Supplemental Table: International Classification of Diseases, ICD-9 Codes for Gastrointestinal Morbidities Accounted For
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Diagnosis and Treatment of Perianal Crohn Disease: NASPGHAN Clinical Report and Consensus Statement
CLINICAL REPORT Diagnosis and Treatment of Perianal Crohn Disease: NASPGHAN Clinical Report and Consensus Statement ÃEdwin F. de Zoeten, zBrad A. Pasternak, §Peter Mattei, ÃRobert E. Kramer, and yHoward A. Kader ABSTRACT disease. The first description connecting regional enteritis with Inflammatory bowel disease is a chronic inflammatory disorder of the perianal disease was by Bissell et al in 1934 (2), and since that time gastrointestinal tract that includes both Crohn disease (CD) and ulcerative perianal disease has become a recognized entity and an important colitis. Abdominal pain, rectal bleeding, diarrhea, and weight loss consideration in the diagnosis and treatment of CD. Perianal characterize both CD and ulcerative colitis. The incidence of IBD in the Crohn disease (PCD) is defined as inflammation at or near the United States is 70 to 150 cases per 100,000 individuals and, as with other anus, including tags, fissures, fistulae, abscesses, or stenosis. autoimmune diseases, is on the rise. CD can affect any part of the The symptoms of PCD include pain, itching, bleeding, purulent gastrointestinal tract from the mouth to the anus and frequently will include discharge, and incontinence of stool. perianal disease. The first description connecting regional enteritis with perianal disease was by Bissell et al in 1934, and since that time perianal INCIDENCE AND NATURAL HISTORY disease has become a recognized entity and an important consideration in the Limited pediatric data describe the incidence and prevalence diagnosis and treatment of CD. Perianal Crohn disease (PCD) is defined as of PCD. The incidence of PCD in the pediatric age group has been inflammation at or near the anus, including tags, fissures, fistulae, abscesses, estimated to be between 13.6% and 62% (3). -

Recent Advances in Surgery the Blind-Loop Syndrome After Gastric
Recent advances in surgery Conducted by ALFRED BLALOCK, M.D. The blind-loop syndrome after gastric operations ince the earliest reports by Whitees time, several examples of the blind-loop ANATOMIC CONFIGURATION OF BLIND LOOPS Various examples of gastrointestinal blind and Wangensteen;O a side-arm loop has been employed as in Fig. 1, A, in which the loop is arranged so as to be self-filling. The side loop arrangement is the one which most 849 850 Recent advances in surgery Surgery ;.$ Nouernbcr 1961 & ad cumulated from observations on lesions at differing sites in the gastrointestinal tract. The principles involved apply, with varia- tions, to blind loops at all levels. The best- known feature of the blind-loop syndrome is megaloblastic anemia, which is due to dis- ruption of vitamin BI2 absorption. Normally, dietary vitamin B12 (Castle's extrinsic fac- tor) is absorbed after an incompletely under- stood interaction with intrinsic factor (Fig. 3, A), a mucoprotein secreted by the gastric rnu~osa.*~In man, the principal site of B,, absorption is the ileum.7* Vitamin B,, deficiency can develop by a number of alternative mechanisms. Rarely loops which have caGsed the blind-loop- syndrome.- is there dietary deficiency of this nutritional A, Anastomosis with formation of a self-filled stagnant loop, B, with jejunal diverticulosis, C, factor. Commonly, as in pernicious anemia with intestinal strictures, D, after enteroenteros- (Fig. 3, B) or after total gastrectomy,Sgthere tomies or fistulas, and E, after gastric operation. is absent intrinsic factor due to gastric atrophy or the absence. of the stomach, re- resembles a blind loop which develops after spectively. -

Plugs for Anal Fistula Repair Original Policy Date: November 26, 2014 Effective Date: January 1, 2021 Section: 7.0 Surgery Page: Page 1 of 12
Medical Policy 7.01.123 Plugs for Anal Fistula Repair Original Policy Date: November 26, 2014 Effective Date: January 1, 2021 Section: 7.0 Surgery Page: Page 1 of 12 Policy Statement Biosynthetic fistula plugs, including plugs made of porcine small intestine submucosa or of synthetic material, are considered investigational for the repair of anal fistulas. NOTE: Refer to Appendix A to see the policy statement changes (if any) from the previous version. Policy Guidelines There is a specific CPT code for the use of these plugs in the repair of an anorectal fistula: • 46707: Repair of anorectal fistula with plug (e.g., porcine small intestine submucosa [SIS]) Description Anal fistula plugs (AFPs) are biosynthetic devices used to promote healing and prevent the recurrence of anal fistulas. They are proposed as an alternative to procedures including fistulotomy, endorectal advancement flaps, seton drain placement, and use of fibrin glue in the treatment of anal fistulas. Related Policies • N/A Benefit Application Benefit determinations should be based in all cases on the applicable contract language. To the extent there are any conflicts between these guidelines and the contract language, the contract language will control. Please refer to the member's contract benefits in effect at the time of service to determine coverage or non-coverage of these services as it applies to an individual member. Some state or federal mandates (e.g., Federal Employee Program [FEP]) prohibits plans from denying Food and Drug Administration (FDA)-approved technologies as investigational. In these instances, plans may have to consider the coverage eligibility of FDA-approved technologies on the basis of medical necessity alone. -

Surgery for Colon and Rectal Cancer
Colon and Rectal Surgery Mohammed Bayasi, MD Department of Surgery Colon and Rectal Surgery What is a Colon and Rectal Surgeon? • Fully trained General Surgeon. • Has done additional training in the diseases of colon and rectum. Why Colon and Rectal Surgery? • Surgical and non surgical therapy for multiple diseases. • Chance to help cancer patients by removing tumor, potentially curing them. • Variety of cases, ages and patient populations. • Specialized area. Colorectal Diseases • Colon • Rectum/Anus – Cancer – Hemorrhoids – Diverticulitis – Anal fistula and – Inflammatory Bowel abscess Disease (Crohn, UC) – Anal fissure – Polyps – Prolapse Symptoms/Signs • Pain • Itching • Discharge • Bleeding • Lump Anatomy Lesson Colon • Extracts water and nutrients. • Helps to form and excrete waste. • Stores important bacteria flora. • Length: 1.5 meters long = 4.9 feet = 59 inches Colon Rectum/Anus • The final portion of the colon. • Area contains muscles important in controlling defecation and flatulence. Rectum/Anus When to see a Colon and Rectal Surgeon • Referral from another physician (Gastroenterology, PCP). • Treatment of anorectal diseases. • Blood with stool, abdominal pain, rectal pain. Hemorrhoids • Internal and external. • Cushions of blood vessels. • When enlarged, they cause bleeding and pain. Treatment • Treatment of symptomatic hemorrhoids is directed by the symptoms themselves. It can broadly be categorized into four groups: − Medical therapy − Office-based procedure − Operative therapies − Emergent interventions Anorectal Abscess • It is a collection of pus in the perianal area. Normal • Causes pain and rectal gland drainage, and if it progresses, fever and systemic Abscess infection. • Treated with incision and drainage. Anorectal Fistula • A tunnel between the inside of the anus and the skin. • Causes discharge, pain, and formation of abscess. -

Common Anorectal Conditions
TurkJMedSci 34(2004)285-293 ©TÜB‹TAK PERSPECTIVESINMEDICALSCIENCES CommonAnorectalConditions PravinJ.GUPTA ConsultingProctologistGuptaNursingHome,D/9,Laxminagar,NAGPUR-440022INDIA Received:July12,2004 Anorectaldisordersincludeadiversegroupof dentateorpectinatelinedividesthesquamousepithelium pathologicdisordersthatgeneratesignificantpatient fromthemucosalorcolumnarepithelium.Fourtoeight discomfortanddisability.Althoughthesearefrequently analglandsdrainintothecryptsofMorgagniatthelevel encounteredingeneralmedicalpractice,theyoften ofthedentateline.Mostrectalabscessesandfistulae receiveonlycasualattentionandtemporaryrelief . originateintheseglands.Thedentatelinealsodelineates Diseasesoftherectumandanusarecommon theareawheresensoryfibersend.Abovethedentate phenomena.Theirprevalenceinthegeneralpopulationis line,therectumissuppliedbystretchnervefibers,and probablymuchhigherthanthatseeninclinicalpractice, notpainnervefibers.Thisallowsmanysurgical sincemostpatientswithsymptomsreferabletothe procedurestobeperformedwithoutanesthesiaabovethe anorectumdonotseekmedicalattention. dentateline.Conversely,belowthedentateline,thereis extremesensitivity,andtheperianalareaisoneofthe Asdoctorsoffirstcontact,general(family) mostsensitiveareasofthebody.Theevacuationofbowel practitioners(GPs)frequentlyfacedifficultquestions contentsdependsonactionbythemusclesofboththe concerningtheoptimummanagementofanorectal involuntaryinternalsphincterandthevoluntaryexternal symptoms.Whiletheexaminationanddiagnosisof sphincter. certainanorectaldisorderscanbechallenging,itisa -

ICD-9 Diagnosis Codes Effective 10/1/2011 (V29.0) Source: Centers for Medicare and Medicaid Services
ICD-9 Diagnosis Codes effective 10/1/2011 (v29.0) Source: Centers for Medicare and Medicaid Services 0010 Cholera d/t vib cholerae 00801 Int inf e coli entrpath 01086 Prim prg TB NEC-oth test 0011 Cholera d/t vib el tor 00802 Int inf e coli entrtoxgn 01090 Primary TB NOS-unspec 0019 Cholera NOS 00803 Int inf e coli entrnvsv 01091 Primary TB NOS-no exam 0020 Typhoid fever 00804 Int inf e coli entrhmrg 01092 Primary TB NOS-exam unkn 0021 Paratyphoid fever a 00809 Int inf e coli spcf NEC 01093 Primary TB NOS-micro dx 0022 Paratyphoid fever b 0081 Arizona enteritis 01094 Primary TB NOS-cult dx 0023 Paratyphoid fever c 0082 Aerobacter enteritis 01095 Primary TB NOS-histo dx 0029 Paratyphoid fever NOS 0083 Proteus enteritis 01096 Primary TB NOS-oth test 0030 Salmonella enteritis 00841 Staphylococc enteritis 01100 TB lung infiltr-unspec 0031 Salmonella septicemia 00842 Pseudomonas enteritis 01101 TB lung infiltr-no exam 00320 Local salmonella inf NOS 00843 Int infec campylobacter 01102 TB lung infiltr-exm unkn 00321 Salmonella meningitis 00844 Int inf yrsnia entrcltca 01103 TB lung infiltr-micro dx 00322 Salmonella pneumonia 00845 Int inf clstrdium dfcile 01104 TB lung infiltr-cult dx 00323 Salmonella arthritis 00846 Intes infec oth anerobes 01105 TB lung infiltr-histo dx 00324 Salmonella osteomyelitis 00847 Int inf oth grm neg bctr 01106 TB lung infiltr-oth test 00329 Local salmonella inf NEC 00849 Bacterial enteritis NEC 01110 TB lung nodular-unspec 0038 Salmonella infection NEC 0085 Bacterial enteritis NOS 01111 TB lung nodular-no exam 0039 -

Crohn's Disease of the Anal Region
Gut: first published as 10.1136/gut.6.6.515 on 1 December 1965. Downloaded from Gut, 1965, 6, 515 Crohn's disease of the anal region B. K. GRAY, H. E. LOCKHART-MUMMERY, AND B. C. MORSON From the Research Department, St. Mark's Hospital, London EDITORIAL SYNOPSIS This paper records for the first time the clinico-pathological picture of Crohn's disease affecting the anal canal. It has long been recognized that anal lesions may precede intestinal Crohn's disease, often by some years, but the specific characteristics of the lesion have not hitherto been described. The differential diagnosis is discussed in detail. In a previous report from this hospital (Morson and types of anal lesion when the patients were first seen Lockhart-Mummery, 1959) the clinical features and were as follows: pathology of the anal lesions of Crohn's disease were described. In that paper reference was made to Anal fistula, single or multiple .............. 13 several patients with anal fissures or fistulae, biopsy Anal fissures ........... ......... 3 of which showed a sarcoid reaction, but in whom Anal fissure and fistula .................... 3 there was no clinical or radiological evidence of Total 19 intra-abdominal Crohn's disease. The opinion was expressed that some of these patients might later The types of fistula included both low level and prove to have intestinal pathology. This present complex high level varieties. The majority had the contribution is a follow-up of these cases as well as clinical features described previously (Morson and of others seen subsequently. Lockhart-Mummery, 1959; Lockhart-Mummery Involvement of the anus in Crohn's disease has and Morson, 1964) which suggest Crohn's disease, http://gut.bmj.com/ been seen at this hospital in three different ways: that is, the lesions had an indolent appearance with 1 Patients who presented with symptoms of irregular undermined edges and absence of indura- intestinal Crohn's disease who, at the same time, ation. -

Clinical Practice Guideline for the Management of Anorectal Abscess, Fistula-In-Ano, and Rectovaginal Fistula Jon D
PRACTICE GUIDELINES Clinical Practice Guideline for the Management of Anorectal Abscess, Fistula-in-Ano, and Rectovaginal Fistula Jon D. Vogel, M.D. • Eric K. Johnson, M.D. • Arden M. Morris, M.D. • Ian M. Paquette, M.D. Theodore J. Saclarides, M.D. • Daniel L. Feingold, M.D. • Scott R. Steele, M.D. Prepared on behalf of The Clinical Practice Guidelines Committee of the American Society of Colon and Rectal Surgeons he American Society of Colon and Rectal Sur- and submucosal locations.7–11 Anorectal abscess occurs geons is dedicated to ensuring high-quality pa- more often in males than females, and may occur at any Ttient care by advancing the science, prevention, age, with peak incidence among 20 to 40 year olds.4,8–12 and management of disorders and diseases of the co- In general, the abscess is treated with prompt incision lon, rectum, and anus. The Clinical Practice Guide- and drainage.4,6,10,13 lines Committee is charged with leading international Fistula-in-ano is a tract that connects the perine- efforts in defining quality care for conditions related al skin to the anal canal. In patients with an anorec- to the colon, rectum, and anus by developing clinical tal abscess, 30% to 70% present with a concomitant practice guidelines based on the best available evidence. fistula-in-ano, and, in those who do not, one-third will These guidelines are inclusive, not prescriptive, and are be diagnosed with a fistula in the months to years after intended for the use of all practitioners, health care abscess drainage.2,5,8–10,13–16 Although a perianal abscess workers, and patients who desire information about the is defined by the anatomic space in which it forms, a management of the conditions addressed by the topics fistula-in-ano is classified in terms of its relationship to covered in these guidelines. -
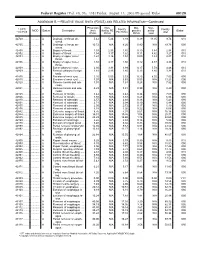
RELATIVE VALUE UNITS (RVUS) and RELATED INFORMATION—Continued
Federal Register / Vol. 68, No. 158 / Friday, August 15, 2003 / Proposed Rules 49129 ADDENDUM B.—RELATIVE VALUE UNITS (RVUS) AND RELATED INFORMATION—Continued Physician Non- Mal- Non- 1 CPT/ Facility Facility 2 MOD Status Description work facility PE practice acility Global HCPCS RVUs RVUs PE RVUs RVUs total total 42720 ....... ........... A Drainage of throat ab- 5.42 5.24 3.93 0.39 11.05 9.74 010 scess. 42725 ....... ........... A Drainage of throat ab- 10.72 N/A 8.26 0.80 N/A 19.78 090 scess. 42800 ....... ........... A Biopsy of throat ................ 1.39 2.35 1.45 0.10 3.84 2.94 010 42802 ....... ........... A Biopsy of throat ................ 1.54 3.17 1.62 0.11 4.82 3.27 010 42804 ....... ........... A Biopsy of upper nose/ 1.24 3.16 1.54 0.09 4.49 2.87 010 throat. 42806 ....... ........... A Biopsy of upper nose/ 1.58 3.17 1.66 0.12 4.87 3.36 010 throat. 42808 ....... ........... A Excise pharynx lesion ...... 2.30 3.31 1.99 0.17 5.78 4.46 010 42809 ....... ........... A Remove pharynx foreign 1.81 2.46 1.40 0.13 4.40 3.34 010 body. 42810 ....... ........... A Excision of neck cyst ........ 3.25 5.05 3.53 0.25 8.55 7.03 090 42815 ....... ........... A Excision of neck cyst ........ 7.07 N/A 5.63 0.53 N/A 13.23 090 42820 ....... ........... A Remove tonsils and ade- 3.91 N/A 3.63 0.28 N/A 7.82 090 noids. -

A Rare Case of Perforated Descending Colon Cancer Complicated with a Fistula and Abscess of Left Iliopsoas and Ipsilateral Obturator Muscle
Hindawi Publishing Corporation Case Reports in Surgery Volume 2014, Article ID 128506, 5 pages http://dx.doi.org/10.1155/2014/128506 Case Report A Rare Case of Perforated Descending Colon Cancer Complicated with a Fistula and Abscess of Left Iliopsoas and Ipsilateral Obturator Muscle Alban Cacurri,1 Gaspare Cannata,1 Stefano Trastulli,2 Jacopo Desiderio,2 Antongiulio Mangia,1 Olga Adamenko,2 Eleonora Pressi,2 Giorgio Giovannelli,2 Giuseppe Noya,1 and Amilcare Parisi2 1 Department of General and Oncologic Surgery, University of Perugia, 06157 Perugia, Italy 2 Department of Digestive and Liver Surgery Unit, St. Maria Hospital, 05100 Terni, Italy Correspondence should be addressed to Gaspare Cannata; [email protected] Received 20 November 2013; Accepted 9 February 2014; Published 16 March 2014 Academic Editors: F. Catena and A. Cho Copyright © 2014 Alban Cacurri et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Perforation of descending colon cancer combined with iliopsoasabscessandfistulaformationisarareconditionandhasbeen reported few times. A 67-year-old man came to our first aid for an acute pain in the left iliac fossa, in the flank, and in the ipsilateral thigh. Ultrasonography and computed tomography revealed a left abdominal wall, retroperitoneal, and iliopsoas abscess that also involved the ipsilateral obturator muscle. It proceeded with an exploratory laparotomy that showed a tumor of the descending colon adhered and perforated in the retroperitoneum with abscess of the iliopsoas muscle on the left-hand side, with presence of a fistula and liver metastases. -

Pelvic Primary Staphylococcal Infection Presenting As a Thigh Abscess
Hindawi Publishing Corporation Case Reports in Surgery Volume 2013, Article ID 539737, 4 pages http://dx.doi.org/10.1155/2013/539737 Case Report Pelvic Primary Staphylococcal Infection Presenting as a Thigh Abscess T. O. Abbas General Surgery Department, Hamad General Hospital, Doha 3050, Qatar Correspondence should be addressed to T. O. Abbas; [email protected] Received 20 February 2013; Accepted 18 March 2013 Academic Editors: K. Honma, G. Rallis, and M. Zafrakas Copyright © 2013 T. O. Abbas. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Intra-abdominal disease can present as an extra-abdominal abscess and can follow several routes, including the greater sciatic foramen, obturator foramen, femoral canal, pelvic outlet, and inguinal canal. Nerves and vessels can also serve as a route out of the abdomen. The psoas muscle extends from the twelfth thoracic and fifth lower lumbar vertebrae to the lesser trochanter of thefemur, which means that disease in this muscle group can migrate along the muscle, out of the abdomen, and present as a thigh abscess. We present a case of a primary pelvic staphylococcal infection presenting as a thigh abscess. The patient was a 60-year-old man who presented with left posterior thigh pain and fever. Physical examination revealed a diffusely swollen left thigh with overlying erythematous, shiny, and tense skin. X-rays revealed no significant soft tissue lesions, ultrasound was suggestive of an inflammatory process, and MRI showed inflammatory changes along the left hemipelvis and thigh involving the iliacus muscle group, left gluteal region, and obturator internus muscle. -

Pediatric Review
CLINICAL REVIEW Application Type 21-227 Submission Number S-021 Submission Code SE-5 Letter Date January 31, 2008 Stamp Date January 31, 2008 PDUFA Goal Date July 31, 2008 Reviewer Name(s) Yuliya Yasinskaya, M.D. (risk/benefit, efficacy, labeling) Julie-Ann Crewalk, M.D. (clinical trial safety) Eileen Navarro, M.D. (postmarketing safety) Review Completion Date July 10, 2008 Established Name Caspofungin acetate (Proposed) Trade Name Cancidas® Therapeutic Class Enchinocandin antifungal Applicant Merck Priority Designation P Formulation lyophilized powder for infusion Dosing Regimen 50, 70mg/m2 Indications ◦ Empiric therapy of fungal infections in febrile neutropenic patients, ◦ Treatment of candidemia and the following Candida infections: intra- abdominal abscesses, peritonitis, and pleural space infections, ◦ Treatment of esophageal candidiasis, ◦ Treatment of refractory invasive aspergillosis Intended Population Children 3 months to 17 years 1 Clinical Review Yuliya Yasinskaya, M.D., Julie-Ann Crewalk, M.D,, and Eileen Navarro, M.D. NDA 21-227, S-021 Cancidas® (caspofungin acetate) Table of Contents 1 RECOMMENDATIONS/RISK BENEFIT ASSESSMENT 6 1 RECOMMENDATIONS/RISK BENEFIT ASSESSMENT 6 1.1 Recommendation on Regulatory Action.....................................................................................................6 1.1.1 Confirmation of efficacy 6 1.1.2 Confirmation of safety 9 1.2 Risk Benefit Assessment ..........................................................................................................................10