Diazepam in the Treatment of Moderate to Severe Alcohol Withdrawal
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diazepam - Alcohol Withdrawal
Diazepam - alcohol withdrawal Why have I been prescribed diazepam? If a person stops drinking alcohol after a time of drinking too much they can experience withdrawal effects. These include “the shakes”, sweating, having fits, seeing things which are not there (hallucinations) and feeling anxious and low in mood. They can feel wound up and find it difficult to sleep. These withdrawal effects can be very uncomfortable and in extreme cases can be dangerous if they persist into “DTs” (delirium tremens). Diazepam is used to help reduce these withdrawal symptoms. It relieves anxiety and tension and aids sleep. Diazepam can also prevent fits. It controls the withdrawal symptoms until the body is free of alcohol and has settled down. This usually takes three to seven days from the time you stop drinking. What exactly is diazepam? Diazepam is a benzodiazepine. This group of medicines is also called anxiolytics or minor tranquillisers. Diazepam has many uses. It can be used to reduce symptoms of anxiety and insomnia, as well as to help people come off alcohol. Diazepam should only be prescribed and taken as a short course. Is diazepam safe to take? Diazepam is safe to take for a short period of time, but it doesn’t suit everyone. Below are a few conditions where diazepam may be less suitable. If any of these apply to you please tell your doctor or key-worker. If you have depression or a mental illness If you have lung disease or breathing problems, or suffer from liver or kidney trouble If you take any other medicines or drugs, including those on prescription and bought from a chemist If you take illicit drugs bought “on the street” If you are pregnant or breast-feeding What is the usual dose of diazepam? The dose of diazepam will usually be started at 10-20mg four times a day. -
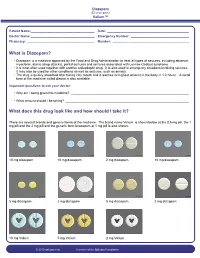
What Is Diazepam?
Diazepam (Di-a-ze-pam) Valium™ Patient Name: ___________________________________ Date: _____________________________________________ Doctor Name: ___________________________________ Emergency Number: ________________________________ Pharmacy: _____________________________________ Number: __________________________________________ What is Diazepam? • Diazepam is a medicine approved by the Food and Drug Administration to treat all types of seizures, including absence, myoclonic, atonic (drop attacks), partial seizures and seizures associated with Lennox-Gastaut syndrome. • It is most often used together with another antiepileptic drug. It is also used in emergency situations involving seizures. It may also be used for other conditions as well as seizures, such as anxiety. • The drug is quickly absorbed after taking it by mouth and it reaches its highest amount in the body in 1-2 hours. A rectal form of the medicine called diastat is also available. Important questions to ask your doctor: • Why am I being given this medicine? _________________________________________________________________ • What amount should I be taking? ____________________________________________________________________ What does this drug look like and how should I take it? There are several brands and generic forms of the medicine. The brand name Valium is shown below at the 0.5 mg pill, the 1 mg pill and the 2 mg pill and the generic form lorazepam at 1 mg pill is also shown. 10 mg diazepam 10 mg diazepam 2 mg diazepam 10 mg diazepam 5 mg diazepam 2 mg diazepam 5 mg diazepam 2 mg diazepam 10 mg Valium 5 mg Valium 2 mg Valium © 2010 epilepsy.com A service of the Epilepsy Foundation Diazepam (Di-a-ze-pam) Valium™ Frequently Asked Questions: How do I take Diazepam? To use the tablet form: chew tablets and swallow or swallow the tablet whole. -

Drug and Alcohol Withdrawal Clinical Practice Guidelines - NSW
Guideline Drug and Alcohol Withdrawal Clinical Practice Guidelines - NSW Summary To provide the most up-to-date knowledge and current level of best practice for the treatment of withdrawal from alcohol and other drugs such as heroin, and other opioids, benzodiazepines, cannabis and psychostimulants. Document type Guideline Document number GL2008_011 Publication date 04 July 2008 Author branch Centre for Alcohol and Other Drugs Branch contact (02) 9424 5938 Review date 18 April 2018 Policy manual Not applicable File number 04/2766 Previous reference N/A Status Active Functional group Clinical/Patient Services - Pharmaceutical, Medical Treatment Population Health - Pharmaceutical Applies to Area Health Services/Chief Executive Governed Statutory Health Corporation, Board Governed Statutory Health Corporations, Affiliated Health Organisations, Affiliated Health Organisations - Declared Distributed to Public Health System, Ministry of Health, Public Hospitals Audience All groups of health care workers;particularly prescribers of opioid treatments Secretary, NSW Health Guideline Ministry of Health, NSW 73 Miller Street North Sydney NSW 2060 Locked Mail Bag 961 North Sydney NSW 2059 Telephone (02) 9391 9000 Fax (02) 9391 9101 http://www.health.nsw.gov.au/policies/ space space Drug and Alcohol Withdrawal Clinical Practice Guidelines - NSW space Document Number GL2008_011 Publication date 04-Jul-2008 Functional Sub group Clinical/ Patient Services - Pharmaceutical Clinical/ Patient Services - Medical Treatment Population Health - Pharmaceutical -

Understanding Benzodiazephine Use, Abuse, and Detection
Siemens Healthcare Diagnostics, the leading clinical diagnostics company, is committed to providing clinicians with the vital information they need for the accurate diagnosis, treatment and monitoring of patients. Our comprehensive portfolio of performance-driven systems, unmatched menu offering and IT solutions, in conjunction with highly responsive service, is designed to streamline workflow, enhance operational efficiency and support improved patient care. Syva, EMIT, EMIT II, EMIT d.a.u., and all associated marks are trademarks of General Siemens Healthcare Diagnostics Inc. All Drugs other trademarks and brands are the Global Division property of their respective owners. of Abuse Siemens Healthcare Product availability may vary from Diagnostics Inc. country to country and is subject 1717 Deerfield Road to varying regulatory requirements. Deerfield, IL 60015-0778 Please contact your local USA representative for availability. www.siemens.com/diagnostics Siemens Global Headquarters Global Siemens Healthcare Headquarters Siemens AG Understanding Wittelsbacherplatz 2 Siemens AG 80333 Muenchen Healthcare Sector Germany Henkestrasse 127 Benzodiazephine Use, 91052 Erlangen Germany Abuse, and Detection Telephone: +49 9131 84 - 0 www.siemens.com/healthcare www.usa.siemens.com/diagnostics Answers for life. Order No. A91DX-0701526-UC1-4A00 | Printed in USA | © 2009 Siemens Healthcare Diagnostics Inc. Syva has been R1 R2 a leading developer N and manufacturer of AB R3 X N drugs-of-abuse tests R4 for more than 30 years. R2 C Now part of Siemens Healthcare ® Diagnostics, Syva boasts a long and Benzodiazepines have as their basic chemical structure successful track record in drugs-of-abuse a benzene ring fused to a seven-membered diazepine ring. testing, and leads the industry in the All important benzodiazepines contain a 5-aryl substituent ring (ring C) and a 1,4–diazepine ring. -

Risk Based Requirements for Medicines Handling
Risk based requirements for medicines handling Including requirements for Schedule 4 Restricted medicines Contents 1. Introduction 2 2. Summary of roles and responsibilities 3 3. Schedule 4 Restricted medicines 4 4. Medicines acquisition 4 5. Storage of medicines, including control of access to storage 4 5.1. Staff access to medicines storage areas 5 5.2. Storage of S4R medicines 5 5.3. Storage of S4R medicines for medical emergencies 6 5.4. Access to storage for S4R and S8 medicines 6 5.5. Pharmacy Department access, including after hours 7 5.6. After-hours access to S8 medicines in the Pharmacy Department 7 5.7. Storage of nitrous oxide 8 5.8. Management of patients’ own medicines 8 6. Distribution of medicines 9 6.1. Distribution outside Pharmacy Department operating hours 10 6.2. Distribution of S4R and S8 medicines 10 7. Administration of medicines to patients 11 7.1. Self-administration of scheduled medicines by patients 11 7.2. Administration of S8 medicines 11 8. Supply of medicines to patients 12 8.1. Supply of scheduled medicines to patients by health professionals other than pharmacists 12 9. Record keeping 13 9.1. General record keeping requirements for S4R medicines 13 9.2. Management of the distribution and archiving of S8 registers 14 9.3. Inventories of S4R medicines 14 9.4. Inventories of S8 medicines 15 10. Destruction and discards of S4R and S8 medicines 15 11. Management of oral liquid S4R and S8 medicines 16 12. Cannabis based products 17 13. Management of opioid pharmacotherapy 18 14. -

Benzodiazepines: Uses and Risks Charlie Reznikoff, MD Hennepin Healthcare
Benzodiazepines: Uses and Risks Charlie Reznikoff, MD Hennepin healthcare 4/22/2020 Overview benzodiazepines • Examples of benzos and benzo like drugs • Indications for benzos • Pharmacology of benzos • Side effects and contraindications • Benzo withdrawal • Benzo tapers 12/06/2018 Sedative/Hypnotics • Benzodiazepines • Alcohol • Z-drugs (Benzo-like sleeping aids) • Barbiturates • GHB • Propofol • Some inhalants • Gabapentin? Pregabalin? 12/06/2018 Examples of benzodiazepines • Midazolam (Versed) • Triazolam (Halcion) • Alprazolam (Xanax) • Lorazepam (Ativan) • Temazepam (Restoril) • Oxazepam (Serax) • Clonazepam (Klonopin) • Diazepam (Valium) • Chlordiazepoxide (Librium) 4/22/2020 Sedatives: gaba stimulating drugs have incomplete “cross tolerance” 12/06/2018 Effects from sedative (Benzo) use • Euphoria/bliss • Suppresses seizures • Amnesia • Muscle relaxation • Clumsiness, visio-spatial impairment • Sleep inducing • Respiratory suppression • Anxiolysis/disinhibition 12/06/2018 Tolerance to benzo effects? • Effects quickly diminish with repeated use (weeks) • Euphoria/bliss • Suppresses seizures • Effects incompletely diminish with repeated use • Amnesia • Muscle relaxation • Clumsiness, visio-spatial impairment • Seep inducing • Durable effects with repeated use • Respiratory suppression • Anxiolysis/disinhibition 12/06/2018 If you understand this pharmacology you can figure out the rest... • Potency • 1 mg diazepam <<< 1 mg alprazolam • Duration of action • Half life differences • Onset of action • Euphoria, clinical utility in acute -

Benzodiazepines
Benzodiazepines Using benzodiazepines in Children and Adolescents Overview Benzodiazepines are group of medications used to treat several different conditions. Some examples of these medications include: lorazepam (Ativan®); clonazepam (Rivotril®); alprazolam (Xanax®) and oxazepam (Serax®). Other benzodiazepine medications are available, but are less commonly used in children and adolescents. What are benzodiazepines used for? Benzodiazepines may be used for the following conditions: • anxiety disorders: generalized anxiety disorder; social anxiety disorder; post-traumatic stress disorder (PTSD); panic attacks/disorder; excessive anxiety prior to surgery • sleep disorders: trouble sleeping (insomnia); waking up suddenly with great fear (night terrors); sleepwalking • seizure disorders (epilepsy) • alcohol withdrawal • treatment of periods of extreme slowing or excessive purposeless motor activity (catatonia) Your doctor may be using this medication for another reason. If you are unclear why this medication is being prescribed, please ask your doctor. How do benzodiazepines work? Benzodiazepines works by affecting the activity of the brain chemical (neurotransmitter) called GABA. By enhancing the action of GABA, benzodiazepines have a calming effect on parts of the brain that are too excitable. This in turn helps to manage anxiety, insomnia, and seizure disorders. How well do benzodiazepines work in children and adolescents? When used to treat anxiety disorders, benzodiazepines decrease symptoms such as nervousness, fear, and excessive worrying. Benzodiazepines may also help with the physical symptoms of anxiety, including fast or strong heart beat, trouble breathing, dizziness, shakiness, sweating, and restlessness. Typically, benzodiazepines are prescribed to manage anxiety symptoms that are uncomfortable, frightening or interfere with daily activities for a short period of time before conventional anti-anxiety treatments like cognitive-behavioural therapy or anti-anxiety takes effect. -

Midazolam Injection, USP
Midazolam Injection, USP 2 mg per 2 mL | NDC 70860-600-02 50 mg per 10 mL | NDC 70860-601-10 ATHENEX AccuraSEETM PACKAGING AND LABELING BIG, BOLD AND BRIGHT — TO HELP YOU SEE IT, SAY IT AND PICK IT RIGHT DIFFERENTIATION IN EVERY LABEL, DESIGNED TO HELP REDUCE MEDICATION ERRORS PLEASE SEE FULL PRESCRIBING INFORMATION, INCLUDING BOXED WARNING, FOR MIDAZOLAM INJECTION, USP, ENCLOSED. THE NEXT GENERATION OF PHARMACY INNOVATION To order, call 1-855-273-0154 or visit www.Athenexpharma.com Midazolam Injection, USP 2 5 mg NDC 70860-600-02 0 NDC 70860-601-10 2 mg per 2 mL mg 50 mg per 10 mL DESCRIPTION Glass Vial DESCRIPTION Glass Vial CONCENTRATION 1 mg per mL CONCENTRATION 5 mg per mL CLOSURE 13 mm CLOSURE 20 mm UNIT OF SALE 25 vials UNIT OF SALE 10 vials BAR CODED Yes BAR CODED Yes STORAGE Room Temp. STORAGE Room Temp. • AP RATED • PRESERVATIVE-FREE • AP RATED • NOT MADE WITH NATURAL RUBBER LATEX • NOT MADE WITH NATURAL RUBBER LATEX CHOOSE AccuraSEETM FOR YOUR PHARMACY Our proprietary, differentiated and highly-visible label designs can assist pharmacists in accurate medication selection. With a unique label design for every Athenex product, we’re offering your pharmacy added AccuraSEE. The idea is simple: “So what you see is exactly what you get.” Athenex, AccuraSEE and all label designs are copyright of Athenex. ©2020 Athenex. 000527 To order, call 1-855-273-0154 or visit www.Athenexpharma.com • Midazolam hydrochloride mufti-dose vial, is not intended for intrathecal or epidural • Anesthetic and sedation drugs are a necessary part of the care of children needing Midazolam Injection, USP administration, and is contraindicated for use in premature infants, because the formulation surgery, other procedures, or tests that cannot be delayed, and no specific medications INDICATIONS AND USAGE contains benzyl alcohol as a preservative. -

Benzodiazepine Group ELISA Kit
Benzodiazepine Group ELISA Kit Benzodiazepine Background Since their introduction in the 1960s, benzodiazepines have been widely prescribed for the treatment of anxiety, insomnia, muscle spasms, alcohol withdrawal, and seizure-prevention as they are depressants of the central nervous system. Despite the fact that they are highly effective for their intended use, benzodiazepines are prescribed with caution as they can be highly addictive. In fact, researchers at NIDA (National Institute on Drug Abuse) have shown that addiction for benzodiazepines is similar to that of opioids, cannabinoids, and GHB. Common street names of benzodiazepines include “Benzos” and “Downers”. The five most encountered benzodiazepines on the illicit market are alprazolam (Xanax), lorazepam (Ativan), clonazepam (Klonopin), diazepam (Valium), and temazepam (Restori). The method of abuse is typically oral or snorted in crushed form. The DEA notes a particularly high rate of abuse among heroin and cocaine abusers. Designer benzodiazepines are currently offered in online shops selling “research chemicals”, providing drug abusers an alternative to prescription-only benzodiazepines. Data defining pharmacokinetic parameters, drug metabolisms, and detectability in biological fluids is limited. This lack of information presents a challenge to forensic laboratories. Changes in national narcotics laws in many countries led to the control of (phenazepam and etizolam), which were marketed by pharmaceutical companies in some countries. With the control of phenazepam and etizolam, clandestine laboratories have begun researching and manufacturing alternative benzodiazepines as legal substitutes. Delorazepam, diclazepam, pyrazolam, and flubromazepam have emerged as compounds in this class of drugs. References Drug Enforcement Administration, Office of Diversion Control. “Benzodiazepines.” http://www.deadiversion.usdoj.gov/drugs_concern/benzo_1. -

Acute Migraine Treatment
Acute Migraine Treatment Morris Levin, MD Professor of Neurology Director, Headache Center UCSF Department of Neurology San Francisco, CA Mo Levin Disclosures Consulting Royalties Allergan Oxford University Press Supernus Anadem Press Amgen Castle Connolly Med. Publishing Lilly Wiley Blackwell Mo Levin Disclosures Off label uses of medication DHE Antiemetics Zolmitriptan Learning Objectives At the end of the program attendees will be able to 1. List all important options in the acute treatment of migraine 2. Discuss the evidence and guidelines supporting the major migraine acute treatment options 3. Describe potential adverse effects and medication- medication interactions in acute migraine pharmacological treatment Case 27 y/o woman has suffered ever since she can remember from “sick headaches” . Pain is frontal, increases over time and is generally accompanied by nausea and vomiting. She feels depressed. The headache lasts the rest of the day but after sleeping through the night she awakens asymptomatic 1. Diagnosis 2. Severe Headache relief Diagnosis: What do we need to beware of? • Misdiagnosis of primary headache • Secondary causes of headache Red Flags in HA New (recent onset or change in pattern) Effort or Positional Later onset than usual (middle age or later) Meningismus, Febrile AIDS, Cancer or other known Systemic illness - Neurological or psych symptoms or signs Basic principles of Acute Therapy of Headaches • Diagnose properly, including comorbid conditions • Stratify therapy rather than treat in steps • Treat early -
Accurate Measurement, and Validation of Solubility Data † ‡ ‡ § † ‡ Víctor R
Article Cite This: Cryst. Growth Des. 2019, 19, 4101−4108 pubs.acs.org/crystal In the Context of Polymorphism: Accurate Measurement, and Validation of Solubility Data † ‡ ‡ § † ‡ Víctor R. Vazqueź Marrero, , Carmen Piñero Berríos, , Luz De Dios Rodríguez, , ‡ ∥ ‡ § Torsten Stelzer,*, , and Vilmalí Lopez-Mej́ ías*, , † Department of Biology, University of Puerto RicoRío Piedras Campus, San Juan, Puerto Rico 00931, United States ‡ Crystallization Design Institute, Molecular Sciences Research Center, University of Puerto Rico, San Juan, Puerto Rico 00926, United States § Department of Chemistry, University of Puerto RicoRío Piedras Campus, San Juan, Puerto Rico 00931, United States ∥ Department of Pharmaceutical Sciences, University of Puerto RicoMedical Sciences Campus, San Juan, Puerto Rico 00936, United States *S Supporting Information ABSTRACT: Solubility measurements for polymorphic com- pounds are often accompanied by solvent-mediated phase transformations. In this study, solubility measurements from undersaturated solutions are employed to investigate the solubility of the two most stable polymorphs of flufenamic acid (FFA forms I and III), tolfenamic acid (TA forms I and II), and the only known form of niflumic acid (NA). The solubility was measured from 278.15 to 333.15 K in four alcohols of a homologous series (methanol, ethanol, 1- propanol, n-butanol) using the polythermal method. It was established that the solubility of these compounds increases with increasing temperature. The solubility curves of FFA forms I and III intersect at ∼315.15 K (42 °C) in all four solvents, which represents the transition temperature of the enantiotropic pair. In the case of TA, the solubility of form II could not be reliably obtained in any of the solvents because of the fast solvent- mediated phase transformation. -

S1 Table. List of Medications Analyzed in Present Study Drug
S1 Table. List of medications analyzed in present study Drug class Drugs Propofol, ketamine, etomidate, Barbiturate (1) (thiopental) Benzodiazepines (28) (midazolam, lorazepam, clonazepam, diazepam, chlordiazepoxide, oxazepam, potassium Sedatives clorazepate, bromazepam, clobazam, alprazolam, pinazepam, (32 drugs) nordazepam, fludiazepam, ethyl loflazepate, etizolam, clotiazepam, tofisopam, flurazepam, flunitrazepam, estazolam, triazolam, lormetazepam, temazepam, brotizolam, quazepam, loprazolam, zopiclone, zolpidem) Fentanyl, alfentanil, sufentanil, remifentanil, morphine, Opioid analgesics hydromorphone, nicomorphine, oxycodone, tramadol, (10 drugs) pethidine Acetaminophen, Non-steroidal anti-inflammatory drugs (36) (celecoxib, polmacoxib, etoricoxib, nimesulide, aceclofenac, acemetacin, amfenac, cinnoxicam, dexibuprofen, diclofenac, emorfazone, Non-opioid analgesics etodolac, fenoprofen, flufenamic acid, flurbiprofen, ibuprofen, (44 drugs) ketoprofen, ketorolac, lornoxicam, loxoprofen, mefenamiate, meloxicam, nabumetone, naproxen, oxaprozin, piroxicam, pranoprofen, proglumetacin, sulindac, talniflumate, tenoxicam, tiaprofenic acid, zaltoprofen, morniflumate, pelubiprofen, indomethacin), Anticonvulsants (7) (gabapentin, pregabalin, lamotrigine, levetiracetam, carbamazepine, valproic acid, lacosamide) Vecuronium, rocuronium bromide, cisatracurium, atracurium, Neuromuscular hexafluronium, pipecuronium bromide, doxacurium chloride, blocking agents fazadinium bromide, mivacurium chloride, (12 drugs) pancuronium, gallamine, succinylcholine