NAEMSP® Review Guide for Emergency Medical Services Clinical Practice and Systems Oversight, Second Edition 2018 Edition
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ABCDE Approach
The ABCDE and SAMPLE History Approach Basic Emergency Care Course Objectives • List the hazards that must be considered when approaching an ill or injured person • List the elements to approaching an ill or injured person safely • List the components of the systematic ABCDE approach to emergency patients • Assess an airway • Explain when to use airway devices • Explain when advanced airway management is needed • Assess breathing • Explain when to assist breathing • Assess fluid status (circulation) • Provide appropriate fluid resuscitation • Describe the critical ABCDE actions • List the elements of a SAMPLE history • Perform a relevant SAMPLE history. Essential skills • Assessing ABCDE • Needle-decompression for tension • Cervical spine immobilization pneumothorax • • Full spine immobilization Three-sided dressing for chest wound • • Head-tilt and chin-life/jaw thrust Intravenous (IV) line placement • • Airway suctioning IV fluid resuscitation • • Management of choking Direct pressure/ deep wound packing for haemorrhage control • Recovery position • Tourniquet for haemorrhage control • Nasopharyngeal (NPA) and oropharyngeal • airway (OPA) placement Pelvic binding • • Bag-valve-mask ventilation Wound management • • Skin pinch test Fracture immobilization • • AVPU (alert, voice, pain, unresponsive) Snake bite management assessment • Glucose administration Why the ABCDE approach? • Approach every patient in a systematic way • Recognize life-threatening conditions early • DO most critical interventions first - fix problems before moving on -

Detail Report
Supplemental Update Report CR Number: 2012319113 Implementation Date: 16-Jan-19 Related CR: 2012319113 MedDRA Change Requested Add a new SMQ Final Disposition Final Placement Code # Proposed SMQ Infusion related reactions Rejected After Suspension MSSO The proposal to add a new SMQ Infusion related reactions is not approved after suspension. The ICH Advisory Panel did approve this SMQ topic to go into the development phase and it Comment: underwent testing in three databases (two regulatory authorities and one company). However, there were numerous challenges encountered in testing and the consensus decision of the CIOMS SMQ Implementation Working Group was that the topic could not be developed to go into production as an SMQ. Most notably, in contrast to other SMQs, this query could not be tested using negative control compounds because it was not possible to identify suitable compounds administered via infusion that were not associated with some type of reaction. In addition, there is no internationally agreed definition of an infusion related reaction and the range of potential reactions associated with the large variety of compounds given by infusion is very broad and heterogenous. Testing was conducted on a set of around 500 terms, the majority of which was already included in Anaphylactic reaction (SMQ), Angioedema (SMQ), and Hypersensitivity (SMQ). It proved difficult to identify potential cases of infusion related reactions in post-marketing databases where the temporal relationship of the event to the infusion is typically not available. In clinical trial databases where this information is more easily available, users are encouraged to provide more specificity about the event, e.g., by reporting “Anaphylactic reaction” when it is known that this event is temporally associated with the infusion. -

Airway – Oropharyngeal: Insertion; Maintenance; Suction; Removal
Policies & Procedures Title: AIRWAY – OROPHARYNGEAL: INSERTION; MAINTENANCE; SUCTION; REMOVAL I.D. Number: 1159 Authorization Source: Nursing Date Revised: September 2014 [X] SHR Nursing Practice Committee Date Effective: October 2002 Date Reaffirmed: January 2016 Scope: SHR Acute, Parkridge Centre Any PRINTED version of this document is only accurate up to the date of printing 30-May-16. Saskatoon Health Region (SHR) cannot guarantee the currency or accuracy of any printed policy. Always refer to the Policies and Procedures site for the most current versions of documents in effect. SHR accepts no responsibility for use of this material by any person or organization not associated with SHR. No part of this document may be reproduced in any form for publication without permission of SHR. 1. PURPOSE 1.1 To safely and effectively use Oropharyngeal Airway (OPA). 2. POLICY 2.1 The Registered Nurse (RN), Registered Psychiatric Nurse (RPN), Licensed Practical Nurse (LPN), Graduate Nurse (GN), Graduate Psychiatric Nurse (GPN), Graduate Licensed Practical Nurse (GLPN) will insert, maintain, suction and remove an oropharyngeal airway (OPA). 2.2 The OPA may be inserted to establish and assist in maintaining a patent airway. 2.3 An OPA should only be used in patients with decreased level of consciousness or decreased gag reflex. 2.4 Patients with OPAs that have been inserted for airway protection should not be left unattended due to risk of aspiration if gag reflex returns unexpectedly. Page 1 of 4 Policies and Procedures: Airway – Oropharyngeal: Insertion; Maintenance; I.D. # 1159 Suction; Removal 3. PROCEDURE 3.1 Equipment: • Oropharyngeal airway of appropriate size • Tongue blade (optional) • Clean gloves • Optional: suction equipment, bag-valve-mask device 3.2 Estimate the appropriate size of airway by aligning the tube on the side of the patient’s face parallel to the teeth and choosing an airway that extends from the ear lobe to the corner of the mouth. -

Understanding Code Status
Understanding Code Status It’s important to consider the type of Code status conversations should include questions such as: medical treatments you want before • Which treatments, if any, might you not want to a medical emergency occurs. All receive? patients must choose a code status. • Under which circumstances, if any, do you believe life-prolonging treatments would not be desirable? Understanding what each code means • How has your past experience, if any, created your and selecting a code status will help opinion about resuscitation procedures for yourself? your caregivers and loved ones follow It is very important to have this discussion your wishes. before a medical emergency occurs. What is Code Status? Choosing your Code Status All patients who are admitted to a hospital or an You will work with your health care provider to outpatient facility (such as a dialysis center or discuss the types of resuscitation procedures and outpatient surgery center) will be asked to choose advance medical treatments you would benefit from a code status for the duration of their stay. and the type that you may not want if a medical emergency were to occur. This conversation should Your chosen code status describes the type of help you determine which code status is right for you resuscitation procedures (if any) you would like the to live well with your goals in mind. health care team to conduct if your heart stopped beating and/or you stopped breathing. During this Outcomes after CPR medical emergency, resuscitation procedures must Unfortunately, what you see on TV is not reality. -

COVID-19 Mrna Pfizer- Biontech Vaccine Analysis Print
COVID-19 mRNA Pfizer- BioNTech Vaccine Analysis Print All UK spontaneous reports received between 9/12/20 and 22/09/21 for mRNA Pfizer/BioNTech vaccine. A report of a suspected ADR to the Yellow Card scheme does not necessarily mean that it was caused by the vaccine, only that the reporter has a suspicion it may have. Underlying or previously undiagnosed illness unrelated to vaccination can also be factors in such reports. The relative number and nature of reports should therefore not be used to compare the safety of the different vaccines. All reports are kept under continual review in order to identify possible new risks. Report Run Date: 24-Sep-2021, Page 1 Case Series Drug Analysis Print Name: COVID-19 mRNA Pfizer- BioNTech vaccine analysis print Report Run Date: 24-Sep-2021 Data Lock Date: 22-Sep-2021 18:30:09 MedDRA Version: MedDRA 24.0 Reaction Name Total Fatal Blood disorders Anaemia deficiencies Anaemia folate deficiency 1 0 Anaemia vitamin B12 deficiency 2 0 Deficiency anaemia 1 0 Iron deficiency anaemia 6 0 Anaemias NEC Anaemia 97 0 Anaemia macrocytic 1 0 Anaemia megaloblastic 1 0 Autoimmune anaemia 2 0 Blood loss anaemia 1 0 Microcytic anaemia 1 0 Anaemias haemolytic NEC Coombs negative haemolytic anaemia 1 0 Haemolytic anaemia 6 0 Anaemias haemolytic immune Autoimmune haemolytic anaemia 9 0 Anaemias haemolytic mechanical factor Microangiopathic haemolytic anaemia 1 0 Bleeding tendencies Haemorrhagic diathesis 1 0 Increased tendency to bruise 35 0 Spontaneous haematoma 2 0 Coagulation factor deficiencies Acquired haemophilia -

Cardiopulmonary Resuscitation EFFECTIVE DATE: October 2007 SUPERCEDES DATE: May 2004
HEALTH SERVICES POLICY & PROCEDURE MANUAL North Carolina Department Of Correction SECTION: Care and Treatment of Patient Division Of Prisons POLICY # TX I-7 PAGE 1 of 3 SUBJECT: Cardiopulmonary Resuscitation EFFECTIVE DATE: October 2007 SUPERCEDES DATE: May 2004 PURPOSE To provide guidelines in case of a medical emergency requiring Cardiopulmonary Resuscitation (CPR). To re-establish effective ventilation and circulation. To prevent irreversible brain damage. To provide an efficient and organized team approach in response to a medical emergency requiring Cardiopulmonary Resuscitation (CPR). To delineate the responsibilities of staff in the event of a medical emergency requiring Cardiopulmonary Resuscitation (CPR). POLICY All Health Services personnel will be certified in Cardiopulmonary Resuscitation (CPR) including Automated External Defibrillator (AED) according to guidelines set forth by the American Heart Association (AHA) “Basic Life Support Health Care Provider Course” (BLS-HCP). It is the responsibility of the employee to maintain current BLS-HCP CPR certification, with renewal every two years. Dental hygienists are required to renew annually per professional standards. Failure to recertify may result in the disciplinary process being initiated. Custody Officers are trained to provide CPR according to guidelines set forth by the American Heart Association “HeartSaver-AED Course”. Cardiopulmonary Resuscitation will be initiated on all patients demonstrating cardiac and/or respiratory arrest (i.e., absence of spontaneous respirations and/or pulseless), with the exception of: a. Decapitation b. Body tissue decomposition noted c. Verification of a current Do Not Resuscitate (DNR) order originated or approved by a physician in the employ of N.C. Division of Prisons. (1) Most patients with current DNR orders will be maintained in a Hospice unit, health ward, or infirmary with DNR located in patient’s chart with staff knowledge of such. -
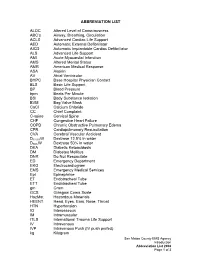
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC's Airway, Breathing, Circulation ACLS Advanced Cardiac Life Suppo
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC’s Airway, Breathing, Circulation ACLS Advanced Cardiac Life Support AED Automatic External Defibrillator AICD Automatic Implantable Cardiac Defibrillator ALS Advanced Life Support AMI Acute Myocardial Infarction AMS Altered Mental Status AMR American Medical Response ASA Aspirin AV Atrial Ventricular BHPC Base Hospital Physician Contact BLS Basic Life Support BP Blood Pressure bpm Beats Per Minute BSI Body Substance Isolation BVM Bag Valve Mask CaCl Calcium Chloride CC Chief Complaint C-spine Cervical Spine CHF Congestive Heart Failure COPD Chronic Obstructive Pulmonary Edema CPR Cardiopulmonary Resuscitation CVA Cerebral Vascular Accident D12.5%W Dextrose 12.5% in water D50%W Dextrose 50% in water DKA Diabetic Ketoacidosis DM Diabetes Mellitus DNR Do Not Resuscitate ED Emergency Department EKG Electrocardiogram EMS Emergency Medical Services Epi Epinephrine ET Endotracheal Tube ETT Endotracheal Tube gm Gram GCS Glasgow Coma Scale HazMat Hazardous Materials HEENT Head, Eyes, Ears, Nose, Throat HTN Hypertension IO Interosseous IM Intramuscular ITLS International Trauma Life Support IV Intravenous IVP Intravenous Push (IV push prefed) kg Kilogram San Mateo County EMS Agency Introduction Abbreviation List 2008 Page 1 of 3 J Joule LOC Loss of Consciousness Max Maximum mcg Microgram meds Medication mEq Milliequivalent min Minute mg Milligram MI Myocardial Infarction mL Milliliter MVC Motor Vehicle Collision NPA Nasopharyngeal Airway NPO Nothing Per Mouth NS Normal Saline NT Nasal Tube NTG Nitroglycerine NS Normal Saline O2 Oxygen OB Obstetrical OD Overdose OPA Oropharyngeal Airway OPQRST Onset, Provoked, Quality, Region and Radiation, Severity, Time OTC Over the Counter PAC Premature Atrial Contraction PALS Pediatric Advanced Life Support PEA Pulseless Electrical Activity PHTLS Prehospital Trauma Life Support PID Pelvic Inflammatory Disease PO By Mouth Pt. -

Faculty Meeting August 9Th, 2011
Review of Systems is a process that includes a review of body systems. It is carried out through a series of questions regarding signs and symptoms. The Review of Systems (ROS) includes information about the following 14 systems. Constitutional: description of general appearance; growth and development, recent weight loss/gain, malaise, chills weakness, fatigue, fever, vital signs, head circumference for a baby, appetite, sleep habits, insomnia, night sweats. Integumentary: (skin and/or breast) rashes, color, sores, dryness, itching, flaking, dandruff, lumps, moles, color change, changes in hair or nails, sweating, hives, bruising, scratches, scars, swelling., acne. Eyes: vision, no change in vision, glasses or contact lenses, last eye exam, eye pain, “eye” redness, excessive tearing, double vision, blurred vision, spots, specks, flashing lights, photophobia, glaucoma, cataracts. Ears, Nose, Mouth/ Throat Ears: hearing loss, tinnitus, vertigo, earaches, ear infections, ear discharges; if hearing is decreased, use of hearing aids. Nose and sinuses: frequent colds, stuffiness’, discharge drainage, nasal itching, hay fever, nosebleeds sinusitis, sinus trouble, sinus pressure, nasal congestion, nasal discharge, nasal infection Mouth/Throat condition of teeth and gums bleeding gums dentures, (how they fit) last dental exam, dry mouth, frequent sore throats, difficulty swallowing, no posterior pharynx pain, hoarseness, sores/ulcers, hoarseness, pyorrhea. Respiratory: cough, sputum, (color, quantity) shortness of breath, pleuritic chest pain, wheezing, asthma, bronchitis, TB, emphysema, pneumonia, hemoptysis, CXR. Cardiovascular: heart trouble; high blood pressure; CV hypertension, heart murmurs, chest pain/ pressure palpitations, dyspnea, orthopnea,, rheumatic fever, paroxysmal nocturnal dyspnea, edema; past EKG or other heart tests. Peripheral Vascular; intermittent claudication, leg cramps, varicose veins, past clots in the vein, syncope, edema. -

VHA Dir 1101.05(2), Emergency Medicine
Department of Veterans Affairs VHA DIRECTIVE 1101.05(2) Veterans Health Administration Transmittal Sheet Washington, DC 20420 September 2, 2016 EMERGENCY MEDICINE 1. REASON FOR ISSUE: This Veterans Health Administration (VHA) directive establishes policy and procedures for VHA Emergency Departments (EDs) and Urgent Care Centers (UCCs). 2. SUMMARY OF MAJOR CHANGES: This directive replaces the previous VHA handbook establishing procedures for VA EDs and UCCs. The following major changes are included: a. Information on EDs, UCCs, diversion, Mental Health, sexual assault, temporary beds, ED/UCC staffing, and Emergency Department Integration Software (EDIS) was added. b. Information about the Intermediate Healthcare Technician Program. c. Information about the ED and Women’s Health, Out of Operating Room Airway Management and Ensuring Correct Surgery and Invasive Procedures, and geriatric emergency care. d. Information about the Emergency Medicine Improvement Initiative and support resources. 3. RELATED ISSUE: None. 4. RESPONSIBLE OFFICE: The Office of Patient Care Services (10P), Specialty Care Services (10P4E), is responsible for the content of this VHA Handbook. Questions may be referred to the National Director for Emergency Medicine at 202-461-7120. 5. RESCISSIONS: VHA Handbook 1101.05, dated May 12, 2010; VHA Directive 1051, dated February 21, 2014; VHA Directive 1079, dated February 3, 2014; VHA Directive 2010-008, dated February 22, 2010; VHA Directive 2010-014, dated March 25, 2010; VHA Directive 1009, dated August 28, 2013; VHA Directive 2010-010, dated March 2, 2010; VHA Directive 2011-029, dated July 15, 2011; and VHA Directive 2009-069, dated December 16, 2009 are rescinded. 6. RECERTIFICATION: This VHA directive is scheduled for recertification on or before the last working day of September 2021. -

Emergency Medical Services Statutes and Regulations
Emergency Medical Services Statutes and Regulations Printed: August 2016 Effective: September 11, 2016 1 9/16/2016 Statutes and Regulations Table of Contents Title 63 of the Oklahoma Statutes Pages 3 - 13 Sections 1-2501 to 1-2515 Constitution of Oklahoma Pages 14 - 16 Article 10, Section 9 C Title 19 of the Oklahoma Statutes Pages 17 - 24 Sections 371 and 372 Sections 1- 1201 to 1-1221 Section 1-1710.1 Oklahoma Administrative Code Pages 25 - 125 Chapter 641- Emergency Medical Services Subchapter 1- General EMS programs Subchapter 3- Ground ambulance service Subchapter 5- Personnel licenses and certification Subchapter 7- Training programs Subchapter 9- Trauma referral centers Subchapter 11- Specialty care ambulance service Subchapter 13- Air ambulance service Subchapter 15- Emergency medical response agency Subchapter 17- Stretcher aid van services Appendix 1 Summary of rule changes Approved changes to the June 11, 2009 effective date to the September 11, 2016 effective date 2 9/16/2016 §63-1-2501. Short title. Sections 1-2502 through 1-2521 of this title shall be known and may be cited as the "Oklahoma Emergency Response Systems Development Act". Added by Laws 1990, c. 320, § 5, emerg. eff. May 30, 1990. Amended by Laws 1999, c. 156, § 1, eff. Nov. 1, 1999. NOTE: Editorially renumbered from § 1-2401 of this title to avoid a duplication in numbering. §63-1-2502. Legislative findings and declaration. The Legislature hereby finds and declares that: 1. There is a critical shortage of providers of emergency care for: a. the delivery of fast, efficient emergency medical care for the sick and injured at the scene of a medical emergency and during transport to a health care facility, and b. -

Medical Emergency Minimum Standard: 5120:1-8-09(E) Revised
Section 6: Jail Emergencies Response Plan Subject: Medical Emergency Minimum Standard: 5120:1-8-09(E) Revised: Authorized: _____________________________ Effective date: ________________________ Sheriff Paul A. Sigsworth POLICY The Erie County Jail shall provide 24-hour emergency medical, dental, and mental health care services. All corrections officers are trained to respond to medical emergencies, and will promptly implement emergency medical procedures for inmates who are in need of emergency medical attention. PROCEDURE A. Policy 1. Any Corrections Officer or member of the Medical Staff who is available will respond when a Medical Emergency is reported and initiate care. B. Definitions: 1. The following occurrence define an emergency, which may result from, but not limited to, injury from attempted suicide or injury from assault. a. Sever Bleeding: i. Apply clean/sterile pressure dressing to wound, apply pressure by use of hands. Monitor for signs and symptoms of shock. Follow American Red Cross Heartsaver Guidelines. b. Unconsciousness: i. Maintain body alignment, observe vital signs, respiration, etc., for any change until the doctor or emergency squad arrives. Monitor for deteriorating status. Follow American Red Cross Heartsaver Guidelines. c. Serious Breathing Difficulties: i. Keep in a semi-sitting position. Loosen or remove all tight clothing, observe and reassure. Monitor for deteriorating status. Follow American Red Cross Heartsaver Guidelines. d. Head, Neck, and/or Spinal Injury: i. Keep inmate quiet. Stop any bleeding, maintain neck alignment, observe and reassure. Monitor for deteriorating status. Follow American Red Cross Heartsaver Guidelines. e. Severe Burns: i. Do not remove clothing. Apply clean wet dressing to area. Prevent chilling, observe and reassure. -

Best Airway and Ventilation Strategy During CPR and After Resuscitation
Best airway and ventilation strategy during CPR and after resuscitation After cardiac arrest a combination of basic and advanced airway and ventilation techniques are used during cardiopulmonary resuscitation (CPR) and after a return of spontaneous circulation (ROSC). Current guidelines are based predominantly on evidence from observational studies and expert consensus; thus, the optimal combination of airway techniques and oxygen and ventilation targets during CPR and after ROSC is uncertain, according to a review article in the journal Critical Care. Current evidence supports a stepwise approach to airway management based on patient factors, rescuer skills and the stage of resuscitation. Observational data suggest that early lay-bystander compression-only CPR can improve survival after sudden cardiac arrest. Chest compressions are easy to learn and do for most rescuers and do not require special equipment. Studies show that lay rescuer compression-only CPR is better than no CPR. During CPR, airway interventions range from compression-only CPR with or without airway opening, mouth-to-mouth ventilation, mouth-to-mask ventilation, bag-mask ventilation (with or without an oropharyngeal airway) or advanced airways (supraglottic airways [SGAs] and tracheal intubation using direct or video laryngoscopy). On arrival of trained rescuers, bag-mask ventilation with supplemental oxygen is the most common initial approach and can be aided with an oropharyngeal or nasopharyngeal airway. During CPR, the bag-mask is used to give two breaths after every 30 compressions. A pre-specified per-protocol analysis reported a significantly higher survival to discharge among those who actually received conventional CPR (30:2) compared with those who received continuous compressions.