Hand Sanitizers: a Review on Formulation Aspects, Adverse Effects, and Regulations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
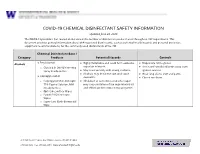
EH&S COVID-19 Chemical Disinfectant Safety Information
COVID-19 CHEMICAL DISINFECTANT SAFETY INFORMATION Updated June 24, 2020 The COVID-19 pandemic has caused an increase in the number of disinfection products used throughout UW departments. This document provides general information about EPA-registered disinfectants, such as potential health hazards and personal protective equipment recommendations, for the commonly used disinfectants at the UW. Chemical Disinfectant Base / Category Products Potential Hazards Controls ● Ethyl alcohol Highly flammable and could form explosive Disposable nitrile gloves Alcohols ● ● vapor/air mixtures. ● Use in well-ventilated areas away from o Clorox 4 in One Disinfecting Spray Ready-to-Use ● May react violently with strong oxidants. ignition sources ● Alcohols may de-fat the skin and cause ● Wear long sleeve shirt and pants ● Isopropyl alcohol dermatitis. ● Closed toe shoes o Isopropyl Alcohol Antiseptic ● Inhalation of concentrated alcohol vapor 75% Topical Solution, MM may cause irritation of the respiratory tract (Ready to Use) and effects on the central nervous system. o Opti-Cide Surface Wipes o Powell PII Disinfectant Wipes o Super Sani Cloth Germicidal Wipe 201 Hall Health Center, Box 354400, Seattle, WA 98195-4400 206.543.7262 ᅵ fax 206.543.3351ᅵ www.ehs.washington.edu ● Formaldehyde Formaldehyde in gas form is extremely Disposable nitrile gloves for Aldehydes ● ● flammable. It forms explosive mixtures with concentrations 10% or less ● Paraformaldehyde air. ● Medium or heavyweight nitrile, neoprene, ● Glutaraldehyde ● It should only be used in well-ventilated natural rubber, or PVC gloves for ● Ortho-phthalaldehyde (OPA) areas. concentrated solutions ● The chemicals are irritating, toxic to humans ● Protective clothing to minimize skin upon contact or inhalation of high contact concentrations. -

Hand Hygiene Solutions
PRODUCT OVERVIEWS Hand Hygiene Solutions Healing Hands Need Help, Too. Almost 80% of infectious Hand hygiene compliance Product selection matters diseases are transmitted rates are often very low Products containing aloe vera, via touch Outpatient clinics: Studies vitamin E and other emollients One of the most common have shown that hand hygiene can help to soothe and protect modes of transmission is frequency amongst clinic staff hands and even promote hand via the hands of healthcare ranges from 11-50%.2, 3 hygiene compliance.4 professionals.1 Designed for the demanding needs of healthcare professionals, Clorox Healthcare® provides a wide array of hand hygiene solutions formulated for frequent hand hygiene in healthcare settings. References 1. Tierno, P. The Secret Life of Germs. New York, NY, USA: Atria Books, 2001. 2. Kukanich KS, Kaur R, Freeman LC, Powell DA. Evaluation of a hand hygiene campaign in outpatient health care clinics. Am J Nurs. 2013 Mar;113(3):36-42. 3. Thompson D, Bowdey L, Brett M, Cheek, Using medical student observers of infection prevention, hand hygiene, and injection safety in outpatient settings: A cross-sectional survey. J Am J Infect. Control 2016; 44(4):374–380. 4. World Health Organization. WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care Is Safer Care. 2009. https://www.ncbi.nlm.nih.gov/books/NBK144051/ (Accessed 22 February 2017) 5. CDC. “Handwashing: Clean Hands Save Lives-Show Me the Science-Why Wash Your Hands?” https://www.cdc.gov/handwashing/why-handwashing.html (Accessed 15 March 2017). Hand hygiene is one of the most effective ways to stop the spread of germs and keep patients, staff and visitors safe.5 Our portfolio of hand hygiene solutions can be used to clean and soothe hands throughout your facility-from reception areas, to patient care areas to break rooms and offices. -

Ethanol Rins and Hand Sanitizer
UNITED STATES ENVIRONMENTAL PROTECTION AGENCY NATIONAL VEHICLE AND FUEL EMISSIONS LABORATORY 2565 PLYMOUTH ROAD ANN ARBOR, MICHIGAN 48105-2498 OFFICE OF AIR AND RADIATION May 11, 2020 Re: Ethanol RINs and Hand Sanitizer Production for EP3 Pathway Ethanol Facilities during the COVID-19 Public Health Emergency Dear Ethanol Producers: EPA administers the Renewable Fuel Standard (RFS) program, including determining what volumes of fuel ethanol qualify for tradable credits (RINs) under the program. In 2014, as part of the RFS Program in 40 C.F.R. Part 80, we created the Efficient Producer Petition Process (EP3) as a streamlined process for corn starch and grain sorghum ethanol producers to demonstrate that their fuel satisfies the lifecycle greenhouse gas (GHG) reduction requirements to qualify for RINs. Consistent with 40 C.F.R. § 80.1416, over 80 dry mill ethanol plants in the United States have been approved for EP3 pathways. Given the current 2019 coronavirus disease (COVID-19), we understand that some consumers and health care professionals are currently experiencing difficulties accessing alcohol-based hand sanitizers. To enhance the availability of hand sanitizer products, the Food and Drug Administration (FDA) has issued a number of temporary policies, including temporary guidance for producers of alcohol for hand sanitizer.1 Based on input from industry, we understand fuel ethanol facilities can quickly and significantly enhance the availability of alcohol suitable for hand sanitizer production. Ethanol production through an EP3 pathway is limited to 200-proof ethanol, whereas alcohol suitable for use as an ingredient in hand sanitizer (hand sanitizer alcohol) is commonly produced as 190-proof ethanol. -

1 Brief Report: the Virucidal Efficacy of Oral Rinse Components Against SARS-Cov-2 in Vitro Evelina Statkute1†, Anzelika Rubin
bioRxiv preprint doi: https://doi.org/10.1101/2020.11.13.381079; this version posted November 13, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-ND 4.0 International license. Brief Report: The Virucidal Efficacy of Oral Rinse Components Against SARS-CoV-2 In Vitro Evelina Statkute1†, Anzelika Rubina1†, Valerie B O’Donnell1, David W. Thomas2† Richard J. Stanton1† 1Systems Immunity University Research Institute, Division of Infection & Immunity, School of Medicine, Heath Park, Cardiff, CF14 4XN 2Advanced Therapies Group, School of Dentistry, Cardiff University, Heath Park, Cardiff CF14 4XY, UK †These authors contributed equally * Correspondence: [email protected], [email protected] Running title: Virucidal Activity of Mouthwashes Keywords: SARS-CoV2, mouthwash, lipid, envelope Disclosure: Venture Life Group plc provided information on mouthwash formulations employed in the study, but had no role in funding, planning, execution, analysis or writing of this study. A separate study funded to Cardiff University by Venture Life Group is assessing in vivo efficacy of CPC in patients with COVID19. The investigators declare no direct conflicts exist. 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.11.13.381079; this version posted November 13, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-ND 4.0 International license. -

Quaternary Ammonium Compounds
FACT SHEET: Quaternary Ammonium Compounds Quaternary ammonium compounds, also known as “quats” or “QACs,” include a number of chemicals used as sanitizers and disinfectants, including benzalkonium chloride, benzethonium chloride, cetalkonium chloride, cetrimide, cetrimonium bromide, cetylpyridinium chloride, glycidyl trimethyl, ammonium chloride, and stearalkonium chloride.[i] In general, quats cause toxic effects through all Mutagenicity routes of exposure including inhalation, Some quats have shown to be mutagenic and to ingestion, dermal application, and irrigation of damage animal DNA and DNA in human body cavities. Exposure to diluted solutions may lymphocytes at much lower levels than are result in mild irritation, while concentrated present in cleaning chemicals.[6] solutions are corrosive, causing burns to the skin and mucous Membranes. They can produce Antimicrobial Resistance systemic toxicity and can also cause allergic Genes have been discovered that mediate reactions.[2] resistance to quats. There has been an association of some of these genes with beta lactamase genes, Asthma and Allergies raising concern for a relationship between Of particular interest with regard to use as disinfectant resistance and antibiotic resistance.[7] disinfectants in the COVID-19 pandemic, quats increase the risk for asthma and allergic Reproductive Toxicity sensitization. Evidence from occupational Mice whose cages were cleaned with QACs had exposures shows increased risk of rhinitis and very low fertility rates. [8] Exposure to a common asthma -
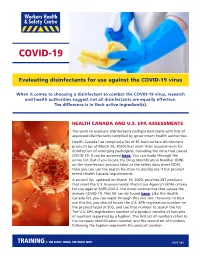
Evaluating Disinfectants for Use Against the COVID-19 Virus
When it comes to choosing a disinfectant to combat the COVID-19 virus, research and health authorities suggest not all disinfectants are equally effective. The difference is in their active ingredient(s). HEALTH CANADA AND U.S. EPA ASSESSMENTS The work to evaluate disinfectants perhaps best starts with lists of approved disinfectants compiled by government health authorities. Health Canada has compiled a list of 85 hard surface disinfectant products (as of March 20, 2020) that meet their requirements for disinfection of emerging pathogens, including the virus that causes COVID-19. It can be accessed here. You can wade through the entire list. But if you locate the Drug Identification Number (DIN) on the disinfectant product label or the safety data sheet (SDS), then you can use the search function to quickly see if the product meets Health Canada requirements. A second list, updated on March 19, 2020, provides 287 products that meet the U.S. Environmental Protection Agency’s (EPA) criteria for use against SARS-CoV-2, the novel coronavirus that causes the disease COVID-19. This list can be found here. Like the Health Canada list, you can wade through this one too. However, to best use this list, you should locate the U.S. EPA registration number on the product label or SDS, and use that number to search the list. The U.S. EPA registration number of a product consists of two sets of numbers separated by a hyphen. The first set of numbers refers to the company identification number, and the second set of numbers following the hyphen represents the product number. -

Tonsillopharyngitis - Acute (1 of 10)
Tonsillopharyngitis - Acute (1 of 10) 1 Patient presents w/ sore throat 2 EVALUATION Yes EXPERT Are there signs of REFERRAL complication? No 3 4 EVALUATION Is Group A Beta-hemolytic Yes DIAGNOSIS Streptococcus (GABHS) • Rapid antigen detection test infection suspected? (RADT) • roat culture No TREATMENT EVALUATION No A Supportive management Is GABHS confi rmed? B Pharmacological therapy (Non-GABHS) Yes 5 TREATMENT A EVALUATE RESPONSEMIMS Supportive management TO THERAPY C Pharmacological therapy • Antibiotics Poor/No Good D Surgery, if recurrent or complicated response response REASSESS PATIENT COMPLETE THERAPY & REVIEW THE DIAGNOSIS© Not all products are available or approved for above use in all countries. Specifi c prescribing information may be found in the latest MIMS. B269 © MIMS Pediatrics 2020 Tonsillopharyngitis - Acute (2 of 10) 1 ACUTE TONSILLOPHARYNGITIS • Infl ammation of the tonsils & pharynx • Etiologies include bacterial (group A β-hemolytic streptococcus, Haemophilus infl uenzae, Fusobacterium sp, etc) & viral (infl uenza, adenovirus, coronavirus, rhinovirus, etc) pathogens • Sore throat is the most common presenting symptom in older children TONSILLOPHARYNGITIS 2 EVALUATION FOR COMPLICATIONS • Patients w/ sore throat may have deep neck infections including epiglottitis, peritonsillar or retropharyngeal abscess • Examine for signs of upper airway obstruction Signs & Symptoms of Sore roat w/ Complications • Trismus • Inability to swallow liquids • Increased salivation or drooling • Peritonsillar edema • Deviation of uvula -

FDA-2015-N-0101; and FDA-2016-N-0124
DE PARTMENT OF HEALTH AND HUMAN SERVICES Food and Drug Administration Silver Spring MD 20993 November 18, 2020 Docket Nos. FDA-1975-N-0012; FDA-2015-N-0101; and FDA-2016-N-0124 The American Cleaning Institute Attention: James Kim, PhD Vice President, Science and Regulatory Affairs 1401 H Street, N.W. Suite 700 Washington, D.C. 20005 Re: Benzalkonium Chloride, Benzethonium Chloride, Chloroxylenol, Ethanol, and Povidone-Iodine Dear Dr. Kim: This letter responds to The American Cleaning Institute’s (ACI’s) July 14, 2020 communication regarding the deferral from final rulemaking under the over-the-counter (OTC) Drug Review on benzalkonium chloride, benzethonium chloride, chloroxylenol, ethanol, and povidone-iodine for use in nonprescription (often referred to as over-the-counter or OTC) consumer antiseptic wash, health care antiseptic, and consumer antiseptic rub drug products. In March 2016, FDA issued letters granting requests to defer three active ingredients— benzalkonium chloride, benzethonium chloride, and chloroxylenol—from inclusion in the final rulemaking for the December 2013 proposed rule for OTC consumer antiseptic washes (78 FR 76444). Similarly, in January 2017, FDA issued letters granting requests to defer six active ingredients—benzalkonium chloride, benzethonium chloride, chloroxylenol, ethanol, povidone- iodine, and isopropyl alcohol—from inclusion in the final rulemaking for the May 2015 proposed rule for OTC health care antiseptics (80 FR 25166). In October 2017, FDA issued letters granting requests to defer three active -

Comparison of Effectiveness Disinfection of 2%
ORIGINAL RESEARCH Journal of Dentomaxillofacial Science (J Dentomaxillofac Sci ) December 2018, Volume 3, Number 3: 169-171 P-ISSN.2503-0817, E-ISSN.2503-0825 Comparison of effectiveness disinfection of 2% Original Research glutaraldehyde and 4.8% chloroxylenol on tooth extraction instruments in the Department of Oral CrossMark http://dx.doi.org/10.15562/jdmfs.v3i2.794 Maxillofacial Surgery, Faculty of Dentistry, University of North Sumatera Month: December Ahyar Riza,* Isnandar, Indra B. Siregar, Bernard Volume No.: 3 Abstract Objective: To compare disinfecting effectiveness of 2% glutaraldehyde while the control group was treated with 4.8% chloroxylenol. Each Issue: 2 and 4.8% chloroxylenol on tooth extraction instruments at the instrument was pre-cleaned using a brush, water and soap for both Department of Oral Surgery, Faculty of Dentistry, University of North groups underwent the disinfection process. Sumatera. Results: The results were statistically analyzed using Mann-Whitney Material and Methods: This was an experimental study with post- Test. The comparison between glutaraldehyde and chloroxylenol First page No.: 147 test only control group design approach. Purposive technique is showed a significant difference to the total bacteria count on applied to collect samples which are lower molar extraction forceps. In instrument after disinfection (p=0.014 < 0.05). this study, sample were divided into 2 groups and each consisting of 18 Conclusion: 2% glutaraldehyde was more effective than 4.8% P-ISSN.2503-0817 instruments. The treatment group was treated with 2% glutaraldehyde chloroxylenol at disinfecting lower molar extraction forceps. Keyword: Disinfection, Glutaraldehyde, Chloroxylenol, Forceps E-ISSN.2503-0825 Cite this Article: Riza A, Siregar IB, Isnandar, Bernard. -

Bio-Butanol Production from Glycerol with Clostridium
Lin et al. Biotechnol Biofuels (2015) 8:168 DOI 10.1186/s13068-015-0352-6 RESEARCH Open Access Bio‑butanol production from glycerol with Clostridium pasteurianum CH4: the effects of butyrate addition and in situ butanol removal via membrane distillation De‑Shun Lin1, Hong‑Wei Yen2, Wei‑Chen Kao1, Chieh‑Lun Cheng1, Wen‑Ming Chen3, Chieh‑Chen Huang4 and Jo‑Shu Chang1,4,5* Abstract Background: Clostridium pasteurianum CH4 was used to produce butanol from glycerol. The performance of butanol fermentation was improved by adding butyrate as the precursor to trigger the metabolic pathway toward butanol production, and by combining this with in situ butanol removal via vacuum membrane distillation (VMD) to avoid the product inhibition arising from a high butanol concentration. 1 Results: Adding 6 g L− butyrate as precursor led to an increase in the butanol yield from 0.24 to 0.34 mol butanol 1 (mol glycerol)− . Combining VMD and butyrate addition strategies could further enhance the maximum effective 1 1 butanol concentration to 29.8 g L− , while the yield was also improved to 0.39 mol butanol (mol glycerol)− . The butanol concentration in the permeate of VMD was nearly five times higher than that in the feeding solution. Conclusions: The proposed butyrate addition and VMD in situ butanol removal strategies are very effective in enhancing both butanol titer and butanol yield. This would significantly enhance the economic feasibility of fermen‑ tative production of butanol. The VMD-based technology not only alleviates the inhibitory effect of butanol, but also markedly increases butanol concentration in the permeate after condensation, thereby making downstream process‑ ing easier and more cost-effective. -

NINDS Custom Collection II
ACACETIN ACEBUTOLOL HYDROCHLORIDE ACECLIDINE HYDROCHLORIDE ACEMETACIN ACETAMINOPHEN ACETAMINOSALOL ACETANILIDE ACETARSOL ACETAZOLAMIDE ACETOHYDROXAMIC ACID ACETRIAZOIC ACID ACETYL TYROSINE ETHYL ESTER ACETYLCARNITINE ACETYLCHOLINE ACETYLCYSTEINE ACETYLGLUCOSAMINE ACETYLGLUTAMIC ACID ACETYL-L-LEUCINE ACETYLPHENYLALANINE ACETYLSEROTONIN ACETYLTRYPTOPHAN ACEXAMIC ACID ACIVICIN ACLACINOMYCIN A1 ACONITINE ACRIFLAVINIUM HYDROCHLORIDE ACRISORCIN ACTINONIN ACYCLOVIR ADENOSINE PHOSPHATE ADENOSINE ADRENALINE BITARTRATE AESCULIN AJMALINE AKLAVINE HYDROCHLORIDE ALANYL-dl-LEUCINE ALANYL-dl-PHENYLALANINE ALAPROCLATE ALBENDAZOLE ALBUTEROL ALEXIDINE HYDROCHLORIDE ALLANTOIN ALLOPURINOL ALMOTRIPTAN ALOIN ALPRENOLOL ALTRETAMINE ALVERINE CITRATE AMANTADINE HYDROCHLORIDE AMBROXOL HYDROCHLORIDE AMCINONIDE AMIKACIN SULFATE AMILORIDE HYDROCHLORIDE 3-AMINOBENZAMIDE gamma-AMINOBUTYRIC ACID AMINOCAPROIC ACID N- (2-AMINOETHYL)-4-CHLOROBENZAMIDE (RO-16-6491) AMINOGLUTETHIMIDE AMINOHIPPURIC ACID AMINOHYDROXYBUTYRIC ACID AMINOLEVULINIC ACID HYDROCHLORIDE AMINOPHENAZONE 3-AMINOPROPANESULPHONIC ACID AMINOPYRIDINE 9-AMINO-1,2,3,4-TETRAHYDROACRIDINE HYDROCHLORIDE AMINOTHIAZOLE AMIODARONE HYDROCHLORIDE AMIPRILOSE AMITRIPTYLINE HYDROCHLORIDE AMLODIPINE BESYLATE AMODIAQUINE DIHYDROCHLORIDE AMOXEPINE AMOXICILLIN AMPICILLIN SODIUM AMPROLIUM AMRINONE AMYGDALIN ANABASAMINE HYDROCHLORIDE ANABASINE HYDROCHLORIDE ANCITABINE HYDROCHLORIDE ANDROSTERONE SODIUM SULFATE ANIRACETAM ANISINDIONE ANISODAMINE ANISOMYCIN ANTAZOLINE PHOSPHATE ANTHRALIN ANTIMYCIN A (A1 shown) ANTIPYRINE APHYLLIC -

In Vivo Evaluation of the Virucidal Efficacy of Chlorhexidine and Povidone-Iodine Mouthwashes Against Salivary SARS-Cov-2
medRxiv preprint doi: https://doi.org/10.1101/2021.03.07.21252302; this version posted March 17, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-NC-ND 4.0 International license . Title: In vivo evaluation of the virucidal efficacy of Chlorhexidine and Povidone-iodine mouthwashes against salivary SARS-CoV-2. Rola Elzein1*, Fadi Abdel-Sater2*, Soha Fakhreddine3, Pierre Abi Hanna3, Rita Feghali4, Hassan Hamad5, Fouad Ayoub6 ¹Department of Pediatric Dentistry and Public Dental Health, Faculty of Dental Medicine, Lebanese University, Beirut, Lebanon 2Laboratory of Cancer Biology and Cellular Immunology, Department of Biological Sciences, Faculty of Sciences, Lebanese University, Beirut, Lebanon 3Infectious Diseases division, Rafik Hariri University Hospital, Beirut, Lebanon 4Department of Laboratory Medicine, Rafik Hariri University Hospital, Beirut, Lebanon 5Medical care Laboratory, Faculty of Public Health IV, Lebanese University, Zahle, Lebanon 6Department of Forensic Odontology, Human Identification and Anthropology, Faculty of Dental Medicine, Lebanese University, Beirut, Lebanon *CORRESPONDING AUTHORS: Rola ELZEIN; Mobile number: 009613252480; Email address: [email protected] Fadi Abdelsater; Mobile number: 009613781176; Email address: [email protected] NOTE: This preprint reports new research that has not been certified by peer review and should not be used to guide clinical practice. medRxiv preprint doi: https://doi.org/10.1101/2021.03.07.21252302; this version posted March 17, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.