Clinical Governance Committee Papers 040320
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

East Neuk Community Forum- Zoom Meeting-15/10/20, Chaired by Martin Dibbs, Kingsbarns Community Council
EAST NEUK COMMUNITY FORUM- ZOOM MEETING-15/10/20, CHAIRED BY MARTIN DIBBS, KINGSBARNS COMMUNITY COUNCIL PRESENT; VARIOUS COMMUNITY COUNCIL REPRESENTATIVES, INCLUDING CRAIL, ANSTRUTHER, KINGSBARNS, BOARHILLS AND DUNINO, ELIE AND PITTENWEEM COUNCILLORS HOLT, PORTEOUS AND DOCHERTY COUNCILLOR ROSS VETTRAINO, FIFE COUNCIL, CONVENER- ENVIRONMENT, PROTECTIVE SERVICES AND COMMUNITY SAFETY COMMITTEE GILLIAN DUNCAN, EAST NEUK FIRST RESPONDERS AND ENCEPT (EAST NEUK COMMUNITY EMERGENCY PLANNING TEAM) SONJA POTJEWIJD AND CRISPIN HAYES, ENCAP (EAST NEUK COMMUNITY ACTION PLAN) APOLOGIES; POLICE SCOTLAND 1. RECYCLING CENTRES IN EAST NEUK There have been various issues since March 2020, due to lockdown with people accessing recycling centres in our area. Particularly with people who do not access to a computer to be able to book times, the elderly in particular and Fife council’s refusal for pick ups, larger vehicles, vans and trailers to be allowed in to drop off rubbish. Councillor Holt stressed the difference between our area, being largely rural and agricultural compared to cities to Councillor Vettraino. She also stressed that we have one of the largest proportion of over 85’s in our area who have needs to be addressed regarding the above topic and especially need further help during covid. Councillor Vettraino advised that trailers, some pickups are now allowed to use the recycling centres. White goods can now be unloaded, as well wood. Rubble cannot be unloaded. AirBnb rubbish is counted as commercial so they should not be using facility. Question was asked whether the recycling centre at Pittenweem could change its opening times, Councillor Vettraino to check. 2. REWILDING Various comments were made by CC’s that there had been no consultation between fife council and the CC’s regarding rewilding in the east Neuk. -
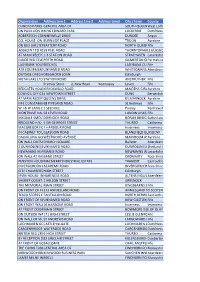
I General Area of South Quee
Organisation Address Line 1 Address Line 2 Address Line3 City / town County DUNDAS PARKS GOLFGENERAL CLUB- AREA IN CLUBHOUSE OF AT MAIN RECEPTION SOUTH QUEENSFERRYWest Lothian ON PAVILLION WALL,KING 100M EDWARD FROM PARK 3G PITCH LOCKERBIE Dumfriesshire ROBERTSON CONSTRUCTION-NINEWELLS DRIVE NINEWELLS HOSPITAL*** DUNDEE Angus CCL HOUSE- ON WALLBURNSIDE BETWEEN PLACE AG PETERS & MACKAY BROS GARAGE TROON Ayrshire ON BUS SHELTERBATTERY BESIDE THE ROAD ALBERT HOTEL NORTH QUEENSFERRYFife INVERKEITHIN ADJACENT TO #5959 PEEL PEEL ROAD ROAD . NORTH OF ENT TO TRAIN STATION THORNTONHALL GLASGOW AT MAIN RECEPTION1-3 STATION ROAD STRATHAVEN Lanarkshire INSIDE RED TELEPHONEPERTH ROADBOX GILMERTON CRIEFFPerthshire LADYBANK YOUTHBEECHES CLUB- ON OUTSIDE WALL LADYBANK CUPARFife ATR EQUIPMENTUNNAMED SOLUTIONS ROAD (TAMALA)- IN WORKSHOP OFFICE WHITECAIRNS ABERDEENAberdeenshire OUTSIDE DREGHORNDREGHORN LOAN HALL LOAN Edinburgh METAFLAKE LTD UNITSTATION 2- ON ROAD WALL AT ENTRANCE GATE ANSTRUTHER Fife Premier Store 2, New Road Kennoway Leven Fife REDGATES HOLIDAYKIRKOSWALD PARK- TO LHSROAD OF RECEPTION DOOR MAIDENS GIRVANAyrshire COUNCIL OFFICES-4 NEWTOWN ON EXT WALL STREET BETWEEN TWO ENTRANCE DOORS DUNS Berwickshire AT MAIN RECEPTIONQUEENS OF AYRSHIRE DRIVE ATHLETICS ARENA KILMARNOCK Ayrshire FIFE CONSTABULARY68 PIPELAND ST ANDREWS ROAD POLICE STATION- AT RECEPTION St Andrews Fife W J & W LANG LTD-1 SEEDHILL IN 1ST AID ROOM Paisley Renfrewshire MONTRAVE HALL-58 TO LEVEN RHS OFROAD BUILDING LUNDIN LINKS LEVENFife MIGDALE SMOLTDORNOCH LTD- ON WALL ROAD AT -

Codebook for IPUMS Great Britain 1851-1881 Linked Dataset
Codebook for IPUMS Great Britain 1851-1881 linked dataset 1 Contents SAMPLE: Sample identifier 12 SERIAL: Household index number 12 SEQ: Index to distinguish between copies of households with multiple primary links 12 PERNUM: Person index within household 13 LINKTYPE: Link type 13 LINKWT: Number of cases in linkable population represented by linked case 13 NAMELAST: Last name 13 NAMEFRST: First name 13 AGE: Age 14 AGEMONTH: Age in months 14 BPLCNTRY: Country of birth 14 BPLCTYGB: County of birth, Britain 20 CFU: CFU index number 22 CFUSIZE: Number of people in individuals CFU 23 CNTRY: Country of residence 23 CNTRYGB: Country within Great Britain 24 COUNTYGB: County, Britain 24 ELDCH: Age of eldest own child in household 27 FAMSIZE: Number of own family members in household 27 FAMUNIT: Family unit membership 28 FARM: Farm, NAPP definition 29 GQ: Group quarters 30 HEADLOC: Location of head in household 31 2 HHWT: Household weight 31 INACTVGB: Adjunct occupational code (Inactive), Britain 31 LABFORCE: Labor force participation 51 MARRYDAU: Number of married female off-spring in household 51 MARRYSON: Number of married male off-spring in household 51 MARST: Marital status 52 MIGRANT: Migration status 52 MOMLOC: Mothers location in household 52 NATIVITY: Nativity 53 NCHILD: Number of own children in household 53 NCHLT10: Number of own children under age 10 in household 53 NCHLT5: Number of own children under age 5 in household 54 NCOUPLES: Number of married couples in household 54 NFAMS: Number of families in household 54 NFATHERS: Number of fathers -

Special Offers Heraldry Trades & Professions History Vital Records – Births, Marriage, Deaths Irish Ancestry Wills & Testaments
SCOTTISH GENEALOGY SOCIETY SALES CATALOGUE OCTOBER 2013 PLEASE NOTE THAT THE FULL SALES CATALOGUE IS AVAILABLE ONLINE AT: WWW.SCOTSGENEALOGY.COM/DOWNLOADS.ASPX THE CATALOGUE IS IN SECTIONS AS FOLLOWS SECTION TITLE SECTION TITLE JACOBITES ARMED FORCES MARINERS & SHIPS BURGH RECORDS MISCELLANEOUS CASTLES OF SCOTLAND MONUMENTAL INSCRIPTIONS CENSUS NAMES DIRECTORIES PEERAGE ECCLESIASTICAL PEOPLE & POLL TAX LISTS OF 1696 EDUCATION POLL & HEARTH TAX EMIGRANTS & IMMIGRANTS SOURCES & GUIDES HEIRS – CD ROM SPECIAL OFFERS HERALDRY TRADES & PROFESSIONS HISTORY VITAL RECORDS – BIRTHS, MARRIAGE, DEATHS IRISH ANCESTRY WILLS & TESTAMENTS All the sections are bookmarked in the pdf catalogue. To calculate the cost of postage take a note of the weight of the goods and consult the postage table at the back of the sales catalogue. This is only a guideline and we reserve the right to increase prices when necessary. Please indicate whether airmail or surface for overseas members and whether first or second class for UK members. Payment may be made in sterling. The sterling equivalent may be obtained from your local bank. The Society accepts MASTER, VISA OR MAESTRO cards The Society reserves the right to alter prices in accordance with changes in publishing costs. PLEASE ENSURE THE CARDHOLDER'S NAME, CARD NUMBER, EXPIRY DATE AND TYPE OF CARD, I.E. VISA OR MASTER, ARE CLEARLY STATED. DISCOUNT Members of the Society are allowed a discount of 10% on Scottish Genealogy Society publications marked with an * (excluding postage and packing) Enquiries regarding trade discount should be directed to The Sales Secretary 15 Victoria Terrace, Edinburgh EH1 2JL Scotland Fax and Tel. No. (UK) 0131 220 3677 E-mail addresses Sales only [email protected] Renewal of membership only [email protected] Website and online shop www.scotsgenealogy.com Scottish Charity No. -

CC Minutes 27 May 2021
BOARHILLS AND DUNINO COMMUNITY COUNCIL NOTES OF MEETING HELD THURSDAY 27 MAY 2021 BY ZOOM Present: Arlene Slaughter, Chair, Helen Raeside, Vice chair, Bobby Simpson (CC), Louise Roger, Councillor John Docherty, Councillor Bill Porteous, Ashley Raeside Apologies: Councillor Linda Holt, Janice Furness, Sybil Scott 1. Welcome by Chair, Arlene Slaughter 2. Declaration of Interest: None 3. Minutes of last meeting (March 25 2021): Accepted MATTERS ARISING: 1. END OF YEAR ACCOUNTS: The accounts to the year end 31 March 2021 have now been completed and checked and signed by Professor Alan Cairns, Boarhills. Many thanks to him for once again giving his time freely.The balance at the year end is £595.78. Fife Council's annual grant application for this year will be open shortly and the chair will apply for it 2. EAST NEUK COMMUNITY FORUM MEETING 7 APRIL 2021 Arlene attended this zoom meeting whereby the following was discussed: a) Gillian Duncan of East Neuk First Responders (FR)raised the issues they were having with both Fife Council Falls Team and Scottish Ambulance. They have approached both many times to offer their assistance but have met with opposition. FR are being contacted by not local relatives whose East Neuk elderly family member has fallen . They can often reach an elderly fall well in advance of the other services who can take hours. They have invested in hoist equipment but have now been advised by Fife Council (FC) that the council's liability insurance cannot cover them. Scottish Ambulance refuse to engage with FR nor call them in the event of a 999 call. -

The Castle Studies Group Bulletin Volume 33 January 2021
THE CASTLE STUDIES GROUP BULLETIN VOLUME 33 JANUARY 2021 Inside this issue Editorial Covid-19 is still very much part of our lives and continues to put a strain Editorial on all works of life. I hope this bulletin finds you safe and well. 1 CSG Online Talks Despite the limitations of normal proceedings, there have been some 1 excavations and surveys that have taken place and other castle related Covid-19 Heritage news. Thank you to those who have suggested and submitted pieces for Funding this bulletin. Also, as you can see below, the CSG online talks will be 2-3 starting this month. Scotland 4-18 Therron Welstead CSG Bulletin Editor Wales 18-20 …………………………………… England 21-23 CSG Online Talks Jersey With an uncertain 2021 ahead of us, we are looking at ways to put on 24 events for our members. This month we are launching a series of talks about castles. Dr. Penny Dransart will be delivering our inaugural talk on Post-Graduates Wednesday 27 January at 5.30pm. She will be speaking about Loch Leven 24-25 Castle in Scotland and the incarceration of Mary Queen of Scots. CST Registration is now open. 25-27 You will have a chance to ask questions after the talk. If you can’t make In Other News… it, we will upload the talk to YouTube. 27 The event will take place on Zoom. If you don’t have Zoom you can download it from their website or you can join meetings from your browser. There is a video guide, though it is likely to be more cumbersome than installing Zoom. -

The Fife Show Saturday 18 May 2013 · Kinloss · Cupar
THE FIFE SHOW SATURDAY 18 MAY 2013 · KINLOSS · CUPAR For online facilities and more visit WWW.FIFESHOW.COM THE FIFE AGricultural association PREMIUM LIST ENTERTAINMENT FOR ALL THE FAMILY 9AM - 5PM Adults £10 · OAPs £5 · Children under 14 FREE · FREE PARKING CLOSING DATE FOR ENTRIES THURSDAY 18 APRIL 2013 Further information available from the Secretary: Hilary Lumsden, Tel: 01334 829 184 Email: [email protected] FARM SALES & ACQUISITIONS THE FIFE AGRICULTURAL ASSOCIATION PROPERTY & LAND MANAGEMENT incorporating RESIDENTIAL SALES | LETTINGS THE EAST OF FIFE AGRICULTURAL ASSOCIATION and ENERGY | FORESTRY | SPORTING THE FIFE AGRICULTURAL SOCIETY HOLIDAY LETS | PROPERTY FINANCE A charity registered in Scotland SCO 11016 OFFICE BEARERS President Mr M Logan, Sypsies Vice-President Mr A Stewart, Kininmonth Past President Mr D McKerrow, Nochnarry Secretary & Treasurer Ms Hilary Lumsden Kerns Cottage, Chance Inn, Cupar, Fife, KY15 5QJ GENERAL COMMITTEE Anstruther and District A Cormack, Annfield; J Jack, Balhousie; A Smith, Auchendownie; D Paterson, Upper Largo; J Brown, Pittenweem; J Johnston, Branxton S Parsons, Balcaskie; Mrs G Rollins, Leven St Andrews and District R Brown, Radernie; J Eccles, Bruckley; J Stewart, Kininmonth; A Stevenson, Bonerbo; Mrs N Pargeter, St Andrews; J Wood, Brewsterwells; I Brown, Blebo Craigs; Mrs M Snow, St Andrews; Whether it's a farm or sporting estate, a country house or a castle, we are J Ballantyne, Balkaithly able to offer an unrivalled agency service. Our commitment to a high standard of Cupar and District -

Registration Districts of Scotland Guide
Alpha RD Name County or Burgh First yearLast year Rd Number Current Rd A Abbey (Burghal) Renfrew 1855 1878 Old RD 559 1 Today's RD 646 A Abbey (Landward) Renfrew 1855 1878 Old RD 559 2 Today's RD 644 A Abbey (Paisley) Renfrew 1670 1854 OPR 559 A Abbey St.Bathans Berwick 1715 1854 OPR 726 A Abbey St.Bathans Berwick 1855 1966 Old RD 726 Today's RD 785 A Abbotrule (Southdean and Abbotrule) Roxburgh 1696 1854 OPR 806 A Abbotshall Fife 1650 1854 OPR 399 A Abbotshall (Landward) Fife 1855 1874 Old RD 399 Today's RD 421 A Abdie Fife 1620 1854 OPR 400 A Abdie Fife 1855 1931 Old RD 400 Today's RD 416 A Aberchirder Banff 1968 1971 Old RD 146 Today's RD 294 A Aberchirder Banff 1972 2000 Old RD 294 Today's RD 293 A Abercorn Linlithgow (West Lothian) 1585 1854 OPR 661 A Abercorn West Lothian 1855 1969 Old RD 661 Today's RD 701 A Abercrombie or St.Monance Fife 1628 1854 OPR 454 A Aberdalgie Perth 1613 1854 OPR 323 A Aberdalgie Perth 1855 1954 Old RD 323 Today's RD 390 A Aberdeen Aberdeen 1560 1854 OPR 168 a A Aberdeen, Eastern District Aberdeen 1931 1967 Old RD 168 3 Today's RD 300 A Aberdeen, Northern District Aberdeen 1931 1967 Old RD 168 1 Today's RD 300 A Aberdeen, Old Machar Parish Aberdeen 1886 1897 Old RD 168 2 Today's RD 300 A Aberdeen, Southern District Aberdeen 1931 1967 Old RD 168 2 Today's RD 300 A Aberdeen Aberdeen 1968 1971 Old RD 168 A Aberdeen Aberdeen City 1972 2006 Old RD 300 Today's RD 300 A Aberdeen Aberdeen City 2007 Today's RD 300 A Aberdeenshire Aberdeenshire 2005 Today's RD 295 A Aberdour Fife 1650 1854 OPR 401 A Aberdour Aberdeen -

Crail Matters 7 January Issue 91
www.crailmatters.com CRAILW/C 7M January A2019. NTo 91 FTree - dEonatioRns welcS ome Suggested hard copy Donation 40p Crail; The Jewel of the East Neuk. A request for Help Crail Matters is distributed free of charge for both paper and digital issues and we accept advertisements without any charge. We do this because we strongly believe that by providing a vehicle for news of events, people and things, we are investing in our community. Although Crail Matters is independent of any political party or grouping (including the Com - munity Council), we believe that local democracy and community wellbeing thrives when people have an opportunity to access local information and opinion. We undertake to make our pages freely available to all who wish to contribute. We distribute 512 digital copies each week (growing by around 2 or 3/week), and a further 120 hard copies, giving a total distribution of around 630 issues/ week. On average, each week the digital copies are opened 1,300 times, suggesting recipients open each issue 2 or 3 times (perhaps on multiple computers/ mobile phones or by other family members). But providing this service costs money!! We estimate that each hard copy costs around 40p to produce, with in addition the back office costs of computers, software and licenses. A number of very loyal supporters make regular contributions to us - and for this we thank them and are very grateful, because this gives us the capacity to continue week by week. If you do not make a donation, would you consider doing so? Crail Matters operates as a non-profit making entity, and any surplus we generate is donated back into Crail. -

1861 Fife : 413 Carnbee Surname Forenames Age Place of Birth Bk Pge Sch
1861 Fife : 413 Carnbee Surname Forenames Age Place of birth Bk Pge Sch ...ff Ann ? FIF Ceres 3 11 56 Adamson David 10 FIF Cameron 1 5 19 Adamson Elizabeth 8 FIF Cameron 1 5 19 Adamson Elspeth 47 FIF Carnbee 1 5 19 Adamson Helen 13 FIF Cameron 1 5 19 Adamson Isabella 1 FIF Carnbee 1 5 19 Adamson Janet 5 FIF Ceres 1 5 19 Adamson Marjory 19 FIF Cameron 2 15 77 Adamson Walter 45 FIF Cameron 1 5 19 Aitchison Agnes 49 FIF Newburn 4 4 18 Aitchison Isabella 24 FIF Newburn 4 4 18 Aitchison Robert 55 FIF Carnbee 4 4 18 Aitken Alexander 8 FIF Carnbee 1 7 32 Aitken Alison F A 23 FIF Leuchars 3 2 6 Aitken Andrew 33 FIF Carnbee 2 3 12 Aitken Andrew 66 FIF Carnbee 2 2 12 Aitken Ann 27 FIF Carnbee 2 3 12 Aitken David 1 mo FIF Carnbee 3 2 6 Aitken David 33 FIF Carnbee 3 3 14 Aitken Elizabeth 59 FIF Carnbee 1 7 30 Aitken George 28 FIF St Andrews 1 7 31 Aitken Henry 23 FIF Ceres 2 7 36 Aitken James 27 FIF Kinghorn 3 2 6 Aitken James 67 FIF St Andrews 3 3 14 Aitken Janet 47 MLN St Cuthbert 1 7 32 Aitken Margaret 25 FIF Carnbee 2 3 12 Aitken Margaret 29 FIF Carnbee 3 3 14 Aitken Margaret 68 FIF Carnbee 3 3 14 Allan Agnes 4 FIF Carnbee 2 11 59 Allan Agnes 33 FIF Crail 2 11 59 Allan Betsy 11 FIF Carnbee 3 8 42 Allan James 34 FIF Elie 2 11 59 Allan Jane 3 FIF Carnbee 3 8 42 Allan Margaret 8 FIF Carnbee 2 11 59 Allan Margaret 8 FIF Crail 3 8 42 Allan Margaret C 36 FIF Carnbee 3 8 42 Allan Mary 6 FIF Carnbee 2 11 59 Allan William 15 FIF Carnbee 3 8 42 Allan William 42 FIF Crail 3 8 42 Anderson Alexander 4 FIF Carnbee 2 2 10 Anderson David 10 FIF Strathmiglo 2 -

Lucania, 2 Beley Bridge Dunino, St Andrews, Fife
OUTSIDE ENERGY PERFORMANCE CERTIFICATE To the front is a lawned garden surrounded by a EPC Rating Band E. mature hedge with double garage beyond. To the rear is a paved terrace, summer house lawned COUNCIL TAX garden and mature trees leading down to Dunino Council Tax Band G. The annual Council Tax Burn. payable at present is £2190.33 Dundee 18 miles Lucania, 2 Beley Bridge St Andrews 4.5 miles Double Garage One remote controlled door and Kirkcaldy 23 miles Dunino, Edinburgh 49.5 miles 5.85m x 5.76m one manual operated. FIXTURES AND FITTINGS 19’2” x 18’10” All fitted floor coverings are included in the sale. St Andrews, Fife Summer House Built of timber with double doors. Other moveable contents and fittings may be 2.4m x 2.33m available by separate negotiation. 7’10” x 7’7” ASKING PRICE Offers over £395,000 are invited. OFFERS TO:- Bradburne & Co., 139 South Street, St Andrews, Fife. KY16 9UN. Fax 01334 474399. IMPORTANT NOTICE These particulars do not constitute any part of an offer or a contract. All statements contained herein, while believed to be correct, are not guaranteed. Intending purchasers must satisfy themselves by inspection or otherwise as to the correctness of each of the statements VIEWING contained in these particulars. Strictly by appointment with the Selling Agents – A closing date for offers may be fixed by the Selling Agents and 01334 479479. prospective purchasers are urged to note their interest formally to the Selling Agents. The Sellers reserve the right to conclude a bargain for the sale of any portions of the subjects of sale ahead of a notified closing SERVICES date and will not be obliged to accept either the highest or any offer for Mains electricity and water. -

SPECIAL OFFERS - Castles Castles of Grampian & Angus
SCOTTISH GENEALOGY SOCIETY SALES CATALOGUE JANUARY 2012 PLEASE NOTE THAT THE FULL SALES CATALOGUE WILL ONLY BE AVAILABLE ON-LINE UPDATES TO THIS CATALOGUE WILL HAPPEN ON A REGULAR BASIS THE CATALOGUE IS IN SECTIONS AS FOLLOWS When using this pdf download select the bookmark tab in the document. The section titles will provide a quick link to the desired section by clicking on the section title. If a section title has a + by it click on the + to expand that section To calculate the cost of postage take a note of the weight of the goods and consult the postage table at the back of the sales catalogue. This is only a guideline and we reserve the right to increase prices when necessary. Please indicate whether airmail or surface for overseas members and whether first or second class for UK members. Payment may be made in sterling. The sterling equivalent may be obtained from your local bank. The Society accepts MASTER, VISA OR MAESTRO cards The Society reserves the right to alter prices in accordance with changes in publishing costs. PLEASE ENSURE THE CARDHOLDER'S NAME, CARD NUMBER, EXPIRY DATE AND TYPE OF CARD, I.E. VISA OR MASTER, ARE CLEARLY STATED. DISCOUNT Members of the Society are allowed a discount of 10% on Scottish Genealogy Society publications marked with an * (excluding postage and packing) Enquiries regarding trade discount t should be directed to: The Sales Secretary 15 Victoria Terrace, Edinburgh EH1 2JL Scotland Fax and Tel. No. (UK) 0131 220 3677 E-mail addresses: Sales only [email protected] Renewal of membership only [email protected] Website and online shop www.scotsgenealogy.com Scottish Charity No.