Heat Response Plans: Summary of Evidence and Strategies for Collaboration and Implementation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Heat Wave Safety Tips
Heat Wave Safety Tips KNOW THE FACTS Heat waves usually consist of high temperatures and high relative humidity. This combination makes it difficult for the human body to dissipate heat through the skin and sweat glands. Sweating will not cool the human body unless the water is removed by evaporation. High relative humidity, consequently, retards evaporation. Certain medications can also make it difficult for a person to sweat. Heat Index… The National Weather Service (NWS) uses the "HEAT INDEX" as a measure of the combined affects of high temperatures and high relative humidity. Research findings strongly suggest that HEAT INDEX (HI) values of 90 to 105 degrees make sunstroke, heat cramps, and heat exhaustion possible with prolonged exposure and/or physical activity. Research findings strongly suggest that HI vales of 105 to 130 degrees make sunstroke, heat cramps, and heat exhaustion likely with prolonged exposure and/or physical activity. Advisories and warnings… The NWS issues Heat Advisories when it expects daytime HI's to equal or exceed 105 degrees for 3 hours or more while nighttime HI's equal or exceed 80 degrees, for any 24- hour period. The NWS issues Excessive Heat Warnings when it expects daytime HI's to equal or exceed 115 degrees for 3 hours or more while nighttime HI's equal or exceed 80 degrees, for any 24-hour period. The NWS may issue an "Excessive Heat Watch" 24 to 8 hours in advance of heat wave conditions. DURING THE HEAT Listen to your NOAA Weather Radio… Stay informed about the latest watches, warnings, and advisories. -

EXTREME HEAT TOOLKIT a Planning Guide for Public Health and Emergency Response Professionals
EXTREME HEAT TOOLKIT A planning guide for public health and emergency response professionals WISCONSIN CLIMATE AND HEALTH PROGRAM Bureau of Environmental and Occupational Health dhs.wisconsin.gov/climate | [email protected] State of Wisconsin | Department of Health Services | Division of Public Health | P-00632 (Rev. 04/2019) 1 CONTENTS Introduction Definitions Guides Guide 1: Definitions of Heat Alerts Guide 2: Heat Illnesses and Symptoms Guide 3: Extreme Heat Tips Guide 4: Populations Vulnerable to Heat Guide 5: Talking Points for Heat-Related Fatality Guide 6: Message Maps about Heat-Related Safety Guide 7: Long-Term Preparation Checklist Guide 8: Anticipation of Imminent Heat Event Checklist Guide 9: Extreme Heat Event Response Checklist Appendices Appendix A: References Appendix B: Additional Resources Appendix C: Sample Heat Response Plan ACKNOWLEDGEMENTS The Wisconsin Extreme Heat Toolkit was made possible through funding from cooperative agreement 5UE1/ EH001043-02 from the Centers for Disease Control and Prevention (CDC) and the commitment of many individuals at the Wisconsin Department of Health Services (DHS) who contributed their valuable time and knowledge to its development. Special thanks to: Jeffrey Phillips, RS, Director of the Bureau of Environmental and Occupational Health, DHS Megan Christenson, MS, MPH, Epidemiologist, DHS Brooke Thompson, MPH, Healthy Homes Program Manager, DHS Stephanie Krueger, Public Health Associate, CDC/ DHS Eleanor Ganz, BRACE Toolkits Intern, DHS For more information, please contact: Colleen Moran, MS, MPH Climate and Health Program Manager Bureau of Environmental and Occupational Health 1 W. Wilson St., Room 150 Madison, WI 53703 [email protected] 608-266-6761 2 INTRODUCTION Purpose The purpose of this Extreme Heat Toolkit is to provide information to local governments, health departments, and citizens about preparing for and responding to heat events. -
National Weather Service Reference Guide
National Weather Service Reference Guide Purpose of this Document he National Weather Service (NWS) provides many products and services which can be T used by other governmental agencies, Tribal Nations, the private sector, the public and the global community. The data and services provided by the NWS are designed to fulfill us- ers’ needs and provide valuable information in the areas of weather, hydrology and climate. In addition, the NWS has numerous partnerships with private and other government entities. These partnerships help facilitate the mission of the NWS, which is to protect life and prop- erty and enhance the national economy. This document is intended to serve as a reference guide and information manual of the products and services provided by the NWS on a na- tional basis. Editor’s note: Throughout this document, the term ―county‖ will be used to represent counties, parishes, and boroughs. Similarly, ―county warning area‖ will be used to represent the area of responsibility of all of- fices. The local forecast office at Buffalo, New York, January, 1899. The local National Weather Service Office in Tallahassee, FL, present day. 2 Table of Contents Click on description to go directly to the page. 1. What is the National Weather Service?…………………….………………………. 5 Mission Statement 6 Organizational Structure 7 County Warning Areas 8 Weather Forecast Office Staff 10 River Forecast Center Staff 13 NWS Directive System 14 2. Non-Routine Products and Services (watch/warning/advisory descriptions)..…….. 15 Convective Weather 16 Tropical Weather 17 Winter Weather 18 Hydrology 19 Coastal Flood 20 Marine Weather 21 Non-Precipitation 23 Fire Weather 24 Other 25 Statements 25 Other Non-Routine Products 26 Extreme Weather Wording 27 Verification and Performance Goals 28 Impact-Based Decision Support Services 30 Requesting a Spot Fire Weather Forecast 33 Hazardous Materials Emergency Support 34 Interactive Warning Team 37 HazCollect 38 Damage Surveys 40 Storm Data 44 Information Requests 46 3. -

Hazard Criteria
NWS San Diego All-Hazard Reference Guide Warnings and Advisories are issued 12 to 48 hours in advance. Watches are issued when warning level conditions are forecast within the next 36 to 48 hours, or up to 72 hours with high confidence. High Winds/Blowing Dust Blowing High Wind Dust Storm Region Wind Advisory Dust Warning Warning Advisory Coastal and Sustained ≥ 30 mph Sustained ≥ 40 mph Visibility Visibility Valley areas or gust ≥ 35 mph gust ≥ 58 mph ¼ to 1 mile <¼ mile Mountains and Sustained ≥ 35 mph Sustained ≥ 45 mph Visibility Visibility Deserts or gust ≥ 40 mph or gust ≥ 58 mph ¼ to 1 mile <¼ mile < 7000 feet Mountains Sustained ≥ 40 mph Sustained ≥ 40 mph Visibility Visibility > 7000 feet or gust ≥ 55 mph or gust ≥ 75 mph ¼ to 1 mile <¼ mile Winter Weather Winter Winter Blizzard Wind Chill Wind Chill Region Weather Storm Warning Advisory Warning Advisory Warning 4-8” in Sustained winds Wind Chill 12” in 12 hours, Wind Chill Mountains 12 hours, > 35 mph and Temperatures 18” in 24 hours, Temperatures > 7000 feet or 8-12” in visibility <¼ mile from High Impact < -20 ◦F 24 hours in blowing snow -10 to -20 ◦F 3-6” in Sustained winds Wind Chill Mountains 8” in 12 hours, Wind Chill 12 hours, > 35 mph and Temperatures 3000 to 12” in 24 hours, Temperatures 4-8” in visibility <¼ mile from 7000 feet High Impact < -20 ◦F 24 hours in blowing snow -10 to -20 ◦F Other areas 1-4” in Sustained winds Wind Chill including 4” in 12 hours, Wind Chill 12 hours, > 35 mph and Temperatures High 6” in 24 hours, Temperatures 3-6” in visibility <¼ mile -

Let Me Just Add That While the Piece in Newsweek Is Extremely Annoying
From: Michael Oppenheimer To: Eric Steig; Stephen H Schneider Cc: Gabi Hegerl; Mark B Boslough; [email protected]; Thomas Crowley; Dr. Krishna AchutaRao; Myles Allen; Natalia Andronova; Tim C Atkinson; Rick Anthes; Caspar Ammann; David C. Bader; Tim Barnett; Eric Barron; Graham" "Bench; Pat Berge; George Boer; Celine J. W. Bonfils; James A." "Bono; James Boyle; Ray Bradley; Robin Bravender; Keith Briffa; Wolfgang Brueggemann; Lisa Butler; Ken Caldeira; Peter Caldwell; Dan Cayan; Peter U. Clark; Amy Clement; Nancy Cole; William Collins; Tina Conrad; Curtis Covey; birte dar; Davies Trevor Prof; Jay Davis; Tomas Diaz De La Rubia; Andrew Dessler; Michael" "Dettinger; Phil Duffy; Paul J." "Ehlenbach; Kerry Emanuel; James Estes; Veronika" "Eyring; David Fahey; Chris Field; Peter Foukal; Melissa Free; Julio Friedmann; Bill Fulkerson; Inez Fung; Jeff Garberson; PETER GENT; Nathan Gillett; peter gleckler; Bill Goldstein; Hal Graboske; Tom Guilderson; Leopold Haimberger; Alex Hall; James Hansen; harvey; Klaus Hasselmann; Susan Joy Hassol; Isaac Held; Bob Hirschfeld; Jeremy Hobbs; Dr. Elisabeth A. Holland; Greg Holland; Brian Hoskins; mhughes; James Hurrell; Ken Jackson; c jakob; Gardar Johannesson; Philip D. Jones; Helen Kang; Thomas R Karl; David Karoly; Jeffrey Kiehl; Steve Klein; Knutti Reto; John Lanzante; [email protected]; Ron Lehman; John lewis; Steven A. "Lloyd (GSFC-610.2)[R S INFORMATION SYSTEMS INC]"; Jane Long; Janice Lough; mann; [email protected]; Linda Mearns; carl mears; Jerry Meehl; Jerry Melillo; George Miller; Norman Miller; Art Mirin; John FB" "Mitchell; Phil Mote; Neville Nicholls; Gerald R. North; Astrid E.J. Ogilvie; Stephanie Ohshita; Tim Osborn; Stu" "Ostro; j palutikof; Joyce Penner; Thomas C Peterson; Tom Phillips; David Pierce; [email protected]; V. -

Wet%Bulb%Temperature%
It’s not just the heat, it’s the humidity. Downscaled Wet-Bulb Temperature Projections and Implication for Future Summer Experiences from the American Climate Prospectus D.J. RasmussenPROJECT DESCRIPTION RhodiumAn Group American Climate Risk Assessment Next Generation, in collaboration with Bloomberg Philanthropies and the Economic Risks of Climate Change: An American Prospectus Paulson Institute, has asked Rhodium Group (RHG) to convene a team of climate scientists and economists to assess the risk to the US economy of global climate Trevor Houser Solomon Hsiang Robert Kopp change. ThisKate assessment, Larsen to conclude in late spring 2014,will combine a review Rhodium Group UC Berkeley Rutgers Universityof existing literatureRhodium Group on the current and potential impacts of climate change in Michael Delgado Amir Jina Michael Mastrandreathe United StatesShashank with Mohan original research quantifying the potential economic Rhodium Group Columbia University Stanford Universitycosts of the rangeRhodium of Group possible climate futures Americans now face. The report Robert Muir-Wood DJ Rasmussen James Rising will inform thePaul work Wilson of a high-level and bipartisan climate risk committee co- RMS Rhodium Group Columbia Universitychaired by MayorRMS Bloomberg, Secretary Paulson and Tom Steyer. Supported by the Risky Business Project • Forthcoming from ColumbiaBACKGROUND University Press, AND SpringCONTEXT 2015 See abstracts: U13A-01, GC23F-03, PA24A-02, U31A-01, GC32A-07,From Superstorm GC41B-0549, Sandy to Midwest droughts to -

The Report: Killer Heat in the United States
Killer Heat in the United States Climate Choices and the Future of Dangerously Hot Days Killer Heat in the United States Climate Choices and the Future of Dangerously Hot Days Kristina Dahl Erika Spanger-Siegfried Rachel Licker Astrid Caldas John Abatzoglou Nicholas Mailloux Rachel Cleetus Shana Udvardy Juan Declet-Barreto Pamela Worth July 2019 © 2019 Union of Concerned Scientists The Union of Concerned Scientists puts rigorous, independent All Rights Reserved science to work to solve our planet’s most pressing problems. Joining with people across the country, we combine technical analysis and effective advocacy to create innovative, practical Authors solutions for a healthy, safe, and sustainable future. Kristina Dahl is a senior climate scientist in the Climate and Energy Program at the Union of Concerned Scientists. More information about UCS is available on the UCS website: www.ucsusa.org Erika Spanger-Siegfried is the lead climate analyst in the program. This report is available online (in PDF format) at www.ucsusa.org /killer-heat. Rachel Licker is a senior climate scientist in the program. Cover photo: AP Photo/Ross D. Franklin Astrid Caldas is a senior climate scientist in the program. In Phoenix on July 5, 2018, temperatures surpassed 112°F. Days with extreme heat have become more frequent in the United States John Abatzoglou is an associate professor in the Department and are on the rise. of Geography at the University of Idaho. Printed on recycled paper. Nicholas Mailloux is a former climate research and engagement specialist in the Climate and Energy Program at UCS. Rachel Cleetus is the lead economist and policy director in the program. -
Write a Better Book Other Martial Artists Will Buy and Read
© 2013 Kris Wilder & Lawrence Kane Page 1 Don’t Write That Book: Write a better book other martial artists will buy and read Kris Wilder and Lawrence Kane © 2013 Kris Wilder & Lawrence Kane Page 2 © 2013 Kris Wilder & Lawrence Kane Page 3 © 2013 Kris Wilder & Lawrence Kane Page 4 “Build it and they will come.” — From the movie Field of Dreams “‘Build it and they will come’ is the greatest lie ever propagated on potential authors.” — Kris Wilder Introduction The belief that if you build it they will come is a complete and utter fallacy, especially when it comes to publishing. Unfortunately thousands upon thousands of authors across the world pour their blood, sweat, and tears (sometimes literally) into their work based upon this myth. Without proper preparation and promotion even the best book on the planet will be read by few and purchased by less. It takes forethought to navigate the world of publishing and deliver a product that will actually reach its intended audience. Let’s take a look at the entertainment industry for a comparison that illustrates this point. One of the most successful television shows of all time was Seinfeld. Seinfeld, however, had poor ratings in its first season and faced the very real possibility of cancellation. Nevertheless the network took a risk, promoted the heck out of the show and, well… the rest is history. But this success did not come lightly. It required good casting, solid storylines, and witty dialogue in addition to a well thought out advertising campaign. Another TV show that you might be familiar with, Firefly, had all the same strengths of casting, storylines, and dialogue. -
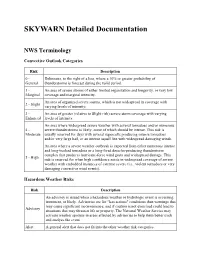
SKYWARN Detailed Documentation
SKYWARN Detailed Documentation NWS Terminology Convective Outlook Categories Risk Description 0 - Delineates, to the right of a line, where a 10% or greater probability of General thunderstorms is forecast during the valid period. 1 - An area of severe storms of either limited organization and longevity, or very low Marginal coverage and marginal intensity. An area of organized severe storms, which is not widespread in coverage with 2 - Slight varying levels of intensity. 3 - An area of greater (relative to Slight risk) severe storm coverage with varying Enhanced levels of intensity. An area where widespread severe weather with several tornadoes and/or numerous 4 - severe thunderstorms is likely, some of which should be intense. This risk is Moderate usually reserved for days with several supercells producing intense tornadoes and/or very large hail, or an intense squall line with widespread damaging winds. An area where a severe weather outbreak is expected from either numerous intense and long-tracked tornadoes or a long-lived derecho-producing thunderstorm complex that produces hurricane-force wind gusts and widespread damage. This 5 - High risk is reserved for when high confidence exists in widespread coverage of severe weather with embedded instances of extreme severe (i.e., violent tornadoes or very damaging convective wind events). Hazardous Weather Risks Risk Description An advisory is issued when a hazardous weather or hydrologic event is occurring, imminent, or likely. Advisories are for "less serious" conditions than warnings that may cause significant inconvenience, and if caution is not exercised could lead to Advisory situations that may threaten life or property. The National Weather Service may activate weather spotters in areas affected by advisories to help them better track and analyze the event. -

Inclement Weather Guidelines for Outdoor Events
INCLEMENT WEATHER GUIDELINES FOR OUTDOOR EVENTS “Inclement weather” is a generic term often used to describe weather conditions that are either unsafe or undesirable for outdoor events. Inclement weather can come in many different forms, as outlined below. This guideline is intended to be used as a tool to help you identify when forecasted or actual weather conditions require cancelling or postponing an event. NOTE: This checklist addresses only the most unsafe weather conditions. Your own event guidelines may dictate actions for other weather conditions that may be undesirable (e.g. rainy, too warm, too cold). Should any of the following triggers occur or become forecasted for the time of the event, the event should be cancelled or, when appropriate, temporarily postponed for safety reasons. Temporarily postponing an event means just waiting a few minutes until the immediate hazard passes, if your schedule allows. When in doubt about what to do, consult with FSU Emergency Management for decision support. ADVANCED NOTICE TRIGGER TO CANCEL EVENT: TRIGGER TO TEMPORARILY POSTPONE TIMEFRAME EVENT: 0 ‐ 48 Hours [ ] Hurricane or Tropical Storm Watch [ ] Winter Storm Watch 0 ‐ 24 Hours [ ] Heat Advisory or Excessive Heat Watch [ ] High Wind Watch [ ] Winter Weather Advisory [ ] Wind Chill Advisory 0 ‐ 12 Hours [ ] Tornado Watch [ ] Severe Thunderstorm Watch [ ] Flash Flood Watch [ ] Excessive Heat Warning [ ] Wind Advisory During Event [ ] Observed Heat Index in excess of 108’F. [ ] FSU ALERT issued for Tornado Warning, Severe Thunderstorm Warning, Flash Flood Warning or [ ] Observed Wind Chill less than 0’F. Lightning Warning. [ ] Observed winds in excess of 35 miles per hour. [ ] Significant Weather Advisory (no FSU ALERT). -

Heat Waves in Southern California: Are They Becoming More Frequent and Longer Lasting?
Heat Waves in Southern California: Are They Becoming More Frequent and Longer Lasting? A!"# T$%!$&#$' University of California, Berkeley S()*) L$D+,-. California State University, Los Angeles J+/- W#00#/ $'1 W#00#$% C. P$(&)!( Jet Propulsion Laboratory, NASA ABSTRACT Los Angeles is experiencing more heat waves and also more extreme heat days. 2ese numbers have increased by over 3 heat waves per century and nearly 23 days per century occurrences, respectively. Both have more than tripled over the past 100 years as a consequence of the steady warming of Los Angeles. Our research explores the daily maximum and minimum temper- atures from 1906 to 2006 recorded by the Department of Water and Power (DWP) downtown station and Pierce College, a suburban valley location. 2e average annual maximum temperature in Los Angeles has warmed by 5.0°F (2.8°C), while the average annual minimum temperature has warmed by 4.2°F (2.3°C). 2e greatest rate of change was during the summer months for both maximum and minimum temperature, with late fall and early winter having the least rates of change. 2ere was also an increase in heat wave duration. Heat waves lasting longer than six days occurred regularly a3er the 1970s but were nonexistent from the start of 1906 until 1956, when the 4rst six-day heat wave was recorded. While heat days have increased dramatically in the past century, cold days, where minimum temperature is below 45°F (7.2°C), show a slight decreasing trend. Recent deadly heat waves in the western United States have generated increasing electricity demands. -
National Weather Service Reference Guide
National Weather Service Reference Guide Purpose of this Document he National Weather Service (NWS) provides many products and services which can be T used by other governmental agencies, Tribal Nations, the private sector, the public and the global community. The data and services provided by the NWS are designed to fulfill us- ers’ needs and provide valuable information in the areas of weather, hydrology and climate. In addition, the NWS has numerous partnerships with private and other government entities. These partnerships help facilitate the mission of the NWS, which is to protect life and prop- erty and enhance the national economy. This document is intended to serve as a reference guide and information manual of the products and services provided by the NWS on a na- tional basis. Editor’s note: Throughout this document, the term ―county‖ will be used to represent counties, parishes, and boroughs. Similarly, ―county warning area‖ will be used to represent the area of responsibility of all of- fices. The local forecast office at Buffalo, New York, January, 1899. The local National Weather Service Office in Tallahassee, FL, present day. 2 Table of Contents Click on description to go directly to the page. 1. What is the National Weather Service?…………………….………………………. 5 Mission Statement 6 Organizational Structure 7 County Warning Areas 8 Weather Forecast Office Staff 10 River Forecast Center Staff 13 NWS Directive System 14 2. Non-Routine Products and Services (watch/warning/advisory descriptions)..…….. 15 Convective Weather 16 Tropical Weather 17 Winter Weather 18 Hydrology 19 Coastal Flood 20 Marine Weather 21 Non-Precipitation 23 Fire Weather 24 Other 25 Statements 25 Other Non-Routine Products 26 Extreme Weather Wording 27 Verification and Performance Goals 28 Impact-Based Decision Support Services 30 Requesting a Spot Fire Weather Forecast 33 Hazardous Materials Emergency Support 34 Interactive Warning Team 37 HazCollect 38 Damage Surveys 40 Storm Data 44 Information Requests 46 3.