Dr. Richard Schlegel's Laboratory Co-Developed the Technology for The
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

HPV Vaccine: Global Effort Defeats Cancer-Causing Virus
HPV Vaccine: Global Effort Defeats Cancer-Causing Virus Georgetown University German Cancer Research Ctr (DKFZ) National Institutes of Health (NIH) University of Queensland, Australia University of Rochester Medical Center The world’s first vaccine against human papilloma viruses (HPV) is also the world’s first vaccine developed to specifically combat cancer. Distributed under the brand names Gardasil and Cervarix, by Merck & Co. and GlaxoSmithKline, respectively, the vaccine is widely known for its effectiveness against precursors of cervical cancer in women. The breakthrough medical advancement, recently approved for use in males, stands to benefit men too. According to the World Health Organization (WHO), some 500,000 women a year worldwide develop cervical cancer, and 274,000 die from the disease. Cervical cancer is caused by HPV and is the most common cancer affecting women in developing countries. The virus, however, does not restrain its attack to women or even to the female reproductive tract; there are more than 100 known types of HPV, and at least 13 are cancer-causing. WHO estimates it also causes 90 percent of anal cancers, 40 percent of cancers of the external genitalia, at least 12 percent of oropharyngeal (throat) cancer cases and at least 3 percent of oral cancer cases. In the United States, HPV is the most common sexually transmitted disease, according to the Centers for Disease Control and Prevention, and will infect at least 50 percent of sexually active people at some point in their lives. In other words, HPV strikes more humans than it spares and it continues to spread. The need to confront and prevent this threat is universally recognized. -
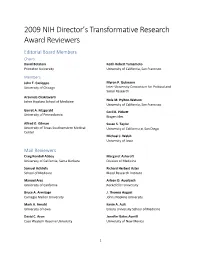
2009 NIH Director's Transformative Research Award Reviewers
2009 NIH Director’s Transformative Research Award Reviewers Editorial Board Members Chairs David Botstein Keith Robert Yamamoto Princeton University University of California, San Francisco Members John T. Cacioppo Myron P. Gutmann University of Chicago Inter-University Consortium for Political and Social Research Aravinda Chakravarti Johns Hopkins School of Medicine Nola M. Hylton-Watson University of California, San Francisco Garret A. Fitzgerald Cecil B. Pickett University of Pennsylvania Biogen Idec Alfred G. Gilman Susan S. Taylor University of Texas Southwestern Medical University of California at San Diego Center Michael J. Welsh University of Iowa Mail Reviewers Craig Kendall Abbey Margaret Ashcroft University of California, Santa Barbara Division of Medicine Samuel Achilefu Richard Herbert Aster School of Medicine Blood Research Institute Manuel Ares Arleen D. Auerbach University of California Rockefeller University Bruce A. Armitage J. Thomas August Carnegie Mellon University Johns Hopkins University Mark A. Arnold Kevin A. Ault University of Iowa Emory University School of Medicine David C. Aron Jennifer Bates Averill Case Western Reserve University University of New Mexico 1 Mary Helen Barcellos-Hoff Leslie A. Bruggeman New York University School of Medicine Case Western Reserve University David P. Bartel Peter Burkhard New Cambrige Center University of Connecticut Ralf Bartenschlager Alma L. Burlingame University of Heidelberg University of California, San Francisco Rashid Bashir Frederic D. Bushman University of Illinois at Urbana – Champaign University of Pennsylvania Carl A. Batt Robert William Caldwell Cornell University Medical College of Georgia Mark T. Bedford Phil Gordon Campbell Research Division Carnegie Mellon University Kevin D. Belfield Joseph Nicholas Cappella University of Central Florida University of Pennsylvania Andrew Steven Belmont William A. -

View Program
Addressing Problems Worth Solving The challenges we are confronting worldwide are both complex and daunting. In the next 20 years, the most important inventions will be those that address critical social and environmental issues, reaching and serving communities with the greatest needs. These inventions will deliver meaningful change, solve urgent problems, and create sustainable economic value for all. The Lemelson Foundation focuses on problems that are worth solving—and not simply problems that can be solved. We recognize the need for a strong supportive invention ecosystem to make this happen. We seek to inspire inventors to know that they can make a difference. We work to ensure that the next generation of inventors can become agents of positive change. Find out more about how we provide support to foster inventions to improve lives at: www.lemelson.org/impactinventing Distinguished Colleagues: On behalf of the Board of Directors, it is my distinct pleasure to welcome you to the fourth annual meeting of the National Academy of Inventors, held this year at the California Institute of Technology and the Langham Huntington Hotel in Pasadena. In addition to a compelling program filled with outstanding speakers, our meet- ing sets the stage for our continued growth and future as an organization. We are grateful for the support of our sponsors and host institutions in making this conference possible. We thank our presenters, panelists, co-chairs, and the conference program committee for their hard work, and we thank you for being here. We are delighted to welcome Steven Chu, Esther Takeuchi and Richard DiMarchi as our featured keynote speakers and look forward to hearing their insights on innovation. -

The Big Ten: from Theory to Mainstream in Personalized Healthcare
The Big Ten: From Theory to Mainstream in Personalized Healthcare Item Type Brochure/Program Authors University of Maryland, Baltimore. School of Medicine Publication Date 2014-11-17 Keywords University of Maryland, Baltimore. School of Medicine--Events Download date 25/09/2021 10:24:23 Item License https://creativecommons.org/licenses/by-nc-nd/4.0/ Link to Item http://hdl.handle.net/10713/4300 The Big Ten: From Theory to Mainstream in Personalized Healthcare Tenth Annual Symposium on Translational Research in Molecular Pathology Date: Monday, November 17, 2014 Location: MSTF Auditorium University of Maryland, Baltimore 9:00am-4:00pm A Third Century Where Discovery Transforms 685 W. Baltimore Street Baltimore, MD21201 Medicine About the Division of Molecular Pathology The Division of Molecular Pathology Faculty The Division of Molecular Pathology is a research division within in the Department of Pathology, the University of Maryland School of Medicine, Burke, Allen P, M.D., Clinical Associate Professor which was established in 2005 under the leadership of Dr. Richard Y. Zhao. Castellani, Rudolph J Jr., M.D., Professor Currently there a total 17 faculty members in the division who conduct Constantine, Niel T., Ph.D., Professor research in various area of molecular pathology. Mission of the Division of Fulton, Amy M, Ph.D., Professor Molecular Pathology is to 1) support the Department of Pathology and the Hamburger, Anne W., PhD, Professor (retired) University of Maryland Medical School's mission for excellence in research, Jiang, Feng, M.D., Ph.D., Assistant Professor teaching and clinical services, 2) foster translational research in the Johnson, Jennifer K, Ph.D., Assistant Professor Department of Pathology in the area of Molecular Pathology, and 3) serve as a Luo, Jianyuan "Jack", PhD, Associate Professor research unit in reaching out and psromote inter-disciplinary collaboration in Mann, Dean L, M.D., Professor Molecular Pathology. -

CURRICULUM VITAE Alfred Bennett Jenson
CURRICULUM VITAE Alfred Bennett Jenson, MD 3715 Glen Bluff Road, Louisville, KY 40222 PERSONAL DATA Phone (Work) 1-502-852-1114 (Home) 1-502-417-9894 EDUCATION B.A., Texas Christian University, Texas, 1957-61 (Cum Laude) M.S., Baylor University (College of Medicine), Texas, l964-66 M.D., Baylor College of Medicine, Texas, l961-66, with honor Internship, Department of Medicine, Baylor College of Medicine Affiliated Hospital Program, l966-67 Residency, Department of Pathology, Baylor College of Medicine Affiliated Hospital Program, l967-70 American Association of Immunology Summer Course, l970 Research Trainee, U.S. Public Health Service, l967-71 (Joe Melnick, Ph.D., Mentor) Postdoctoral Fellow of the National Multiple Sclerosis Society, l973-75 Basic Program Officials Guide to Contracting, l979 Sabbatical, National German Cancer Institute (DKFZ), Heidelberg, Germany, October- December, 1999. POSITIONS Chief Resident, Pathology, Ben Taub General Hospital, Houston, Texas, l969-70 (Harlan Spjut, MD, Pathology Chief of Staff). Instructor, Department of Pathology, Baylor College of Medicine, l970-71. Instructor in Pathology, Department of Optometry, University of Houston, Texas, l970-71 Comparative Pathologist, USAR, Veterinary Medicine Division, Veterinary Pathology Branch, Edgewood Arsenal, MD, l971-73. Consultant, Cancer Cytology, Maryland State Department of Public Health and Hygiene, l972-73 Research Associate in Immunopathology, Scripps Clinic and Research Foundation, La Jolla, CA, 1973-75 (Frank Dixon, MD, Mentor). Senior Medical Surgeon, USPHS, Laboratory of Oral Medicine, National Institutes of Dental Research, National Institutes of Health, MD, l975-80 (Abner Notkins, MD, Laboratory Chief). Associate Professor, Department of Pathology, Georgetown University Schools of Medicine and Dentistry, l980-1989. Vice-Chairman, Department of Pathology, Georgetown University Schools of Medicine and Dentistry, l983-85. -

Viable Adenovirus Vaccine Prototypes: High-Level Production of a Papillomavirus Capsid Antigen from the Major Late Transcriptional Unit
Viable adenovirus vaccine prototypes: High-level production of a papillomavirus capsid antigen from the major late transcriptional unit Michael Berg†, Julie DiFatta†‡, Egbert Hoiczyk†, Richard Schlegel§, and Gary Ketner†¶ †W. Harry Feinstone Department of Molecular Microbiology and Immunology, Johns Hopkins Bloomberg School of Public Health, 615 North Wolfe Street, Baltimore, MD 21205; and §Department of Pathology, Georgetown University Medical Center, Washington, DC 20007 Communicated by Diane E. Griffin, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, February 4, 2005 (received for review October 21, 2004) Safe, effective, orally delivered, live adenovirus vaccines have been The eventual target of this work is human papillomavirus, the in use for three decades. Recombinant derivatives of the live etiologic agent of cervical cancer. More than 500,000 cases of adenovirus vaccines may prove an economical alternative to cur- cervical cancer are diagnosed annually, and Ͼ200,000 women die rent vaccines for a variety of diseases. To explore that possibility, each year from the disease (3). Vaccination with empty virus-like we constructed a series of recombinants that express the major particles (VLPs), which spontaneously assemble from recombi- capsid protein (L1) of canine oral papillomavirus (COPV), a model nant papillomavirus L1 capsid protein, confers immunity to for mucosal human papillomavirus (HPV) infection. Vaccination papillomavirus-induced tumors in animal systems (4–6). VLPs with virus-like particles (VLPs) composed of recombinant HPV L1 induce strong immune responses in humans (7, 8), and a VLP completely prevents persistent HPV infection [Koutsky, L. A., Ault, vaccine was 100% effective in preventing persistent infection K. A., Wheeler, C.