Methylamphetamine Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Stimulants and Hallucinogens Under Consideration: a Brief Overview of Their Chemistry and Pharmacology
Drug and Alcohol Dependence, 17 (1986) 107-118 107 Elsevier Scientific Publishers Ireland Ltd. THE STIMULANTS AND HALLUCINOGENS UNDER CONSIDERATION: A BRIEF OVERVIEW OF THEIR CHEMISTRY AND PHARMACOLOGY LOUIS S. HARRIS Dcparlmcnl of Pharmacology, Medical College of Virginia, Virginia Commonwealth Unwersity, Richmond, VA 23298 (U.S.A.) SUMMARY The substances under review are a heterogenous set of compounds from a pharmacological point of view, though many have a common phenylethyl- amine structure. Variations in structure lead to marked changes in potency and characteristic action. The introductory material presented here is meant to provide a set of chemical and pharmacological highlights of the 28 substances under con- sideration. The most commonly used names or INN names, Chemical Abstract (CA) names and numbers, and elemental formulae are provided in the accompanying figures. This provides both some basic information on the substances and a starting point for the more detailed information that follows in the individual papers by contributors to the symposium. Key words: Stimulants, their chemistry and pharmacology - Hallucinogens, their chemistry and pharmacology INTRODUCTION Cathine (Fig. 1) is one of the active principles of khat (Catha edulis). The structure has two asymmetric centers and exists as two geometric isomers, each of which has been resolved into its optical isomers. In the plant it exists as d-nor-pseudoephedrine. It is a typical sympathomimetic amine with a strong component of amphetamine-like activity. The racemic mixture is known generically in this country and others as phenylpropanolamine (dl- norephedrine). It is widely available as an over-the-counter (OTC) anti- appetite agent and nasal decongestant. -

(19) United States (12) Patent Application Publication (10) Pub
US 20130289061A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2013/0289061 A1 Bhide et al. (43) Pub. Date: Oct. 31, 2013 (54) METHODS AND COMPOSITIONS TO Publication Classi?cation PREVENT ADDICTION (51) Int. Cl. (71) Applicant: The General Hospital Corporation, A61K 31/485 (2006-01) Boston’ MA (Us) A61K 31/4458 (2006.01) (52) U.S. Cl. (72) Inventors: Pradeep G. Bhide; Peabody, MA (US); CPC """"" " A61K31/485 (201301); ‘4161223011? Jmm‘“ Zhu’ Ansm’ MA. (Us); USPC ......... .. 514/282; 514/317; 514/654; 514/618; Thomas J. Spencer; Carhsle; MA (US); 514/279 Joseph Biederman; Brookline; MA (Us) (57) ABSTRACT Disclosed herein is a method of reducing or preventing the development of aversion to a CNS stimulant in a subject (21) App1_ NO_; 13/924,815 comprising; administering a therapeutic amount of the neu rological stimulant and administering an antagonist of the kappa opioid receptor; to thereby reduce or prevent the devel - . opment of aversion to the CNS stimulant in the subject. Also (22) Flled' Jun‘ 24’ 2013 disclosed is a method of reducing or preventing the develop ment of addiction to a CNS stimulant in a subj ect; comprising; _ _ administering the CNS stimulant and administering a mu Related U‘s‘ Apphcatlon Data opioid receptor antagonist to thereby reduce or prevent the (63) Continuation of application NO 13/389,959, ?led on development of addiction to the CNS stimulant in the subject. Apt 27’ 2012’ ?led as application NO_ PCT/US2010/ Also disclosed are pharmaceutical compositions comprising 045486 on Aug' 13 2010' a central nervous system stimulant and an opioid receptor ’ antagonist. -

Gavinmclaughlin.Pdf (2.172Mb)
Accepted for publication in Drug Testing and Analysis 13.04.2018 Synthesis, analytical characterization and monoamine transporter activity of the new psychoactive substance 4- methylphenmetrazine (4-MPM), with differentiation from its ortho- and meta- positional isomers Gavin McLaughlin, a,b* Michael H. Baumann, c Pierce V. Kavanagh, a Noreen Morris, d John D. Power, a,b Geraldine Dowling, a,e Brendan Twamley, f John O’Brien, f Gary Hessman, f Folker Westphal, g Donna Walther, c and Simon D. Brandt h a Department of Pharmacology and Therapeutics, School of Medicine, Trinity Centre for Health Sciences, St. James’s Hospital, James’s Street, Dublin 8, D08W9RT, Ireland b Forensic Science Ireland, Garda Headquarters, Phoenix Park, Dublin 8, D08HN3X, Ireland c Designer Drug Research Unit, Intramural Research Program, National Institute on Drug Abuse, National Institutes of Health, 333 Cassell Drive, Suite 4400, Baltimore, MD 21224, USA d Department of Life & Physical Sciences, Faculty of Science and Health, Athlone Institute of Technology, Dublin Road, Athlone, Co. Westmeath, N37HD68, Ireland e Department of Life Sciences, School of Science, Sligo Institute of Technology, Ash Lane, Sligo, F91YW50, Ireland f School of Chemistry, Trinity College Dublin, College Green, Dublin 2, D02EV57, Ireland g State Bureau of Criminal Investigation Schleswig-Holstein, Section Narcotics/Toxicology, Mühlenweg 166, D-24116 Kiel, Germany h School of Pharmacy and Biomolecular Sciences, Liverpool John Moores University, Byrom Street, Liverpool L3 3AF, UK *Correspondence to: Gavin McLaughlin, Department of Pharmacology & Therapeutics, School of Medicine, Trinity Centre for Health Sciences, St. James’s Hospital, James’s Street, Dublin 8, D08W9RT, Ireland. E-Mail: [email protected] Running title: Characterization of methylphenmetrazine isomers 1 Accepted for publication in Drug Testing and Analysis 13.04.2018 Abstract The availability of new psychoactive substances on the recreational drug market continues to create challenges for scientists in the forensic, clinical and toxicology fields. -

An Update on Pharmacological Therapy for ADHD Derek Ott, M.D., M.S
An Update on Pharmacological Therapy for ADHD Derek Ott, M.D., M.S. Assistant Clinical Professor UCLA David Geffen School of Medicine Division of Child & Adolescent Psychiatry Director, Pediatric Neuropsychiatry Clinic Epidemiology Most commonly diagnosed behavioral disorder of childhood 1 in 20 children are affected worldwide Roughly 3 – 7% of school children are affected Males>Females between 2:1 up to 9:1 Girls often show less hyperactivity, fewer conduct disorder, decreased rates of externalizing behaviors; inattentive subtype may be more common Hyperactive/Impulsive subtype more commonly diagnosed in young children Worldwide Prevalence: 3% to 7% Studies of ADHD prevalence United States (Shaffer et al 1996) Tennessee (Wolraich et al 1996) Mannheim, Germany (Esser et al 1990) London, England (Esser et al 1990) Germany (Baumgaertel et al 1995) Iowa (Lindgren et al 1990) Pittsburgh, PA (Costello et al 1988) US inner city (Newcorn et al 1989) Ontario (Szatmari et al 1989) New Zealand (Anderson et al 1997) 0 5 10 15 20 Prevalence of ADHD (%) in school-age children Goldman, et al. JAMA.1998;279:1100-1107. Eology Dopamine + norepinephrine implicated historically No specific tests to determine levels Imaging studies support frontal lobe dysfunction in ADHD + (sub)cortical circuit involvement Neither of which are valid for diagnostic purposes Specific gene associations have been suggested • Thyroid receptor gene (chr #3) • DA/T1 transporter gene (chr #5) • DA/D4 receptor gene (chr #11) Eology • Neurological Factors: ? • Imaging studies -
On Speed: the Many Lives of Amphetamine
On Speed Nicolas Rasmussen On Speed The Many Lives of Amphetamine a New York University Press • New York and London NEW YORK UNIVERSITY PRESS New York and London www.nyupress.org © 2008 by New York University All rights reserved Library of Congress Cataloging-in-Publication Data Rasmussen, Nicolas, 1962– On speed : the many lives of amphetamine / Nicolas Rasmussen. p. ; cm. Includes bibliographical references and index. ISBN-13: 978-0-8147-7601-8 (cl : alk. paper) ISBN-10: 0-8147-7601-9 (cl : alk. paper) 1. Amphetamines—United States—History. 2. Amphetamine abuse— United States—History. I. Title. II. Title: Many lives of amphetamine. [DNLM: 1. Amphetamines—history—United States. 2. Amphetamine-Related Disorders—history—United States. 3. History, 20th Century—United States. 4. History, 21st Century—United States. QV 102 R225o 2007] RM666.A493R37 2007 362.29'90973—dc22 2007043261 New York University Press books are printed on acid-free paper, and their binding materials are chosen for strength and durability. Manufactured in the United States of America c10987654321 p10987654321 To my parents, Laura and Norman, for teaching me to ask questions Contents Acknowledgments ix Introduction 1 1 The New Sensation 6 2 Benzedrine: The Making of a Modern Medicine 25 3 Speed and Total War 53 4 Bootleggers, Beatniks, and Benzedrine Benders 87 5 A Bromide for the Atomic Age 113 6 Amphetamine and the Go-Go Years 149 7 Amphetamine’s Decline: From Mental Medicine to Social Disease 182 8 Fast Forward: Still on Speed, 1971 to Today 222 Conclusion: The Lessons of History 255 Notes 261 List of Archival Sources 347 Index 348 About the Author 352 Illustrations appear in two groups following pages 86 and 148. -

Phenylmorpholines and Analogues Thereof Phenylmorpholine Und Analoge Davon Phenylmorpholines Et Analogues De Celles-Ci
(19) TZZ __T (11) EP 2 571 858 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: C07D 265/30 (2006.01) A61K 31/5375 (2006.01) 20.06.2018 Bulletin 2018/25 A61P 25/24 (2006.01) A61P 25/16 (2006.01) A61P 25/18 (2006.01) (21) Application number: 11723158.9 (86) International application number: (22) Date of filing: 20.05.2011 PCT/US2011/037361 (87) International publication number: WO 2011/146850 (24.11.2011 Gazette 2011/47) (54) PHENYLMORPHOLINES AND ANALOGUES THEREOF PHENYLMORPHOLINE UND ANALOGE DAVON PHENYLMORPHOLINES ET ANALOGUES DE CELLES-CI (84) Designated Contracting States: • DECKER, Ann Marie AL AT BE BG CH CY CZ DE DK EE ES FI FR GB Durham, North Carolina 27713 (US) GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO PL PT RO RS SE SI SK SM TR (74) Representative: Hoeger, Stellrecht & Partner Patentanwälte mbB (30) Priority: 21.05.2010 US 347259 P Uhlandstrasse 14c 70182 Stuttgart (DE) (43) Date of publication of application: 27.03.2013 Bulletin 2013/13 (56) References cited: WO-A1-2004/052372 WO-A1-2008/026046 (73) Proprietors: WO-A1-2008/087512 DE-B- 1 135 464 • Research Triangle Institute FR-A- 1 397 563 GB-A- 883 220 Research Triangle Park, North Carolina 27709 GB-A- 899 386 US-A1- 2005 267 096 (US) • United States of America, as represented by • R.A. GLENNON ET AL.: "Beta-Oxygenated The Secretary, Department of Health and Human Analogues of the 5-HT2A Serotonin Receptor Services Agonist Bethesda, Maryland 20892-7660 (US) 1-(4-Bromo-2,5-dimethoxyphenyl)-2-aminopro pane", JOURNAL OF MEDICINAL CHEMISTRY, (72) Inventors: vol. -

Whoexpertcommittee Ondrugdependence
Thisreportcontainsthecollectiveviewsof an international groupof expertsanddoesnotnecessarilyrepresentthedecisions Tile World 1lealth Organization is a specialized agcncyof the United Nations with orthestatedpolicyof theWorldHealthOrganization primary responsibility for international health'matters anti public health. Through this organization, which was created in 1948, the health professions of' some I65 countries exchange their knowledge and experience with the aim of making possible will permit them lo lead a socially and ccommlically productive lil_. WHOExpertCommittee By means of direct technical cooperation whh its Membcr Stales, and by stimt,- hhensiveding suchhealthcooperationservices, tamonghe preventionthem, WllOprornotesthcdevclopmcntorcomprc-anti control of diseascs, thc improvement o[ environmental conditions, tile development of health manpower, the coordination onDrugDependence anti development of biomedical and health services research, and thc planning and implementation of health programmes. These broad fiekls of endeavour encompass a wide variety of activities, such as developing systems of primary health cltre that reach the whole population of Mem- ber countries; promoting tile health of`mothers and children; combating malnutrition; controlling malaria and other communicable diseases including tuberculosis and leprosy; having achieved tile eradication or smallpox, promoting mass immunization against a numbcr of other preventable diseases; improving mental health; providing safe water supplies: anti training health -

Doping Control of Athletes
trends in analytical chemistry, vol. 7, no. IO, I988 375 trends Doping control of athletes E. G. de Jong*, I?. A. A. Maes and The definition of the Council of Europe for doping J. M. van Rossum is2: Utrecht, Netherlands ‘The administration to or the use by a healthy indi- vidual in any way of compounds which are not natu- History ral to the organism or the use of physiological com- The origin of the word doping is not certain. It first pounds in abnormal doses or in an abnormal way appeared in the English dictionaries at the end of the with the only purpose to artificially and dishonestly nineteenth century. The first reference to the use of influence the performance of this person during doping by athletes was in 1864 during swimming competition.’ competitions that were held in the canals of Amster- Another possible definition is: dam. The use of what is known as a ‘speedball’, a ‘The use of compounds which are not synthesized mixture of heroine and cocaine, by cyclists was de- by the human body or the use of endogenous com- scribed in 1869. In 1904 the Russian chemist pounds in excessive doses with the aim to improve Bukowski was able to identify some alkaloids in the performance in sport competitions.’ saliva of horses’. A simpler definition is: Australia was the first country to take measures ‘The use of forbidden drugs. ’ against doping in sports in 1962, and England fol- The last definition can only be used when we have lowed with the drugs bill in 1964. -
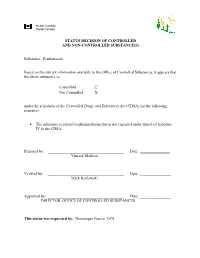
Substance: Fenbutrazate Based on the Current
Health Canada Santé Canada STATUS DECISION OF CONTROLLED AND NON-CONTROLLED SUBSTANCE(S) Substance: Fenbutrazate Based on the current information available to the Office of Controlled Substances, it appears that the above substance is: Controlled ☐ Not Controlled X under the schedules of the Controlled Drugs and Substances Act (CDSA) for the following reason(s): The substance is related to phenmetrazine but is not captured under item 6 of Schedule IV to the CDSA. Prepared by: _______________________________________ Date: _______________ Vincent Marleau Verified by: _______________________________________ Date: ________________ Mark Kozlowski Approved by: _______________________________________ Date: ________________ DIRECTOR, OFFICE OF CONTROLLED SUBSTANCES This status was requested by: Dominique Franco, OCS 2 Drug Status Report Drug: Fenbutrazate Drug Name Status: Fenbutrazate is the common name. Chemical Name: 2-(3-Methyl-2-phenylmorpholino)ethyl 2-phenylbutanoate Other Names: Phenbutrazate; 2-Phenylbutyric Acid 2-(3-Methyl-2-phenylmorpholino)ethyl Ester; Fenbutrazatum; Nethanol; Phenbutrazatum; α-Ethylbenzeneacetic Acid 2-(3-Methyl-2- phenyl-4-morpholinyl)ethyl Ester. Chemical structure: Fenbutrazate Phenmetrazine Molecular Formula: C23H29NO3 CAS-RN: 4378-36-3 Pharmacological class / Application: Phenmetrazine derivative International status: US: Fenbutrazate is not listed specifically in the Schedules to the US Controlled Substances Act and is not mentioned anywhere on the DEA website. United Nations: The substance is not listed on the Yellow List - List of Narcotic Drugs under International Control, the Green List - List of Psychotropic Substances under International Control, nor the Red List - List of Precursors and Chemicals Frequently Used in the Illicit Manufacture of Narcotic Drugs and Psychotropic Substances under International Control. Canadian Status: Fenbutrazate is not listed in the Schedules to the CDSA. -
Introduced B.,Byhansen, 16
LB301 LB301 2021 2021 LEGISLATURE OF NEBRASKA ONE HUNDRED SEVENTH LEGISLATURE FIRST SESSION LEGISLATIVE BILL 301 Introduced by Hansen, B., 16. Read first time January 12, 2021 Committee: Judiciary 1 A BILL FOR AN ACT relating to the Uniform Controlled Substances Act; to 2 amend sections 28-401, 28-405, and 28-416, Revised Statutes 3 Cumulative Supplement, 2020; to redefine terms; to change drug 4 schedules and adopt federal drug provisions; to change a penalty 5 provision; and to repeal the original sections. 6 Be it enacted by the people of the State of Nebraska, -1- LB301 LB301 2021 2021 1 Section 1. Section 28-401, Revised Statutes Cumulative Supplement, 2 2020, is amended to read: 3 28-401 As used in the Uniform Controlled Substances Act, unless the 4 context otherwise requires: 5 (1) Administer means to directly apply a controlled substance by 6 injection, inhalation, ingestion, or any other means to the body of a 7 patient or research subject; 8 (2) Agent means an authorized person who acts on behalf of or at the 9 direction of another person but does not include a common or contract 10 carrier, public warehouse keeper, or employee of a carrier or warehouse 11 keeper; 12 (3) Administration means the Drug Enforcement Administration of the 13 United States Department of Justice; 14 (4) Controlled substance means a drug, biological, substance, or 15 immediate precursor in Schedules I through V of section 28-405. 16 Controlled substance does not include distilled spirits, wine, malt 17 beverages, tobacco, hemp, or any nonnarcotic substance if such substance 18 may, under the Federal Food, Drug, and Cosmetic Act, 21 U.S.C. -

4-Fluoroamphetamine (4-FA) Critical Review Report Agenda Item 4.3
4-Fluoroamphetamine (4-FA) Critical Review Report Agenda Item 4.3 Expert Committee on Drug Dependence Thirty-ninth Meeting Geneva, 6-10 November 2017 39th ECDD (2017) Agenda item 4.3 4-FA Contents Acknowledgements.................................................................................................................................. 4 Summary...................................................................................................................................................... 5 1. Substance identification ....................................................................................................................... 6 A. International Nonproprietary Name (INN).......................................................................................................... 6 B. Chemical Abstract Service (CAS) Registry Number .......................................................................................... 6 C. Other Chemical Names ................................................................................................................................................... 6 D. Trade Names ....................................................................................................................................................................... 6 E. Street Names ....................................................................................................................................................................... 6 F. Physical Appearance ...................................................................................................................................................... -

Marrakesh Agreement Establishing the World Trade Organization
No. 31874 Multilateral Marrakesh Agreement establishing the World Trade Organ ization (with final act, annexes and protocol). Concluded at Marrakesh on 15 April 1994 Authentic texts: English, French and Spanish. Registered by the Director-General of the World Trade Organization, acting on behalf of the Parties, on 1 June 1995. Multilat ral Accord de Marrakech instituant l©Organisation mondiale du commerce (avec acte final, annexes et protocole). Conclu Marrakech le 15 avril 1994 Textes authentiques : anglais, français et espagnol. Enregistré par le Directeur général de l'Organisation mondiale du com merce, agissant au nom des Parties, le 1er juin 1995. Vol. 1867, 1-31874 4_________United Nations — Treaty Series • Nations Unies — Recueil des Traités 1995 Table of contents Table des matières Indice [Volume 1867] FINAL ACT EMBODYING THE RESULTS OF THE URUGUAY ROUND OF MULTILATERAL TRADE NEGOTIATIONS ACTE FINAL REPRENANT LES RESULTATS DES NEGOCIATIONS COMMERCIALES MULTILATERALES DU CYCLE D©URUGUAY ACTA FINAL EN QUE SE INCORPOR N LOS RESULTADOS DE LA RONDA URUGUAY DE NEGOCIACIONES COMERCIALES MULTILATERALES SIGNATURES - SIGNATURES - FIRMAS MINISTERIAL DECISIONS, DECLARATIONS AND UNDERSTANDING DECISIONS, DECLARATIONS ET MEMORANDUM D©ACCORD MINISTERIELS DECISIONES, DECLARACIONES Y ENTEND MIENTO MINISTERIALES MARRAKESH AGREEMENT ESTABLISHING THE WORLD TRADE ORGANIZATION ACCORD DE MARRAKECH INSTITUANT L©ORGANISATION MONDIALE DU COMMERCE ACUERDO DE MARRAKECH POR EL QUE SE ESTABLECE LA ORGANIZACI N MUND1AL DEL COMERCIO ANNEX 1 ANNEXE 1 ANEXO 1 ANNEX