Moderate to Severe Cases of Green Pit Viper Bites In
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Zootaxa,Revision of the Tropidolaemus
Zootaxa 1644: 1–40 (2007) ISSN 1175-5326 (print edition) www.mapress.com/zootaxa/ ZOOTAXA Copyright © 2007 · Magnolia Press ISSN 1175-5334 (online edition) Revision of the Tropidolaemus wagleri-complex (Serpentes: Viperidae: Crotali- nae). I. Definition of included taxa and redescription of Tropidolaemus wagleri (Boie, 1827) GERNOT VOGEL1, PATRICK DAVID2, MARIO LUTZ3, JOHAN VAN ROOIJEN4 & NICOLAS VIDAL5 1 Society for Southeast Asian Herpetology, Im Sand 3, D-69115 Heidelberg, Germany E-mail: [email protected] 2 Département Systématique et Evolution, USM 602 Taxonomie-collection – Reptiles & Amphibiens, Case postale 30, Muséum National d’Histoire Naturelle, 25 rue Cuvier, F-75231 Paris Cedex 05, France, E-mail: [email protected] 3 Zoological Institute of HerpaWorld inc., Paradise Reptile Zoo, 5203 Puerto Galera, Oriental Mindoro, Philippines E-mail: [email protected] 4 Da Costastraat 99, 2321 AM Leiden, The Netherlands E-mail: [email protected] 5 Département Systématique et Evolution, UMR 7138, Systématique, Evolution, Adaptation, Case Postale 26, Muséum National d’His- toire Naturelle, 57 rue Cuvier, F-75231 Paris Cedex 05, France E-mail: [email protected] TABLE OF CONTENTS ABSTRACT…………………………………………………………………………………………….................... .........1 INTRODUCTION…………………………………………………………………………………………….................... 2 MATERIAL AND METHODS……………………………………………………………………………….................... 3 HISTORICAL ANALYSIS…………………………………………………………………………………….................. 6 TAXONOMIC RESULTS................. …………………………………………………………………………………….12 -

Biology and Conser V a Tion of Tropical Asian Amphibians
BIOLOGY AND CONSERVATION OF TROPICAL ASIAN AMPHIBIANS BIOLOGY AND CONSERVATION OF TROPICAL ASIAN AMPHIBIANS PROCEEDINGS OF THE CONFERENCE “BIOLOGY OF THE AMPHIBIANS IN THE SUNDA REGION, SOUTH-EAST ASIA” Organized by The Institute of Biodiversity and Environmental Conservation Universiti Malaysia Sarawak, Kota Samarahan, Sarawak, Malaysia and Biozentrum Grindel und Zoologishches Museum University of Hamburg, Germany 28–30 September 2009 With support from Volkswagen Stiftung and Sarawak Shell Bhd. Edited by Indraneil Das, Alexander Haas and Andrew Alek Tuen 2011 In: Biology and Conservation of Tropical Asian Amphibians. Proceedings of the Conference “Biology of the Amphibians in the Sunda Region, South-east Asia”. Organized by Universiti Malaysia Sarawak, Kota Samarahan, Sarawak, Malaysia 28–30 September 2009. pp:1–7. Edited by Indraneil Das, Alexander Haas and Andrew Alek Tuen. 2011. Institute of Biodiversity and Environmental Conservation, Universiti Malaysia Sarawak, Kota Samarahan. HERPETOFAUNA DIVERSITY OF KARIMATA ISLAND, INDONESIA UMILAELA ARIFIN, DJOKO T. ISKANDAR and ROSITA ELIANUR School of Life Sciences and Technology-Institut Teknologi Bandung, Labtek XI Building, 10, Jalan Ganesa, Bandung, West Java, Indonesia 40132 (with four text-figures) ABSTRACT.– A study on the herpetological diversity of Karimata Island was conducted from 27 January–7 March 2008. Eight species of amphibians, dominated by the family Dicroglossidae (Limnonectes ingeri, L. malesianus, L. paramacrodon and Fejervarya cancrivora) and 18 species of reptiles, dominated by the family Gekkonidae (Cnemaspis kendallii, Cyrtodactylus sp. A, Cyrtodactylus sp. B, Gekko gecko, G. monarchus and Hemidactylus frenatus) were recorded. Due to an impoverished fauna, unusual distribution of certain species has been observed. A Philautus sp. occurs from lowland up to the peak of the highest mountain in this island. -

Commencement Ceremony May 7, 2016 Banners
COMMENCEMENT CEREMONY MAY 7, 2016 BANNERS NATIONAL ALUMNI COLLEGE OF ARTS ASSOCIATION AND SCIENCES ETSU National University Libraries College of Alumni Association Arts and Sciences CLAUDIUS G. CLEMMER COLLEGE OF CLINICAL COLLEGE OF AND REHABILITATIVE EDUCATION HEALTH SCIENCES College of Business Claudius G. Clemmer College of Honors College and Technology College of Education Clinical & Rehabilitative COLLEGE OF PUBLIC HEALTHHealth Sciences BILL GATTON COLLEGE OF PHARMACY College of College of Bill Gatton Nursing Public Health College of Pharmacy QUILLEN COLLEGE OF MEDICINE S CHOOL OF CONTINUING STUDIES AND ACADEMIC OUTREACH School of School of Graduate Studies James H. Quillen Continuing Studies College of Medicine and Academic Outreach Commencement Ceremony Spring 2016 Guests are asked to refrain from coming forward to take pictures during the ceremony. Stage decorations provided by Sean Morris, Assistant Director of Grounds and Landscaping, and Tisha Harrison, Director, University Advancement Flag Etiquette All persons present in uniform should render the military salute. Members of the armed forces and veterans who are present but not in uniform may render the military salute. All other persons present should face the flag and stand at attention with their right hand over the heart, or if applicable, remove their headdress with their right hand and hold it at the left shoulder, the hand being over the heart. When the national anthem is played or sung, citizens should stand at attention through the last note. 1 THE PLATFORM PARTY Dr. Brian Noland, President, East Tennessee State University Dr. Bert C. Bach, Provost and Vice President for Academic Affairs Dr. Wilsie S. Bishop, University Chief Operating Officer and Vice President for Health Affairs Dr. -
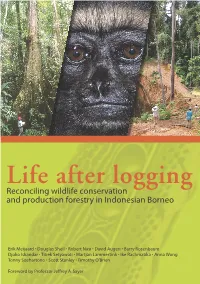
Life After Logging: Reconciling Wildlife Conservation and Production Forestry in Indonesian Borneo
Life after logging Reconciling wildlife conservation and production forestry in Indonesian Borneo Erik Meijaard • Douglas Sheil • Robert Nasi • David Augeri • Barry Rosenbaum Djoko Iskandar • Titiek Setyawati • Martjan Lammertink • Ike Rachmatika • Anna Wong Tonny Soehartono • Scott Stanley • Timothy O’Brien Foreword by Professor Jeffrey A. Sayer Life after logging: Reconciling wildlife conservation and production forestry in Indonesian Borneo Life after logging: Reconciling wildlife conservation and production forestry in Indonesian Borneo Erik Meijaard Douglas Sheil Robert Nasi David Augeri Barry Rosenbaum Djoko Iskandar Titiek Setyawati Martjan Lammertink Ike Rachmatika Anna Wong Tonny Soehartono Scott Stanley Timothy O’Brien With further contributions from Robert Inger, Muchamad Indrawan, Kuswata Kartawinata, Bas van Balen, Gabriella Fredriksson, Rona Dennis, Stephan Wulffraat, Will Duckworth and Tigga Kingston © 2005 by CIFOR and UNESCO All rights reserved. Published in 2005 Printed in Indonesia Printer, Jakarta Design and layout by Catur Wahyu and Gideon Suharyanto Cover photos (from left to right): Large mature trees found in primary forest provide various key habitat functions important for wildlife. (Photo by Herwasono Soedjito) An orphaned Bornean Gibbon (Hylobates muelleri), one of the victims of poor-logging and illegal hunting. (Photo by Kimabajo) Roads lead to various impacts such as the fragmentation of forest cover and the siltation of stream— other impacts are associated with improved accessibility for people. (Photo by Douglas Sheil) This book has been published with fi nancial support from UNESCO, ITTO, and SwedBio. The authors are responsible for the choice and presentation of the facts contained in this book and for the opinions expressed therein, which are not necessarily those of CIFOR, UNESCO, ITTO, and SwedBio and do not commit these organisations. -

(Tropidolaemus Subannulatus Gray, 1842) on Cebu Island, Philippines
Philippine Journal of Science RESEARCH NOTE 149 (3): 669-673, September 2020 ISSN 0031 - 7683 Date Received: 20 Feb 2020 First Distribution Record of North Philippine Temple Pitviper (Tropidolaemus subannulatus Gray, 1842) on Cebu Island, Philippines Archiebald Baltazar B. Malaki1,4*, Steve Michael T. Alcazar1,4, Edgardo P. Lillo1,6, Raamah C. Rosales3, Bernardo A. Redoblado2, John Lou B. Diaz2, and Inocencio E. Buot Jr.5 1Forestry Department; 2College of Forestry and Agriculture Cebu Technological University – Argao Campus, Lamacan, Argao 6021 Cebu, Philippines 3College of Arts and Sciences, Cebu Technological University – Main Campus Cor. M.J. Cuenco Ave., R. Palma St., Cebu City 6000 Philippines 4School of Environmental Science and Management; 5Institute of Biological Sciences 6Forest Biological Sciences Department, College of Forestry and Natural Resources University of the Philippines Los Bańos, College, Laguna 4031 Philippines This paper presents the newly documented single specimen of the North Philippine temple pitviper (Tropidolaemus subannulatus), one of the venomous endemic snakes of the Philippines. The species has never been recorded in Cebu Island in the last two waves of survey in 1986 and 2016. The new record for Cebu Island on 13 Apr 2018 was a male juvenile T. subannulatus in a diverse forest over limestone in Mount Lantoy key biodiversity area (KBA), with an elevation of 648 m having geographic coordinates of 9.91395ºN and 123.51207ºE in Barangay Cansuje, Argao, Cebu, Philippines. The specimen was recorded in the permanent vegetation plot no. 1, established within the secondary natural forest, perching on the vines (Piper sp.). Some tree species found within the collection area were the following: Garcinia rubra, Ficus ampelas, Canarium asperum, Calophyllum blancoi, Gomphandra luzoniensis, and Goniothalamus almeri. -

Evolutionary Interpretations of Nicotinic Acetylcholine Receptor Targeting Venom Effects by a Clade of Asian Viperidae Snakes
Neurotoxicity Research https://doi.org/10.1007/s12640-020-00211-2 ORIGINAL ARTICLE Evolutionary Interpretations of Nicotinic Acetylcholine Receptor Targeting Venom Effects by a Clade of Asian Viperidae Snakes Richard J. Harris1 & Christina N. Zdenek1 & Jordan Debono1 & David Harrich2 & Bryan G. Fry1 Received: 23 January 2020 /Revised: 29 March 2020 /Accepted: 17 April 2020 # Springer Science+Business Media, LLC, part of Springer Nature 2020 Abstract Ecological variability among closely related species provides an opportunity for evolutionary comparative studies. Therefore, to investigate the origin and evolution of neurotoxicity in Asian viperid snakes, we tested the venoms of Azemiops feae, Calloselasma rhodostoma, Deinagkistrodon acutus, Tropidolaeums subannulatus,andT. wagleri for their relative specificity and potency upon the amphibian, lizard, bird, rodent, and human α-1 (neuromuscular) nicotinic acetylcholine receptors. We utilised a biolayer interferometry assay to test the binding affinity of these pit viper venoms to orthosteric mimotopes of nicotinic acetylcholine receptors binding region from a diversity of potential prey types. The Tropidolaemus venoms were much more potent than the other species tested, which is consistent with the greater prey escape potential in arboreal niches. Intriguingly, the venom of C. rhodostoma showed neurotoxic binding to the α-1 mimotopes, a feature not known previously for this species. The lack of prior knowledge of neurotoxicity in this species is consistent with our results due to the bias in rodent studies and human bite reports, whilst this venom had a greater binding affinity toward amphibian and diapsid α-1 targets. The other large terrestrial species, D. acutus, did not display any meaningful levels of neurotoxicity. -

With a Key to the Complex in China and Adjacent Areas
s c^ ^ TRANSLATIONS OF RECENT DESCRIPTIONS OF ^^ PT CHINESE PITVIPERS OF THE TRIMERESURUS-COMFLEX (SERPENTES, VIPERIDAE), WITH A KEY TO THE COMPLEX IN CHINA AND ADJACENT AREAS Patrick David Laboratoire des Reptiles et Amphibiens Museum national d'Histoire naturelle, Paris & Haiyan Tong Laboratoire de Paleontologie Universite Paris-VI SMITHSONIAN HERPETOLOGICAL INFORMATION SERVICE NO. 112 1997 SMITHSONIAN HERPETOLOGICAL INFORMATION SERVICE The SHIS series publishes and distributes translations, bibliographies, indices, and similar items judged useful to individuals interested in the biology of amphibians and reptiles, but unlikely to be published in the normal technical journals. Single copies are distributed free to interested individuals. Libraries, herpetological associations, and research laboratories are invited to exchange their publications with the Division of Amphibians and Reptiles. We wish to encourage individuals to share their bibliographies, translations, etc. with other herpetologists through the SHIS series. If you have such items please contact George Zug for instructions on preparation and submission. Contributors receive 50 free copies. Please address all requests for copies and inquiries to George Zug, Division of Amphibians and Reptiles, National Museum of Natural History, Smithsonian Institution, Washington DC 20560 USA, Please include a self-addressed mailing label with requests. Historical perspective The renewed interest in herpetological researches that occurred in the 1970's in the People's Repubhc of China (hereafter merely referred to as China) led to the descriptions of many new taxa. Between 1972 and 1995, 17 species and 14 subspecies of snakes were described as new, either by Chinese or foreign authors. All species are still considered as valid, whereas seven subspecies proved to be junior synonyms of other taxa. -

A Review and Database of Snake Venom Proteomes
Toxins 2017, 9, 290; doi:10.3390/toxins9090290 S1 of S2 Supplementary Materials: A Review and Database of Snake Venom Proteomes Theo Tasoulis and Geoffrey K. Isbister * Table S1. Elapid species with unusual venom composition. % SPECIES PLA2 β-B SVMP LAAO 3FT OHN CRiSP MT CYS PDE REFERENCE WV Bungarus multicinctus 8.1 58.3 0.2 32.6 99.2 [1] China B.multicinctus 15.3 40.8 0.8 2.1 27.5 2.4 88.9 [2] Vietnam Calliophis bivirgata 41.1 18.7 14.4 22.6 0.6 1.3 98.7 [3] flaviceps Abbreviations: PLA2, phospholipase A2, β-B, β-bungarotoxin (PLA2 linked with a KUN), SVMP, snake venom metalloprotease, LAAO, L-amino acid oxidase, 3FT, three-finger toxin, OHN, Ohanin, CRiSP, Cysteine-Rich Secretary Protein, MT, maticotoxin, CYS, Cystatin PDE, phosphodiesterase, % WV, percentage of whole venom. Table S2. The unusual venom composition of Tropidolaemus wagleri (Temple Pit Viper[4]). SPECIES PLA2 SVSP SVMP LAAO LMMNLP PDE CTL WAGLERIN CYT % WV REF Tropidolaemus wagleri 7.3 5.5 1.7 1.7 34.5 1 3.5 38.2 0.9 94.3 [4] Abbreviations: PLA2, phospholipase A2, SVSP, snake venom serine protease, SVMP, snake venom metalloprotease, LAAO, L-amino acid oxidase, LMMNLP, low molecular mass non-lethal peptide, PDE, phosphodiesterase, CTL, C-type lectin, WAGLERIN, waglerin, CYT, cytotoxin, % WV, percentage of whole venom. Table S3. The remaining 36 protein families in viper and elapid venoms have been classed as rare protein families. Most have only been recorded in one or two species of snakes, and always made up less than 10% of the whole venom. -
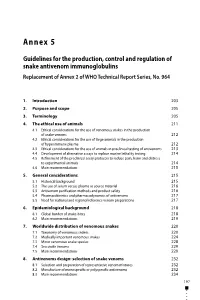
Guidelines for the Production, Control and Regulation of Snake Antivenom Immunoglobulins Replacement of Annex 2 of WHO Technical Report Series, No
Annex 5 Guidelines for the production, control and regulation of snake antivenom immunoglobulins Replacement of Annex 2 of WHO Technical Report Series, No. 964 1. Introduction 203 2. Purpose and scope 205 3. Terminology 205 4. The ethical use of animals 211 4.1 Ethical considerations for the use of venomous snakes in the production of snake venoms 212 4.2 Ethical considerations for the use of large animals in the production of hyperimmune plasma 212 4.3 Ethical considerations for the use of animals in preclinical testing of antivenoms 213 4.4 Development of alternative assays to replace murine lethality testing 214 4.5 Refinement of the preclinical assay protocols to reduce pain, harm and distress to experimental animals 214 4.6 Main recommendations 215 5. General considerations 215 5.1 Historical background 215 5.2 The use of serum versus plasma as source material 216 5.3 Antivenom purification methods and product safety 216 5.4 Pharmacokinetics and pharmacodynamics of antivenoms 217 5.5 Need for national and regional reference venom preparations 217 6. Epidemiological background 218 6.1 Global burden of snake-bites 218 6.2 Main recommendations 219 7. Worldwide distribution of venomous snakes 220 7.1 Taxonomy of venomous snakes 220 7.2 Medically important venomous snakes 224 7.3 Minor venomous snake species 228 7.4 Sea snake venoms 229 7.5 Main recommendations 229 8. Antivenoms design: selection of snake venoms 232 8.1 Selection and preparation of representative venom mixtures 232 8.2 Manufacture of monospecific or polyspecific antivenoms 232 8.3 Main recommendations 234 197 WHO Expert Committee on Biological Standardization Sixty-seventh report 9. -

An Inconspicuous, Conspicuous New Species of Asian Pipesnake, Genus
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Wolverhampton Intellectual Repository and E-theses Zootaxa 4093 (1): 001–025 ISSN 1175-5326 (print edition) http://www.mapress.com/j/zt/ Article ZOOTAXA Copyright © 2016 Magnolia Press ISSN 1175-5334 (online edition) http://doi.org/10.11646/zootaxa.4093.1.1 http://zoobank.org/urn:lsid:zoobank.org:pub:8C32F03F-E901-465D-B03D-7E6EEF288329 An inconspicuous, conspicuous new species of Asian pipesnake, genus Cylindrophis (Reptilia: Squamata: Cylindrophiidae), from the south coast of Jawa Tengah, Java, Indonesia, and an overview of the tangled taxonomic history of C. ruffus (Laurenti, 1768) MAX KIECKBUSCH1,4,§, SVEN MECKE1,§, LUKAS HARTMANN1, LISA EHRMANTRAUT1, MARK O’SHEA2 & HINRICH KAISER3 1Department of Animal Evolution and Systematics and Zoological Collection Marburg, Faculty of Biology, Philipps-Universität Mar- burg, Karl-von-Frisch-Straße 8, 35032 Marburg, Germany 2Faculty of Sciences and Engineering, University of Wolverhampton, Wulfruna Street, Wolverhampton, WV1 1LY, United Kingdom; and West Midland Safari Park, Bewdley, Worcestershire DY12 1LF, United Kingdom 3Department of Biology, Victor Valley College, 18422 Bear Valley Road, Victorville, California 92395, USA; and Department of Verte- brate Zoology, National Museum of Natural History, Smithsonian Institution, Washington, DC 20013, USA 4Corresponding author. E-mail: [email protected] §Co-first authors, listed in alphabetical order Abstract We describe a new species of Cylindrophis currently known only from Grabag, Purworejo Regency, Jawa Tengah Pro- vince (Central Java), Java, Indonesia. Cylindrophis subocularis sp. nov. can be distinguished from all congeners by the presence of a single, eponymous subocular scale between the 3rd and 4th or 4th and 5th supralabial, preventing contact be- tween the 4th or 5th supralabial and the orbit, and by having the prefrontal in narrow contact with or separated from the orbit. -

Table of Contents (PDF)
April 6, 2021 u vol. 118 u no. 14 From the Cover e2021311118 Ancient origins of oral venom e2021535118 Tornado strength and damage-based ratings e2013894118 Evaluating oil and gas well integrity e2013097118 Health benefits of natural sounds e2016337118 Invasive species in the global pet trade Contents THIS WEEK IN PNAS—This week’s research highlights Cover image: Pictured is a Bornean eiti1421118 In This Issue keeled pit viper (Tropidolaemus subannulatus). Agneesh Barua and — Alexander S. Mikheyev examined gene CORE CONCEPTS A brief introduction to emerging topics in science regulatory networks associated with e2104652118 Muography offers a new way to see inside a multitude of objects toxin production in snakes and found David Adam a metavenom network composed of more than 3,000 housekeeping genes. RETROSPECTIVE The findings suggest that snakes likely – developed venom from an ancient oral e2103938118 Alexander Spirin (1931 2020): A visionary scientist, a teacher, secretory system that was adapted to a colleague, a friend handle high protein loads. This ancient Valentina Evdokimova, Yuri Svitkin, and Nahum Sonenberg system is conserved between reptiles and mammals, suggesting that many COMMENTARIES mammals may harbor the potential to ’ become venomous under the right e2102056118 A slime mold s remembrance of things past conditions. See the article by Barua and Robert H. Austin Mikheyev, e2021311118. Image credit: See companion article, e2007815118, in vol. 118, issue 10 Anton Sorokin (photographer). e2102057118 Metabolic plasticity allows cancer cells to thrive under nutrient starvation Wilhelm Palm See companion article, e2003014118, in vol. 118, issue 10 e2102055118 Why does passion matter more in individualistic cultures? Jeanne L. -

Reported Primers
Russian Journal of Herpetology Vol. 26, No. 2, 2019, pp. 111 – 122 DOI: 10.30906/1026-2296-2019-26-2-111-122 A NEW SPECIES OF PITVIPER (SERPENTES: VIPERIDAE: Trimeresurus LACEPÈDE, 1804) FROM WEST KAMENG DISTRICT, ARUNACHAL PRADESH, INDIA Ashok Captain,1# V. Deepak,2,3# Rohan Pandit,4,7 Bharat Bhatt,5 and Ramana Athreya6,7* Submitted August 13, 2018 A new species of pitviper, Trimeresurus arunachalensis sp. nov., is described based on a single specimen. It differs from all known congeners by the following combination of characters — 19:17:15 acutely keeled dorsal scale rows (except first row — keeled or smooth); overall reddish-brown coloration; white dorsolateral stripe on outer posterior edges of ventrals and sometimes first dorsal scale row; 7 supralabials; 6 – 7 scales between supraoculars; 145 ventrals; 51 paired subcaudals (excluding the terminal scale); single anal; a sharply defined canthus rostralis with the margin overhanging the loreal region; a distinctly concave rostral scale with the upper edge projecting well beyond its lower margin; an unforked, attenuate hemipenis that extends to the 8th subcaudal scale, and has no visible spines. DNA phylogenetic analysis indicates that the new species is distinct from congeners and nested well within the Trimeresurus clade. The closest relative based on available DNA data is T. tibetanus. The new spe- cies is presently known from a single locality — Ramda, West Kameng, Arunachal Pradesh, northeastern India. Keywords: Crotalinae; snake; taxonomy; Trimeresurus arunachalensis sp. nov.; viper. INTRODUCTION 1804) comprising more than 90 species in total, Trimere- surus is the most diverse group with 50 known species Of the eight genera of pitvipers found in Asia (Callo- distributed across south and south-east Asia (e.g., Uetz et selasma Cope, 1860; Deinagkistrodon Gloyd, 1979; al., 2018).