate to dress up as Merry Men and the Disaffected Youths Grande Duke, Kingclaw, Mascot Fight, and we want to chip in on the debate. And yeah, because schoolgirls and erotically pass a Moules & Miggins, Nephu Huzzband there’s a new film coming out. -
BGS Report, Single Column Layout
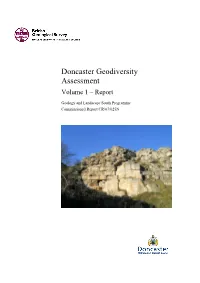
Doncaster Geodiversity Assessment Volume 1 – Report Geology and Landscape South Programme Commissioned Report CR/07/025N BRITISH GEOLOGICAL SURVEY GEOLOGY AND LANDSCAPE SOUTH PROGRAMME COMMISSIONED REPORT CR/07/025N Doncaster Geodiversity Assessment Volume 1 – Report S Engering and H F Barron The National Grid and other Ordnance Survey data are used with the permission of the Contributors Controller of Her Majesty’s Stationery Office. Licence No: 100017897/2007. Keywords Geodiversity; Doncaster. Editor Front cover A H Cooper Permian Bryozoan reef, North Cliff Quarry, Doncaster Bibliographical reference ENGERING, S & BARRON, H F. 2007. Doncaster Geodiversity Assessment. British Geological Survey Commissioned Report, CR/07/025N. 139pp. Copyright in materials derived from the British Geological Survey’s work is owned by the Natural Environment Research Council (NERC) and/or the authority that commissioned the work. You may not copy or adapt this publication without first obtaining permission. Contact the BGS Intellectual Property Rights Section, British Geological Survey, Keyworth, e-mail [email protected]. You may quote extracts of a reasonable length without prior permission, provided a full acknowledgement is given of the source of the extract. Maps and diagrams in this report use topography based on Ordnance Survey mapping. © NERC 2007. All rights reserved Keyworth, Nottingham British Geological Survey 2007 BRITISH GEOLOGICAL SURVEY The full range of Survey publications is available from the BGS British Geological Survey offices Sales Desks at Nottingham, Edinburgh and London; see contact details below or shop online at www.geologyshop.com Keyworth, Nottingham NG12 5GG The London Information Office also maintains a reference 0115-936 3241 Fax 0115-936 3488 collection of BGS publications including maps for consultation. -

Cause Papers Project Standardization
1 Cause Papers in the Diocesan Courts of the Archbishopric of York, 1300–1858 Editing and Standardisation in the Cause Papers Database The Cause Papers project provided an on-line searchable catalogue of more than 13,000 cause papers relating to cases heard between 1300 and 1858 in the Church Courts of the diocese of York, the original records for which are held at the Borthwick Institute for Archives at the University of York. The project aimed to pioneer a new standard of excellence in data accuracy and standardization. Cataloguing such a large and varied number of records posed numerous challenges in these areas, including the problem of how to incorporate spelling and language variations of surname and place names. The following document provides information on the methods used by the project team in compiling, editing and standardizing the data. It is split into the following sections:- 1) Information provided by the database 2) List of standard reference works used by the project team 3) List of types and sub-types of cases commonly used in the database 4) Standardization of Forenames 5) Standardization of Surnames – Part A 6) Standardization of Surnames – Part B 7) Problematic Place-names – Identification and Standardization Please note that this text is not intended as a guide to on-line catalogue. Users requiring assistance with searching the catalogue should consult the on-screen help text. 2 Editing and standardisation for the Cause Paper Database 1) Information provided by the database Owing to the volume and complexity of manuscript material involved, it was not possible to provide full transcriptions of the cause papers. -

York Clergy Ordinations 1800-1849
YORK CLERGY ORDINATIONS 1800-1849 Sara Slinn Borthwick List and Index 28 2001 © University of York 2001 ISBN 0-903857-80-4 ISSN 1361-3014 CONTENTS pages Introduction and editorial method …………………….…… i List of abbreviations ………………………………………. xiv Alphabetical list of York ordinands, 1800-1849 ………….. 1 Appendix 1 Unsuccessful candidates …………….. 209 Appendix 2 Table of York Ordinations, 1800-1849 ….. 215 Index ………………………………………………………. 220 YORK CLERGY ORDINATIONS, 1800-1849 INTRODUCTION & EDITORIAL METHOD INTRODUCTION BACKGROUND - THE DIOCESE OF YORK The first half of the nineteenth century was a period of great change not just for the Church of England as a whole, but for the diocese of York in particular. In territorial terms it was a time of loss. The diocese of Ripon was founded in 1836 taking with it some of the most heavily populated new industrial regions of West Yorkshire, Bradford, Halifax and Leeds. By 1836 the archbishop had also lost his peculiar jurisdiction over Hexhamshire and in 1837 the archdeaconry of Nottingham was transferred to the diocese of Lincoln. Even though a time of territorial loss for the diocese, it was a period of increased church building. When changing expectations of the parochial role of the clergy, the demand for clerical residence and the provision of a living wage for stipendary curates and increased parochial demands for preaching and the sacraments within a broadening definition of parochial work are added to this the period is seen to be one of repeated adaptation and change. ORDINATION- THE SOURCES From the middle of the eighteenth century onwards the information recorded in the York Institution Act Books can be validated and expanded by reference to the bundles of papers submitted by the candidates themselves prior to their taking orders. -

Doncaster Metropolitan Borough Council Planning
DONCASTER METROPOLITAN BOROUGH COUNCIL PLANNING COMMITTEE - 7th February 2017 Application 4 Application 16/02552/OUT Application 5th December 2016 Number: Expiry Date: Application Outline Application Type: Proposal Outline application for erection of stables, toilets, equipment and hay Description: store (Approval being sought for Access, Appearance and Landscaping) At: Skelbrooke Stables Bannister Lane Skelbrooke Doncaster For: Mr George Smith Third Party Reps: 49 representations Parish: Hampole And Skelbrooke and a 80 name Parish Meeting petition Ward: Sprotbrough Author of Report Mark Ramsay MAIN RECOMMENDATION: GRANT 1.0 Reason for Report 1.1 This application is being presented to Planning Committee due to the level of public interest. 2.0 Proposal and Background 2.1 The proposal is in Outline only with matters of access appearance and landscaping to be agreed but scale and layout reserved for further consideration in a future application. The proposal has been amended since it was first submitted, reducing the scale of the hay store and toilet facility and reducing the number of stables. Additionally reference to a riding school and a ménage (which was outside the redline of the application) have also been omitted. 2.2 The site is on the opposite side of the road from the residential area of the hamlet of Skelbrooke and located in the South Yorkshire Green Belt. There is an existing metalled access running into the middle of the land owned by the applicant with an existing L shaped timber stable block in the north east corner of the site. 2.3 The site is located next to a beck which runs between the stables and the copse wood. -
Doncaster Local Plan Local Plan Evidence Base
Doncaster Local Plan Local Plan Evidence Base Assessing Mineral Sites Representations Version: Consultation Draft May 2018 0 Table of Contents Assessment of Industry Representations for Minerals Development ............................................................. 2 National Policy .......................................................................................................................................... 2 Doncaster’s Mineral Resources .................................................................................................................... 2 Sand and Gravel ....................................................................................................................................... 2 Limestone (Dolomite) ................................................................................................................................ 3 Industrial Dolomite .................................................................................................................................... 4 Clay .......................................................................................................................................................... 4 Groundwater Protection - The Sherwood Sandstone Aquifer .................................................................... 4 Site Assessment Methodology (Summary) ................................................................................................ 4 Stages One and Two: .............................................................................................................................. -
A Saunter Through the Ages Down the Avenue Burghwallis
A Saunter Through The Ages Down The Avenue Burghwallis Being An Unofficial History of Saint Helen’s Church & Some Village Gossip H. R. Dimon. March 1962 (HARRIS BROS) A PERSONAL INTRODUCTION Dear Subscriber, I have just been looking through some shocking old records — my school report, for instance. Boys, I suppose, keep either one or other of two people busy — the Doctor or the Policeman. In my case it was the former. He spoke to Father in the only language Pa understood: “The child’s a little hot-house plant.” This explains a laconic remark on my school report: “History — Good, when present” ! And to that the fact that I’ve never known what time it is, and it is obvious that I am no historian. Neither am I a “literary man.” The language I use has never been called anything but bad. Therefore, you have been warned; my qualifications “to write up a history” are as good as a plumber’s to bake a cake. If the result is as heavy as lead, the fault is in the mixing; the ingredients are good. Three reasons are given for making an attempt. Two follow immediately; the third is tacked on to the end of the foreword, as a tail. 1. For a long time a knitting-together of the historical data of our Church has seemed desirable. Having watched the reactions of a party of Americans round a guide in the Tower of London, on the spot where Sir Walter Raleigh was beheaded, one felt an inadequacy in our own treatment of visitors genuinely seeking after historical details of the Church.