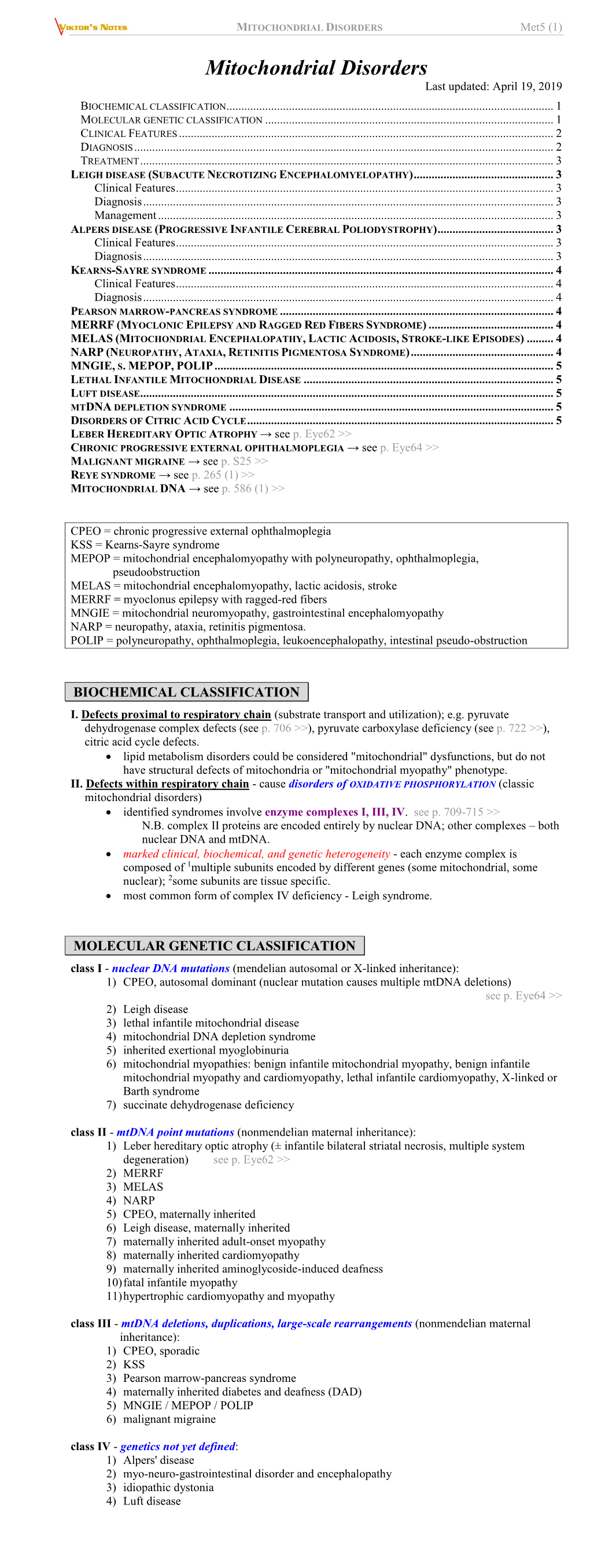
Met5. Mitochondrial Disorders.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Family Phenotypic Heterogeneity Caused by Mitochondrial DNA Mutation A3243G Heterogeneidade Fenotípica De Uma Família Causada
Alves D, et al. Phenotypic heterogeneity of inherited diabetes and deafness, Acta Med Port 2017 Jul-Aug;30(7-8):581-585 REFERENCES 1. Bywaters EG. Still’s disease in the adult. Ann Rheum Dis. 1971;30:121– with emphasis on organ failure. Semin Arthritis Rheum. 1987;17:39–57. 33. 9. Ohta A, Yamaguchi M, Tsunematsu T, Kasukawa R, Mizushima H, 2. Efthimiou P, Paik PK, Bielory L. Diagnosis and management of adult Kashiwagi H, et al. Adult Still’s disease: a multicenter survey of Japanese onset Still’s disease. Ann Rheum Dis. 2006;65:564–72. patients. J Rheumatol. 1990;17:1058–63. 3. Cheema GS, Quismorio FP. Pulmonary involvement in adult-onset Still’s 10. Cagatay Y, Gul A, Cagatay A, Kamali S, Karadeniz A, Inanc M, et al. disease. Curr Opin Pulm Med. 1999;5:305–9. Adult-onset Still’s disease. Int J Clin Pract. 2009;63:1050–5. 4. Zeng T, Zou YQ, Wu MF, Yang CD. Clinical features and prognosis 11. Riera E, Olivé A, Narváez J, Holgado S, Santo P, Mateo L, et al. CASO CLÍNICO of adult-onset still’s disease: 61 cases from China. J Rheumatol. Adult onset Still’s disease: review of 41 cases. Clin Exp Rheumatol. 2009;36:1026–31. 2011;29:331–6. 5. Yamaguchi M, Ohta A, Tsunematsu T, Kasukawa R, Mizushima Y, 12. Chen PD, Yu SL, Chen S, Weng XH. Retrospective study of 61 patients Kashiwagi H, et al. Preliminary criteria for classification of adult Still’s with adult-onset Still’s disease admitted with fever of unknown origin in disease. -

Identification of P.A684V Missense Mutation in the WFS1 Gene As a Frequent Cause of Autosomal Dominant Optic Atrophy and Hearing
RESEARCH ARTICLE Identification of p.A684V Missense Mutation in the WFS1 Gene as a Frequent Cause of Autosomal Dominant Optic Atrophy and Hearing Impairment Nanna D. Rendtorff,1 Marianne Lodahl,1 Houda Boulahbel,2 Ida R. Johansen,1 Arti Pandya,3 Katherine O. Welch,4 Virginia W. Norris,4 Kathleen S. Arnos,4 Maria Bitner-Glindzicz,5 Sarah B. Emery,6 Marilyn B. Mets,7 Toril Fagerheim,8 Kristina Eriksson,9 Lars Hansen,1 Helene Bruhn,10 Claes M€oller,11 Sture Lindholm,12 Stefan Ensgaard,13 Marci M. Lesperance,6 and Lisbeth Tranebjaerg1,14*,† 1Wilhelm Johannsen Centre for Functional Genome Research, Department of Cellular and Molecular Medicine (ICMM), The Panum Institute, University of Copenhagen, Copenhagen, Denmark 2Biotech Research & Innovation Centre (BRIC), University of Copenhagen, Copenhagen, Denmark 3Department of Human and Molecular Genetics, Virginia Commonwealth University, Richmond, Virginia 4Department of Biology, Gallaudet University, Washington DC 5UCL Institute of Child Health, London, UK 6Division of Pediatric Otolaryngology, Department of Otolaryngology-Head and Neck Surgery, UniversityofMichiganHealthSystem,AnnArbor,Michigan 7Departments of Ophthalmology and Surgery, Feinberg School of Medicine, Northwestern University, Evanston, Illinois 8Division of Child and Adolescent Health, Department of Medical Genetics, University Hospital of North Norway, Tromsø, Norway 9Department of Ophthalmology, Lundby Hospital, Gothenburg, Sweden 10Division of Metabolic Diseases, Department of Laboratory Medicine, Karolinska Institute, Karolinska University Hospital, Stockholm, Sweden 11Department of Audiology/Disability Research (SIDR), O¨rebro University, Sweden 12Department of Audiology, County Hospital, Kalmar, Sweden 13Department of Psychiatrics, Stockholm, Sweden 14Department of Audiology, Bispebjerg Hospital, Copenhagen, Denmark Received 19 July 2010; Accepted 2 February 2011 Optic atrophy (OA) and sensorineural hearing loss (SNHL) are these additional eight families. -
Maternally Inherited Diabetes and Deafness (MIDD) Syndrome with M.3243A>G Mutation Associated with Renal Failure — a Case Report
CASE REPORT ISSN 2450–7458 Grzegorz Kade1, Sebastian Krzysztof Spaleniak2, Bogdan Brodacki3, Agnieszka Pollak4, Dariusz Moczulski2, Monika Ołdak4, Marek Saracyn5 1Department of Internal Medicine, Nephrology and Dialysis, Military Institute of Medicine, Warsaw, Poland 2Department of Internal Medicine and Nephrodiabetology, Medical University of Lodz, Poland 3Neurological Clinic, Military Institute of Medicine, Warsaw, Poland 4Department of Genetics, Institute of Physiology and Pathology of Hearing, Warsaw, Poland 5Department of Endocrinology and Isotope Therapy, Military Institute of Medicine, Warsaw, Poland Maternally inherited diabetes and deafness (MIDD) syndrome with m.3243A>G mutation associated with renal failure — a case report ABSTRACT before as a cause of renal failure in MIDD patients. Maternally-inherited diabetes with deafness (MIDD) (Clin Diabetol 2020; 9; 6: 475–478) is a rare form of monogenic diabetes that results, in most cases, from an A-to-G transition at position 3243 Key words: mitochondrial diabetes, sensorineural of mitochondrial DNA (m.3243A>G). The clinical pres- deafness, m.3243A>G mutation, renal failure, entation of m.3243A>G mutation is variable, ranging incomplete distal renal tubular acidosis from mild to severe phenotypes. Diabetes is often accompanied by sensorineural deafness, cardiomyo- Introduction pathy, neuromuscular, psychiatric disorders, macular The relationship between the m.3243A>G muta- dystrophy and renal failure (kidney manifestations in tion and maternally inherited diabetes mellitus and adults presenting with this mutation remain poorly deafness syndrome (MIDD) was first described in 1992 defined). by Ballinger et al. [1] Another disease associated with The study presents a case of a 40-years-old woman this mitochondrial mutation is MELAS syndrome (mito- with a history of bilateral sensorineural deafness, chondrial encephalopathy, lactic acidosis, and stroke- renal failure and diabetes that was diagnosed due to like episodes) which has been described by Pavlakis et increasing muscle weakness during exercise. -

The Role of Mitochondrial Mutations and Chronic Inflammation in Diabetes
International Journal of Molecular Sciences Review The Role of Mitochondrial Mutations and Chronic Inflammation in Diabetes Siarhei A. Dabravolski 1, Varvara A. Orekhova 2,*, Mirza S. Baig 3, Evgeny E. Bezsonov 2,4 , Antonina V. Starodubova 5,6 , Tatyana V. Popkova 7 and Alexander N. Orekhov 2,4 1 Department of Clinical Diagnostics, Vitebsk State Academy of Veterinary Medicine, 210026 Vitebsk, Belarus; [email protected] 2 Laboratory of Angiopathology, Institute of General Pathology and Pathophysiology, 125315 Moscow, Russia; [email protected] (E.E.B.); [email protected] (A.N.O.) 3 Department of Biosciences and Biomedical Engineering (BSBE), Indian Institute of Technology Indore (IITI), Simrol 456552, India; [email protected] 4 Institute of Human Morphology, 117418 Moscow, Russia 5 Federal Research Centre for Nutrition, Biotechnology and Food Safety, 109240 Moscow, Russia; [email protected] 6 Therapy Faculty, Pirogov Russian National Research Medical University, 117997 Moscow, Russia 7 V.A. Nasonova Institute of Rheumatology, 115522 Moscow, Russia; [email protected] * Correspondence: [email protected]; Tel.: +7-(495)-415-95-94; Fax: +7-(495)-415-95-94 Abstract: Diabetes mellitus and related disorders significantly contribute to morbidity and mortality worldwide. Despite the advances in the current therapeutic methods, further development of anti- diabetic therapies is necessary. Mitochondrial dysfunction is known to be implicated in diabetes development. Moreover, specific types of mitochondrial diabetes have been discovered, such as MIDD (maternally inherited diabetes and deafness) and DAD (diabetes and Deafness). Hereditary Citation: Dabravolski, S.A.; mitochondrial disorders are caused by certain mutations in the mitochondrial DNA (mtDNA), which Orekhova, V.A.; Baig, M.S.; Bezsonov, encodes for a substantial part of mitochondrial proteins and mitochondrial tRNA necessary for E.E.; Starodubova, A.V.; Popkova, T.V.; Orekhov, A.N. -

Mitochondrial Diseases in North America an Analysis of the NAMDC Registry
ARTICLE OPEN ACCESS Mitochondrial diseases in North America An analysis of the NAMDC Registry Emanuele Barca, MD, PhD, Yuelin Long, MS, Victoria Cooley, MS, Robert Schoenaker, MD, BS, Correspondence Valentina Emmanuele, MD, PhD, Salvatore DiMauro, MD, Bruce H. Cohen, MD, Amel Karaa, MD, Dr. Hirano [email protected] Georgirene D. Vladutiu, PhD, Richard Haas, MBBChir, Johan L.K. Van Hove, MD, PhD, Fernando Scaglia, MD, Sumit Parikh, MD, Jirair K. Bedoyan, MD, PhD, Susanne D. DeBrosse, MD, Ralitza H. Gavrilova, MD, Russell P. Saneto, DO, PhD, Gregory M. Enns, MBChB, Peter W. Stacpoole, MD, PhD, Jaya Ganesh, MD, Austin Larson, MD, Zarazuela Zolkipli-Cunningham, MD, Marni J. Falk, MD, Amy C. Goldstein, MD, Mark Tarnopolsky, MD, PhD, Andrea Gropman, MD, Kathryn Camp, MS, RD, Danuta Krotoski, PhD, Kristin Engelstad, MS, Xiomara Q. Rosales, MD, Joshua Kriger, MS, Johnston Grier, MS, Richard Buchsbaum, John L.P. Thompson, PhD, and Michio Hirano, MD Neurol Genet 2020;6:e402. doi:10.1212/NXG.0000000000000402 Abstract Objective To describe clinical, biochemical, and genetic features of participants with mitochondrial diseases (MtDs) enrolled in the North American Mitochondrial Disease Consortium (NAMDC) Registry. Methods This cross-sectional, multicenter, retrospective database analysis evaluates the phenotypic and molecular characteristics of participants enrolled in the NAMDC Registry from September 2011 to December 2018. The NAMDC is a network of 17 centers with expertise in MtDs and includes both adult and pediatric specialists. Results One thousand four hundred ten of 1,553 participants had sufficient clinical data for analysis. For this study, we included only participants with molecular genetic diagnoses (n = 666). -

Maternally Inherited Diabetes and Deafness Presenting with Ptosis and Macular Pattern Dystrophy Olufunmilola Ogun, Claire Sheldon and Jason J.S
RESIDENT & FELLOW SECTION Pearls & Oy-sters: Section Editor Maternally inherited diabetes and deafness Mitchell S.V. Elkind, MD, MS presenting with ptosis and macular pattern dystrophy Olufunmilola Ogun, PEARLS She had had hearing loss since her early 20s. An op- MBBS, MSc • Ptosis can occur with a variety of mitochondrial tometrist had noted asymptomatic retinal lesions Claire Sheldon, MD, syndromes, not just chronic progressive exter- about 10 years prior, without progression on subse- PhD, FRCSC nal ophthalmoplegia. quent visits; a retina specialist considered a diagnosis Jason J.S. Barton, MD, • Macular pattern dystrophy is highly character- of early age-related macular degeneration. She did PhD, FRCPC istic of maternally inherited diabetes and deaf- not have cardiac disease or diabetes. Her mother and ness (MIDD), and funduscopy should be a younger brother had early-onset deafness and the performed on all subjects with personal or fam- brother had diabetes. Correspondence & reprint Her visual acuity was 20/20 in both eyes; color requests to Dr. Barton: ily history of diabetes and deafness. [email protected] vision and peripheral visual fields were normal. Fun- OY-STER duscopy showed an unusual macular dystrophy, with a perimacular ring of retinal atrophy in both eyes. • Only 15% of patients with MIDD have diabe- She had a mild ptosis in the right eye with poor lid tes at diagnosis, and diabetes may start at ages closure of both eyes. Eye movements were normal. ranging from the teens to the fifth decade. Audiology confirmed moderate sensorineural hear- Mitochondrial disorders can cause an array of neuro- ing loss. The rest of her neurologic examination was ophthalmologic manifestations such as ptosis, external normal. -

Frequency and Clinical Features of Patients with Sensorineural Hearing Loss Associated with the A3243G Mutation of the Mitochondrial DNA in Otorhinolaryngic Clinics
J Hum Genet (2001) 46:595–599 © Jpn Soc Hum Genet and Springer-Verlag 2001 ORIGINAL ARTICLE Hiroshi Nagata · Keiichiro Kumahara · Takuya Tomemori Yukiko Arimoto · Kyoko Isoyama · Koh Yoshida Akiyoshi Konno Frequency and clinical features of patients with sensorineural hearing loss associated with the A3243G mutation of the mitochondrial DNA in otorhinolaryngic clinics Received: June 1, 2001 / Accepted: July 16, 2001 Abstract The A3243G mutation of the mitochondrial gene well as in individuals is believed to explain the diversity is a cause of maternally inherited diabetes and deafness. of clinical manifestations associated with identical mtDNA The aim of this study was to evaluate the frequency and mutations. One such mutation potentially associated with clinical features of this mutation in patients with senso- various clinical syndromes is the A to G point mutation at rineural hearing loss (SNHL) in otorhinolaryngic clinics. nucleotide position 3243 (A3243G) in the mitochondrial The frequency of the A3243G mutation in 230 patients with tRNALeu(UUR) gene. This mutation was first identified in SNHL was 1.74% (4/230). Three of the four patients had patients with MELAS (mitochondrial myopathy, encepha- diabetes mellitus (DM) and were already aware that they lopathy, lactic acidosis, and stroke-like episodes) syndrome had the mutation. The other had cardiomyopathy but not (Goto et al. 1990). Subsequent work showed that the iden- DM, and proved to have the mutation in this study. The tical mutation is also causative for maternally inherited frequency of the mutation was 12.9% (4/31) in patients with diabetes associated with deafness (Kadowaki et al. 1994; a family history of possible maternal inheritance of SNHL, van den Ouweland et al. -

Diabetes and Deafness; Not All MODY Is MELAS
Diabetes Care In Press, published online May 31, 2007 Diabetes and deafness; is it sufficient to screen for the mitochondrial 3243A>G mutation alone? Received for publication 8 March 2007 and accepted in revised form 26 May 2007. Running title: Diagnostic strategies in diabetes and deafness. Roger G Whittaker MRCP1*, Andrew M Schaefer MRCP1, Robert McFarland MRCP1, Robert W Taylor MRCPath1, Mark Walker FRCP2, Douglass M Turnbull FRCP1. 1Mitochondrial Research Group, School of Neurology, Neurobiology and Psychiatry, Newcastle University, Newcastle upon Tyne, NE2 4HH, UK. 2Diabetes Research Group, School of Clinical Medical Sciences, Newcastle University, Newcastle upon Tyne, NE2 4HH, UK. *Corresponding author; [email protected] Copyright American Diabetes Association, Inc., 2007 The m.3243A>G mitochondrial DNA mutation in either whole blood or mutation is well known to be urinary epithelial cells (8) . We associated with deafness and wanted to assess whether this is a diabetes, and patients presenting sensible investigation strategy in with these clinical features are patients presenting in this way. routinely screened for this mutation. Firstly, we wanted to assess how We wanted to assess whether this is many patients with other mutations a suitable screening strategy. We of the mitochondrial genome present retrospectively reviewed the clinical with the combination of diabetes and notes of 242 patients who had deafness, who would potentially be attended a specialist mitochondrial missed in this screening strategy. clinic in the preceding twenty five Secondly, we wanted to see whether year period. Out of the total of 29 other clinical features of patients with mitochondrial disease mitochondrial disease were present presenting with deafness and in these patients which might have diabetes, only 21 would have been provided additional clues as to the correctly diagnosed by screening for correct diagnosis (9). -

Overview on Visceral Manifestations of Mitochondrial Disorders
r E v i E w overview on visceral manifestations of mitochondrial disorders J. Finsterer Neurological Department, Krankenanstalt Rudolfstiftung, Vienna, Austria, tel.: +43 (0)1-71165-92085, fax: +43 (0)1-478 17 11, e-mail: [email protected] A b s T r act Mitochondriopathies (MCPs) that reach adult age not Since MCPs may cause any symptom, in any organ, at any only manifest in the central and peripheral nervous age, the clinical presentation is quite heterogeneous. In systems, eyes, ears, and dermis, but also in visceral rare cases only a single organ is affected, but multisystem organs, such as endocrine organs, heart, liver, guts, involvement may develop with progression of the disease. kidneys and blood. visceral manifestations occur as part Possible manifestations of visceral organs are summarised of a multisystem involvement or rarely as single organ in table 1. Various combinations of organ involvement led to affection. Endocrinological abnormalities are found the definition of mitochondrial syndromes, of which some in the MElAs, MERRF, KSS, MIDD and DIDMoAd are well known for their acronyms. The majority of MCPs, syndromes. Cardiac involvement occurs in the MElAs, however, do not fit into one of these disease categories. MERRF, KSS, CPEo, LHON, NArP, and leigh syndromes. Mitochondrial syndromes with visceral manifestations are gastrointestinal manifestations are common in the listed in tables 2 and 3. MERRF, MNGIE, DIDMoAd, and leigh syndromes. Mitochondrial syndromes with renal manifestations are the KSS, Pearson, DIDMoAd, and leigh syndromes. The A et i o l o g y haematopoetic system is affected in the KSS, MERRF, and leigh syndromes. -

The Effects of Coenzyme Q10 Treatment on Maternally Inherited Diabetes Mellitus and Deafness, and Mitochondrial DNA 3243 (A to G) Mutation
Diabetologia (1998) 41: 584±588 Ó Springer-Verlag 1998 The effects of coenzyme Q10 treatment on maternally inherited diabetes mellitus and deafness, and mitochondrial DNA 3243 (A to G) mutation S. Suzuki, Y. Hinokio, M. Ohtomo, M. Hirai, A. Hirai, M. Chiba, S. Kasuga, Y. Satoh, H. Akai, T. Toyota Third Department of Internal Medicine, Tohoku University School of Medicine, Seiryou-machi, Aoba-ku, Sendai, Japan Summary The characteristic clinical features of dia- DM), 5 mutant IGT and 5 mutant NGT subjects in betes mellitus with mitochondrial DNA (mtDNA) yearly examinations. The insulin secretory response 3243(A-G) mutation are progressive insulin secretory assessed by glucagon-induced C-peptide secretion defect, neurosensory deafness and maternal inheri- and 24 h urinary C-peptide excretion after 3 years in tance, referred to as maternally inherited diabetes the CoQ10-DM group was significantly higher than mellitus and deafness (MIDD). A treatment for that in the control-DM group. CoQ10 therapy pre- MIDD to improve insulin secretory defects and re- vented progressive hearing loss and improved blood duce deafness has not been established. The effects lactate after exercise in the MIDD patients. CoQ10 of coenzyme Q10 (CoQ10) treatment on insulin secre- treatment did not affect the diabetic complications tory response, hearing capacity and clinical symp- or other clinical symptoms of MIDD patients. CoQ10 toms of MIDD were investigated. 28 MIDD patients treatment did not affect the insulin secretory capacity (CoQ10-DM), 7 mutant subjects with impaired glu- of the mutant IGT and NGT subjects. There were no cose tolerance (IGT), and 15 mutant subjects with side effects during therapy. -
Molecular Bases of Hearing Loss in Multi-Systemic Mitochondrial
October 2006 ⅐ Vol. 8 ⅐ No. 10 article Molecular bases of hearing loss in multi-systemic mitochondrial cytopathy Fernando Scaglia, MD1,2, Chang-Hung Hsu, MD3, Haeyoung Kwon, PhD4, Ren-Kui Bai, MD, PhD1, Cherng-Lih Perng, MD3, Hua-Mei Chang, PhD5,PuDai,MD6, E. O’Brian Smith, PhD7, David A. H. Whiteman, MD8, Annette Feigenbaum, MD9, Andrea Gropman, MD10, and Lee-Jun C. Wong, PhD1 Purpose: Hearing loss is a common clinical feature in classic mitochondrial syndromes. The purpose of this study was to evaluate the diverse molecular etiologies and natural history of hearing loss in multi-systemic mitochondrial cytopathies and the possible correlation between degree of hearing loss and neurological phenotype. Methods: In this retrospective study we evaluated the clinical features and molecular bases of hearing loss associated with multi-systemic mitochondrial cytopathy. Forty-five patients with sensorineural hearing loss and definite diagnosis of mitochondrial cytopathy according to the published diagnostic criteria were studied. Results: The sensorineural hearing loss was progressive and for the most part symmetrical with involvement of the higher frequencies. Both cochlear and retrocochlear involvement were found in this cohort. No correlation was found between the degree of hearing loss and the number and severity of neurological manifestations. Deleterious mtDNA point mutations of undisputed pathogenicity were identified in 18 patients. The A3243G mutation was the most frequently encoun- tered among this group. MtDNA depletion, over-replication, and multiple deletions were found in further 11 cases. Conclusion: This study reveals an expanding spectrum of mtDNA abnormalities associated with hearing loss. No correlation was found between the degrees of hearing loss and the severity of neurological manifestations. -
Identification of Novel Mutations of the WFS1 Gene in Brazilian Patients with Wolfram Syndrome
European Journal of Endocrinology (2009) 160 309–316 ISSN 0804-4643 CLINICAL STUDY Identification of novel mutations of the WFS1 gene in Brazilian patients with Wolfram syndrome Maria Regina R Gasparin, Felipe Crispim, Sı´lvia L Paula1, Maria Beatriz S Freire2, Ivaldir S Dalbosco3, Thais Della Manna4, Joa˜o Eduardo N Salles5,Fa´bio Gasparin6, Ale´xis Guedes, Joa˜o M Marcantonio7, Ma´rcio Gambini8, Camila P Salim and Regina S Moise´s Division of Endocrinology, Federal University of Sa˜o Paulo, Sa˜o Paulo, Brazil, 1Federal University of Goia´s, Goiaˆnia, Brazil, 2Medical School of Jundiaı´, Jundiaı´, Brazil, 3University Foundation of Rio Grande, Rio Grande, Brazil, 4Pediatric Endocrinology Unit, University of Sa˜o Paulo, Sa˜o Paulo, Brazil, 5Medical School of Santa Casa de Sa˜o Paulo, Sa˜o Paulo, Brazil, 6Department of Ophthalmology, University of Sa˜o Paulo, Sa˜o Paulo, Brazil, 7Maringa´, PR, Brazil and 8Jundiaı´, SP, Brazil (Correspondence should be addressed to R S Moise´s; Email: [email protected]) Abstract Objective: Wolfram syndrome (WS) is a rare, progressive, neurodegenerative disorder with an autosomal recessive pattern of inheritance. The gene for WS, WFS1, was identified on chromosome 4p16 and most WS patients carry mutations in this gene. However, some studies have provided evidence for genetic heterogeneity and the genotype–phenotype relationships are not clear. Our aim was to ascertain the spectrum of WFS1 mutations in Brazilian patients with WS and to examine the phenotype–genotype relationships in these patients. Design and methods: Clinical characterization and analyses of the WFS1 gene were performed in 27 Brazilian patients with WS from 19 families.