Overview on Visceral Manifestations of Mitochondrial Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mitochondrial Trnaleu(Uur) May Cause an MERRF Syndrome
J7ournal ofNeurology, Neurosurgery, and Psychiatry 1996;61:47-51 47 The A to G transition at nt 3243 of the J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.61.1.47 on 1 July 1996. Downloaded from mitochondrial tRNALeu(uuR) may cause an MERRF syndrome Gian Maria Fabrizi, Elena Cardaioli, Gaetano Salvatore Grieco, Tiziana Cavallaro, Alessandro Malandrini, Letizia Manneschi, Maria Teresa Dotti, Antonio Federico, Giancarlo Guazzi Abstract Two distinct maternally inherited encephalo- Objective-To verify the phenotype to myopathies with ragged red fibres have been genotype correlations of mitochondrial recognised on clinical grounds: MERRF, DNA (mtDNA) related disorders in an which is characterised by myoclonic epilepsy, atypical maternally inherited encephalo- skeletal myopathy, neural deafness, and optic myopathy. atrophy,' and MELAS, which is defined by Methods-Neuroradiological, morpholog- stroke-like episodes in young age, episodic ical, biochemical, and molecular genetic headache and vomiting, seizures, dementia, analyses were performed on the affected lactic acidosis, skeletal myopathy, and short members of a pedigree harbouring the stature.2 Molecular genetic studies later con- heteroplasmic A to G transition at firmed the nosological distinction between the nucleotide 3243 of the mitochondrial two disorders, showing that MERRF is strictly tRNAI-u(UR), which is usually associated associated with two mutations of the mito- with the syndrome of mitochondrial chondrial tRNALYs at nucleotides 83443 and encephalomyopathy, lactic -

Progressive Myoclonic Epilepsy
www.neurologyindia.com Indian Perspective Progressive myoclonic epilepsy P. Satishchandra, S. Sinha Department of Neurology, National Institute of Mental Health & Neurosciences, Bangalore, India Abstract Progressive myoclonic epilepsy (PME) is a disease complex and is characterized by the development of relentlessly progressive myoclonus, cognitive impairment, ataxia, and other neurologic deficits. It encompasses different diagnostic entities and the common causes include Lafora body disease, neuronal ceroid lipofuscinoses, Unverricht–Lundborg disease, myoclonic epilepsy with ragged-red fiber (MERRF) syndrome, sialidoses, dentato-rubro-pallidal atrophy, storage diseases, and some of the inborn errors of metabolism, among others. Recent advances in this area have clarified molecular genetic basis, biological basis, and natural history, and also provided Address for correspondence: a rational approach to the diagnosis. Most of the large studies related to PME are from Dr. P. Satishchandra, south India from a single center, National Institute of Mental Health and Neurological National Institute of Mental Health Sciences (NIMHANS), Bangalore. However, there are a few case reports and small series & Neurosciences (NIMHANS), Hosur Road, Bangalore - 560 029, about Lafora body disease, neuronal ceroid lipofuscinoses and MERRF from India. We India. review the clinical and research experience of a cohort of PME patients evaluated at E-mail: drpsatishchandra@yahoo. NIMHANS over the last two decades, especially the phenotypic, electrophysiologic, -

Family Phenotypic Heterogeneity Caused by Mitochondrial DNA Mutation A3243G Heterogeneidade Fenotípica De Uma Família Causada
Alves D, et al. Phenotypic heterogeneity of inherited diabetes and deafness, Acta Med Port 2017 Jul-Aug;30(7-8):581-585 REFERENCES 1. Bywaters EG. Still’s disease in the adult. Ann Rheum Dis. 1971;30:121– with emphasis on organ failure. Semin Arthritis Rheum. 1987;17:39–57. 33. 9. Ohta A, Yamaguchi M, Tsunematsu T, Kasukawa R, Mizushima H, 2. Efthimiou P, Paik PK, Bielory L. Diagnosis and management of adult Kashiwagi H, et al. Adult Still’s disease: a multicenter survey of Japanese onset Still’s disease. Ann Rheum Dis. 2006;65:564–72. patients. J Rheumatol. 1990;17:1058–63. 3. Cheema GS, Quismorio FP. Pulmonary involvement in adult-onset Still’s 10. Cagatay Y, Gul A, Cagatay A, Kamali S, Karadeniz A, Inanc M, et al. disease. Curr Opin Pulm Med. 1999;5:305–9. Adult-onset Still’s disease. Int J Clin Pract. 2009;63:1050–5. 4. Zeng T, Zou YQ, Wu MF, Yang CD. Clinical features and prognosis 11. Riera E, Olivé A, Narváez J, Holgado S, Santo P, Mateo L, et al. CASO CLÍNICO of adult-onset still’s disease: 61 cases from China. J Rheumatol. Adult onset Still’s disease: review of 41 cases. Clin Exp Rheumatol. 2009;36:1026–31. 2011;29:331–6. 5. Yamaguchi M, Ohta A, Tsunematsu T, Kasukawa R, Mizushima Y, 12. Chen PD, Yu SL, Chen S, Weng XH. Retrospective study of 61 patients Kashiwagi H, et al. Preliminary criteria for classification of adult Still’s with adult-onset Still’s disease admitted with fever of unknown origin in disease. -

Identification of P.A684V Missense Mutation in the WFS1 Gene As a Frequent Cause of Autosomal Dominant Optic Atrophy and Hearing
RESEARCH ARTICLE Identification of p.A684V Missense Mutation in the WFS1 Gene as a Frequent Cause of Autosomal Dominant Optic Atrophy and Hearing Impairment Nanna D. Rendtorff,1 Marianne Lodahl,1 Houda Boulahbel,2 Ida R. Johansen,1 Arti Pandya,3 Katherine O. Welch,4 Virginia W. Norris,4 Kathleen S. Arnos,4 Maria Bitner-Glindzicz,5 Sarah B. Emery,6 Marilyn B. Mets,7 Toril Fagerheim,8 Kristina Eriksson,9 Lars Hansen,1 Helene Bruhn,10 Claes M€oller,11 Sture Lindholm,12 Stefan Ensgaard,13 Marci M. Lesperance,6 and Lisbeth Tranebjaerg1,14*,† 1Wilhelm Johannsen Centre for Functional Genome Research, Department of Cellular and Molecular Medicine (ICMM), The Panum Institute, University of Copenhagen, Copenhagen, Denmark 2Biotech Research & Innovation Centre (BRIC), University of Copenhagen, Copenhagen, Denmark 3Department of Human and Molecular Genetics, Virginia Commonwealth University, Richmond, Virginia 4Department of Biology, Gallaudet University, Washington DC 5UCL Institute of Child Health, London, UK 6Division of Pediatric Otolaryngology, Department of Otolaryngology-Head and Neck Surgery, UniversityofMichiganHealthSystem,AnnArbor,Michigan 7Departments of Ophthalmology and Surgery, Feinberg School of Medicine, Northwestern University, Evanston, Illinois 8Division of Child and Adolescent Health, Department of Medical Genetics, University Hospital of North Norway, Tromsø, Norway 9Department of Ophthalmology, Lundby Hospital, Gothenburg, Sweden 10Division of Metabolic Diseases, Department of Laboratory Medicine, Karolinska Institute, Karolinska University Hospital, Stockholm, Sweden 11Department of Audiology/Disability Research (SIDR), O¨rebro University, Sweden 12Department of Audiology, County Hospital, Kalmar, Sweden 13Department of Psychiatrics, Stockholm, Sweden 14Department of Audiology, Bispebjerg Hospital, Copenhagen, Denmark Received 19 July 2010; Accepted 2 February 2011 Optic atrophy (OA) and sensorineural hearing loss (SNHL) are these additional eight families. -

Dominant Optic Atrophy
Lenaers et al. Orphanet Journal of Rare Diseases 2012, 7:46 http://www.ojrd.com/content/7/1/46 REVIEW Open Access Dominant optic atrophy Guy Lenaers1*, Christian Hamel1,2, Cécile Delettre1, Patrizia Amati-Bonneau3,4,5, Vincent Procaccio3,4,5, Dominique Bonneau3,4,5, Pascal Reynier3,4,5 and Dan Milea3,4,5,6 Abstract Definition of the disease: Dominant Optic Atrophy (DOA) is a neuro-ophthalmic condition characterized by a bilateral degeneration of the optic nerves, causing insidious visual loss, typically starting during the first decade of life. The disease affects primary the retinal ganglion cells (RGC) and their axons forming the optic nerve, which transfer the visual information from the photoreceptors to the lateral geniculus in the brain. Epidemiology: The prevalence of the disease varies from 1/10000 in Denmark due to a founder effect, to 1/30000 in the rest of the world. Clinical description: DOA patients usually suffer of moderate visual loss, associated with central or paracentral visual field deficits and color vision defects. The severity of the disease is highly variable, the visual acuity ranging from normal to legal blindness. The ophthalmic examination discloses on fundoscopy isolated optic disc pallor or atrophy, related to the RGC death. About 20% of DOA patients harbour extraocular multi-systemic features, including neurosensory hearing loss, or less commonly chronic progressive external ophthalmoplegia, myopathy, peripheral neuropathy, multiple sclerosis-like illness, spastic paraplegia or cataracts. Aetiology: Two genes (OPA1, OPA3) encoding inner mitochondrial membrane proteins and three loci (OPA4, OPA5, OPA8) are currently known for DOA. Additional loci and genes (OPA2, OPA6 and OPA7) are responsible for X-linked or recessive optic atrophy. -

TIMM8A Gene Translocase of Inner Mitochondrial Membrane 8A
TIMM8A gene translocase of inner mitochondrial membrane 8A Normal Function The TIMM8A gene provides instructions for making a protein that is found inside mitochondria, which are structures within cells that convert the energy from food into a form that cells can use. Mitochondria have two membranes, an outer membrane and an inner membrane, which are separated by a fluid-filled area called the intermembrane space. The TIMM8A protein is found in the intermembrane space, where it forms a complex (a group of proteins that work together) with a very similar protein called TIMM13. This complex transports other proteins across the intermembrane space to the mitochondrial inner membrane. Health Conditions Related to Genetic Changes Deafness-dystonia-optic neuronopathy syndrome At least 20 mutations in the TIMM8A gene have been found to cause deafness-dystonia- optic neuronopathy (DDON) syndrome. Most of these mutations result in the absence of functional TIMM8A protein inside the mitochondria, which prevents the formation of the TIMM8A/TIMM13 complex. Researchers believe that the lack of this complex leads to abnormal transport of proteins across the intermembrane space, although it is unclear how abnormal protein transport affects the function of the mitochondria and causes the signs and symptoms of DDON syndrome. Some people with DDON syndrome have large DNA deletions that remove the entire TIMM8A gene and one end of a neighboring gene known as BTK. Mutations in the BTK gene cause X-linked agammaglobulinemia (XLA), which is characterized by an increased susceptibility to infections. Individuals with large DNA deletions that include the TIMM8A gene and the BTK gene have the signs and symptoms of both DDON syndrome and XLA. -

Mitochondrial Carriers Regulating Insulin Secretion Profiled in Human Islets Upon Metabolic Stress
Jiménez-Sánchez et al. Supplementary files Mitochondrial carriers regulating insulin secretion profiled in human islets upon metabolic stress Supplementary Table S1: Clinical Data of the human donors of pancreatic islets, type of analyses performed and tested conditions. Supplementary Table S2: Quantitative data related to the transcriptomic profiles of mitochondrial solute carriers and associated genes in human islets upon metabolic stress. NA: Not applicable, ND: not detected. Supplementary Table S3: Quantitative data related to the transcriptomic profiles of the electron transport chain machinery and related mitochondrial carriers in human islets upon metabolic stress.NA: Not applicable, ND: not detected. Supplementary Table S4: Quantitative data related to the transcriptomic profiles of the outer and inner mitochondrial membrane translocases TOM/TIM machinery in human islets upon metabolic stress.NA: Not applicable, ND: not detected. Supplementary Table S5: Quantitative data related to the transcriptomic profiles of mitochondrial iron transport genes in human islets under metabolic stress. NA: Not applicable, ND: not detected. Supplementary Table S6: Quantitative data related to the transcriptomic profiles of mitochondrial calcium transport genes in human islets upon metabolic stress. NA: Not applicable, ND: not detected. Supplementary Table S7: Primers used for quantitative RT-PCR analysis Supplementary Figure S1: Functional interaction network of human (a) mitochondrial calcium transport genes; (b) outer and inner mitochondrial membrane translocases TOM/TIM machinery; (c) electron transport chain machinery and related carriers; (d) mitochondrial iron transport genes. Nodes were connected using the STRING interaction knowledgebase with a confidence score >0.4. Supplementary Figure S2: Effects of high 25 mM glucose (G25) and 0.4 mM oleate (Olea) or palmitate (Palm) on the transcriptional regulation of the electron transport chain machinery. -

Deafness-Dystonia-Optic Neuronopathy Syndrome
Deafness-dystonia-optic neuronopathy syndrome Description Deafness-dystonia-optic neuronopathy (DDON) syndrome, also known as Mohr- Tranebjærg syndrome, is characterized by hearing loss that begins early in life, problems with movement, impaired vision, and behavior problems. This condition occurs almost exclusively in males. The first symptom of DDON syndrome is hearing loss caused by nerve damage in the inner ear (sensorineural hearing loss), which begins in early childhood. The hearing impairment worsens over time, and most affected individuals have profound hearing loss by age 10. People with DDON syndrome typically begin to develop problems with movement during their teens, although the onset of these symptoms varies among affected individuals. Some people experience involuntary tensing of the muscles (dystonia), while others have difficulty coordinating movements (ataxia). The problems with movement usually worsen over time. Individuals with DDON syndrome have normal vision during childhood, but they may develop vision problems due to breakdown of the nerves that carry information from the eyes to the brain (optic atrophy). Affected individuals can develop an increased sensitivity to light (photophobia) or other vision problems beginning in adolescence. Their sharpness of vision (visual acuity) slowly worsens, often leading to legal blindness in mid-adulthood. People with this condition may also have behavior problems, including changes in personality and aggressive or paranoid behaviors. They also usually develop a gradual decline in thinking and reasoning abilities (dementia) in their forties. The lifespan of individuals with DDON syndrome depends on the severity of the disorder. People with severe cases have survived into their teenage years, while those with milder cases have lived into their sixties. -

Polyphagia Ellen N
W0117-Section I (31-50).qxd 4/23/04 7:26 PM Page 124 CHAPTER • 34 Polyphagia Ellen N. Behrend olyphagia is the consumption of food in excess of and liver disease) lead to polyphagia by unknown mecha- normal caloric intake. Hunger and satiety and, conse- nisms. Secondary polyphagia can also be caused by certain P quently, feeding behavior are primarily controlled by drugs. certain regions in the central nervous system (CNS), but many factors affect the function of these areas. Thus polypha- gia can be classified as primary (i.e., a CNS abnormality) or HISTORY secondary (i.e., a systemic problem affecting the CNS). Secondary polyphagia is by far more common and usually is Any change in body weight is an important differentiating accompanied by clinical signs of the underlying disease. feature of the various causes of polyphagia (Figure 34-1). Determining whether weight gain or loss has occurred should Primary or drug-induced polyphagia typically results in weight be the first step in formulating a list of differential diagnoses gain, because nutrients are adequate and feeding is inappro- and a diagnostic plan. priately increased. Pathologic secondary polyphagia is more commonly associated with weight loss, because the nutrient supply usually does not meet physiologic demands. However, PHYSIOLOGY some causes, such as acromegaly, hypoglycemia caused by an insulinoma, sudden acquired retinal degeneration syndrome Food intake is controlled by a variety of factors, including gas- (SARDS), and hyperadrenocorticism (HAC), lead to weight trointestinal, environmental, and CNS phenomena. The CNS, gain. Physiologic polyphagia can result in weight gain (e.g., mainly the hypothalamus, controls eating behavior.The lateral pregnancy, growth) or maintenance of weight (e.g., lactation, hypothalamic nuclei represent the “feeding center”; their cold environment, increased exercise). -

Sudden Death in Eating Disorders
Vascular Health and Risk Management Dovepress open access to scientific and medical research Open Access Full Text Article REVIEW Sudden death in eating disorders Beatriz Jáuregui-Garrido1 Abstract: Eating disorders are usually associated with an increased risk of premature death Ignacio Jáuregui-Lobera2,3 with a wide range of rates and causes of mortality. “Sudden death” has been defined as the abrupt and unexpected occurrence of fatality for which no satisfactory explanation of the 1Department of Cardiology, University Hospital Virgen del Rocío, 2Behavioral cause can be ascertained. In many cases of sudden death, autopsies do not clarify the main Sciences Institute, 3Pablo de Olavide cause. Cardiovascular complications are usually involved in these deaths. The purpose of University, Seville, Spain this review was to report an update of the existing literature data on the main findings with respect to sudden death in eating disorders by means of a search conducted in PubMed. The most relevant conclusion of this review seems to be that the main causes of sudden death in eating disorders are those related to cardiovascular complications. The predictive value of the For personal use only. increased QT interval dispersion as a marker of sudden acute ventricular arrhythmia and death has been demonstrated. Eating disorder patients with severe cardiovascular symptoms should be hospitalized. In general, with respect to sudden death in eating disorders, some findings (eg, long-term eating disorders, chronic hypokalemia, chronically low plasma albumin, and QT intervals .600 milliseconds) must be taken into account, and it must be highlighted that during refeeding, the adverse effects of hypophosphatemia include cardiac failure. -
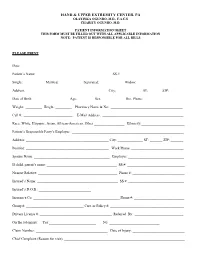
Patient Information Sheet This Form Must Be Filled out with All Applicable Information Note: Patient Is Responsible for All Bills
HAND & UPPER EXTREMITY CENTER, PA OLAYINKA OGUNRO, M.D., F.A.C.S CHARITY OGUNRO, M.D. PATIENT INFORMATION SHEET THIS FORM MUST BE FILLED OUT WITH ALL APPLICABLE INFORMATION NOTE: PATIENT IS RESPONSIBLE FOR ALL BILLS PLEASE PRINT Date: ________________________________________ Patient’s Name: _________________________________________ SS #: __________________________________ Single: __________ Married: ___________ Separated: ___________ Widow: ____________ Address: _____________________________________________ City: _____________ ST: ______ ZIP:________ Date of Birth: ___________________ Age:_________ Sex: ____________ Hm. Phone: ______________________ Weight: _________ Height: _________ Pharmacy Name & No: ________________________________________ Cell #: ___________________________ E-Mail Address: _____________________________________________ Race: White, Hispanic, Asian, African-American, Other _________________ Ethnicity:________________________ Patient’s Responsible Party’s Employer: ______________________________________________________________ Address: ______________________________________________ City: ______________ ST: _______ ZIP: _______ Position: ______________________________________________ Work Phone: _____________________________ Spouse Name: __________________________________________ Employer: _______________________________ If child, parent’s name: _______________________________________ SS #: ________________________________ Nearest Relative: ____________________________________________ Phone #: _____________________________ -

Myoclonus Epilepsy Associated with Ragged-Red Fibers
DOI: 10.1590/0004-282X20140124 VIEWS AND REVIEWS When should MERRF (myoclonus epilepsy associated with ragged-red fibers) be the diagnosis? Quando o diagnóstico deveria ser MERRF (epilepsia mioclônica associada com fibras vermelhas rasgadas)? Paulo José Lorenzoni, Rosana Herminia Scola, Cláudia Suemi Kamoi Kay, Carlos Eduardo S. Silvado, Lineu Cesar Werneck ABSTRACT Myoclonic epilepsy associated with ragged red fibers (MERRF) is a rare mitochondrial disorder. Diagnostic criteria for MERRF include typical manifestations of the disease: myoclonus, generalized epilepsy, cerebellar ataxia and ragged red fibers (RRF) on muscle biopsy. Clinical features of MERRF are not necessarily uniform in the early stages of the disease, and correlations between clinical manifestations and physiopathology have not been fully elucidated. It is estimated that point mutations in the tRNALys gene of the DNAmt, mainly A8344G, are responsible for almost 90% of MERRF cases. Morphological changes seen upon muscle biopsy in MERRF include a substantive proportion of RRF, muscle fibers showing a deficient activity of cytochrome c oxidase (COX) and the presence of vessels with a strong reaction for succinate dehydrogenase and COX deficiency. In this review, we discuss mainly clinical and laboratory manifestations, brain images, electrophysiological patterns, histology and molecular findings as well as some differential diagnoses and treatments. Keywords: MERRF, mitochondrial, epilepsy, myoclonus, myopathy. RESUMO Epilepsia mioclônica associada com fibras vermelhas rasgadas (MERRF) é uma rara doença mitocondrial. O critério diagnóstico para MERRF inclui as manifestações típicas da doença: mioclonia, epilepsia generalizada, ataxia cerebelar e fibras vermelhas rasgadas (RRF) na biópsia de músculo. Na fase inicial da doença, as manifestações clínicas podem não ser uniformes, e correlação entre as manifestações clínicas e fisiopatologia não estão completamente elucidadas.