Public Accounts Committee Public Document Pack
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

City and County of Swansea Scrutiny Programme
CITY AND COUNTY OF SWANSEA NOTICE OF MEETING You are invited to attend a Meeting of the SCRUTINY PROGRAMME COMMITTEE At: Committee Room 2, Civic Centre, Swansea On: Monday, 11 March, 2013 Time: 4.30 pm AGENDA Page No. 1. Apologies for Absence. 2. To receive Disclosures of Personal and Prejudicial Interests. 1 3. To approve the Minutes of the Scrutiny Programme Committee 2 - 11 held on 11 February 2013. 4. Crime & Disorder Scrutiny: Performance of Safer Swansea 12 - 69 Partnership - Presentation followed by Questions to Co-Chairs of the Partnership: • Chief Superintendent Julian Williams (South Wales Police) • Reena Owen (Corporate Director – Environment) 5. Follow Up on Previous Scrutiny Reports: 70 - 82 a) Swansea City Centre (first follow up) (Joint Report of the Cabinet Members for Place and Regeneration) 6. Single Integrated Plan Consultation: a) Report Back from Councillor Consultation Seminar on Swansea's New 83 - 94 Single Integrated Plan. b) Scrutiny Arrangements for Swansea Local Service Board. 95 - 98 7. Annual Self Evaluation - Education Services to Children and 99 - 187 Young People 2012-2013. 8. Scrutiny Work Programme: 188 - 201 a) The Committee Work Plan. b) Progress on Informal Scrutiny Panels and Working Groups. 9. Scrutiny Letters: a) Letter to / from Cabinet Member for Well Being re. Child & Family 202 - 208 Services Performance Panel. b) Letter to / from Cabinet Member for Place re. Local Flood Risk 209 - 215 Management Scrutiny Working Group. 10. Date and Time of Future Meetings for 2012/13 Municipal Year (all on Mondays at 4.30 p.m.) - 8 April 2013. Patrick Arran Head of Legal, Democratic Services & Procurement Monday, 4 March 2013 Contact: Samantha Woon - Tel: (01792) 637292 Agenda Item 2 Disclosures of Personal Interest from Members To receive Disclosures of Personal Interest from Members in accordance with the provisions of the Code of Conduct adopted by the City and County of Swansea. -

The Glamorgan-Gwent Archaeological Trust Half
THE GLAMORGAN-GWENT ARCHAEOLOGICAL TRUST High Street Presumed layout of burgage plots Outer Ditch High Street Excavated section of outer Bailey ditch Presumed line of medieval town wall Ditch awe Goat Street Goat Medieval course Old of River Tawe Castle River T New Castle Cross Street Wind Street St Mary's Church 14th century St David's hospital preserved as part of Fisher Street the Cross Keys public house Areas of 13th and 14th Century pits Line of medieval boundary ditch GRID for Swansea's N 0 100metres lower suburb HALF-YEARLY REVIEW 2010 & ANNUAL REVIEW OF PROJECTS 2009-2010 STE GI RE E D The Glamorgan-Gwent Archaeological Trust Ltd R O I A R N Heathfield House Heathfield Swansea SA1 6EL G IO A N ISAT Cover images from top: The ‘wandering wall’ on Cefn Car. Part of a stone inscription, probably a tombstone, referring to an ‘unjust fate’. It was found in the debris of the tower building shown below it. Aerial close-up of the herring-bone stone foundations of the tower building discovered during the building of a new coach park near Celtic Manor. Plan showing the ‘old’ and ‘new’ Swansea Castle and the probable medieval town layout. The reverse (tail side) of an extremely rare Henry 1 silver penny, struck in Pembroke probably between 1115 and 1120. This is the earliest coin yet found in Swansea. A 19th century worker’s house in a small settlement of at least five houses and a barn at Ffos-y-fran near Merthyr Tydfil. The settlement is thought to date back to the mid- 18th century when the Dowlais Ironworks was established. -

FFRWYTH YR HAF Nid Y Clawr Cyfansoddiadau Ryn Ni’N Gyfarwydd Â’I Weld Bob Blwyddyn Yw Hwn, Ond Rhyw Flwyddyn Fel ‘Na Yw Hi Wedi Bod
D u d y s g RHIF 377 MEDI 2020 £1.00 FFRWYTH YR HAF Nid y clawr Cyfansoddiadau ryn ni’n gyfarwydd â’i weld bob blwyddyn yw hwn, ond rhyw flwyddyn fel ‘na yw hi wedi bod. Yr hyn gewch chi yn y gyfrol hon yn bennaf yw cerddi buddugol Cystadleuaeth y Stôl Farddoniaeth a’r Stôl Ryddiaith, ond hefyd y gweithiau a ddaeth yn ail ac yn drydydd. Terwyn Tomos o Landudoch a enillodd y Stôl Farddoniaeth, a Llŷr Gwyn Lewis y Stôl Rhyddiaith. Mae sylwadau’r beirniaid yma hefyd, ond yn ogystal mae cerdd yr un gan dri mab Parc Nest, ynghyd â cherddi newydd ar gyfer yr Ŵyl AmGen gan nifer o Brifeirdd Coronog a Chadeiriol y Genedlaethol dros y blynyddoedd. Gwledd yn wir! Os nad ydych chi wedi darllen y gyfrol, ewch ar unwaith i brynu copi - byddwch wrth eich boddl Mae’n flasus iawn. Afalau Surion Bach Mwyar Duon’ AC O FLAS GWAHANOL 1 1 GOLYGYDD Y MIS Mary Jones Y GAMBO MIS HYDREF Eleri Evans Glasfryn, Tanygroes SA43 2JE Rhif ôn: 01239 810871 e-bost: [email protected] Pwyllgor a deunydd i mewn erbyn 29 Medi Dosbarthu dydd Iau 15 Hydref 2.00yp PWYLLGOR GWAITH Bryngwyn: Linda Morgan Plwmp a Phentre-Gât: Y GAMBO (01239 711249) Celia Richardson a Nigel Blake, Cadeirydd: Marlene Evans (01239 710708) (01239 851300) Eleri Evans (01239 810871) Brynhoffnant: Llinos Davies [email protected] [email protected] (01239 654135) Pontgarreg: Lynda Evans Ysgrifennydd a Clwb 500: [email protected] [email protected] John Davies, Y Graig, Aber-porth Caerwedros: Aled a Heledd Dafis (01239 654277) (01239 810555) (01545 561355) Rhydlewis: Vera Davies e-bost: [email protected] [email protected] (01239 851489) Trysoryddion: Des ac Esta Ceinewydd: Wendy Davies Sarnau a Penmorfa: Davies, Min-y-Maes, Penparc, (01545 560344) Alison Vaughan-Jones Aberteifi SA43 1RE Coed-y-bryn: Yn eisiau (01239 654610) [email protected] (01239 613447) Croeslan: Marlene E. -

HEFCW Circular W20/09HE: Annex B 1 Research Wales Innovation Fund
HEFCW circular W20/09HE: Annex B Research Wales Innovation Fund Strategy 2020/21 – 2022/23 Institution: Swansea University RWIF strategy lead: Prof. Marcus Doel, Deputy PVC – Research & Innovation Prof. Martin Stringer, PVC – Student Experience & Civic Mission Emma Dunbar- Head of Engagement, Innovation, Employability & Enterprise, REIS Email: [email protected] [email protected] [email protected] Telephone : 07860736047 (Emma Dunbar) Section A: Overview 1. Strategic ambitions Please provide an overview of your institution’s 3 year [and beyond if longer term plans are available] approach to research and innovation activity which will be supported by RWIF. You may wish to highlight broad areas which you are targeting, and describe how RWIF funding will align with your institutional mission and internal strategies. [max 300 words] This 3 year strategy comes at a particular moment in our history, when celebrating our centenary, we have had to come together as a community in response to the Covid-19 pandemic. We will use this opportunity to reflect on what we might achieve over the next few years that will resonate for our second century. We are proud to belong to the City of Swansea and the wider Swansea Bay City Region (SBCR) and we celebrate that heritage. We will strengthen our position within the SBCR, as the region’s major university, with the quality and scale of research and innovation to facilitate powerful strategic collaborations between universities, government funding bodies, our extensive SME network, large companies, and their supply chains; and to deliver transformational economic and social benefits both within Wales, the UK and across the rest of the world. -

The Story of a Man Called Daltone
- The Story of a Man called Daltone - “A semi-fictional tale about my Dalton family, with history and some true facts told; or what may have been” This story starts out as a fictional piece that tries to tell about the beginnings of my Dalton family. We can never know how far back in time this Dalton line started, but I have started this when the Celtic tribes inhabited Britain many yeas ago. Later on in the narrative, you will read factual information I and other Dalton researchers have found and published with much embellishment. There also is a lot of old English history that I have copied that are in the public domain. From this fictional tale we continue down to a man by the name of le Sieur de Dalton, who is my first documented ancestor, then there is a short history about each successive descendant of my Dalton direct line, with others, down to myself, Garth Rodney Dalton; (my birth name) Most of this later material was copied from my research of my Dalton roots. If you like to read about early British history; Celtic, Romans, Anglo-Saxons, Normans, Knight's, Kings, English, American and family history, then this is the book for you! Some of you will say i am full of it but remember this, “What may have been!” Give it up you knaves! Researched, complied, formated, indexed, wrote, edited, copied, copy-written, misspelled and filed by Rodney G. Dalton in the comfort of his easy chair at 1111 N – 2000 W Farr West, Utah in the United States of America in the Twenty First-Century A.D. -
Information for Candidates APPOINTMENT of NON
NHS Trust Non-executive Director Information for Candidates APPOINTMENT OF NON-EXECUTIVE DIRECTOR OF WELSH AMBULANCE SERVICES NHS TRUST NHS Trust Non-executive Director Diversity Statement The Welsh Government believes that public bodies should have board members who reflect Welsh society - people from all walks of life - to help them understand people's needs and make better decisions. This is why the Welsh Government is encouraging a wide and diverse range of individuals to apply for appointments to public bodies. Applications are particularly welcome from all under-represented groups including women, people under 30 years of age, members of ethnic minorities, disabled people, lesbian, gay, bisexual and trans people. Positive about Disability The Welsh Government operates a Positive about Disabled People scheme and welcome applications from people with disabilities. The scheme guarantees an interview to disabled people if they meet the minimum criteria for the post. The application form also enables you to detail any specific needs or equipment that you may need if invited to attend an interview. NHS Trust Non-executive Director Background and Context The Welsh Government’s vision for the NHS in Wales is “to create world-class health”. This vision is set out in Together for Health, and is based on providing more community services closer to home, alongside specialist centres of excellence, which give better results for patients. Who does what in the NHS in Wales? The Minister for Health and Social Services is responsible for all aspects of the NHS in Wales. Details of the Ministers responsibilities can be found here http://gov.wales/about/cabinet/cabinetm/markdrakeford The National Delivery Group, forms part of the Welsh Government’s Health and Social Services (HSSG) Group, and is responsible for overseeing the development and delivery of NHS services across Wales. -

Dyffryn Teifi O Dan Garped O Eira
Rhifyn 280 - 60c www.clonc.co.uk Chwefror 2010 Papur Bro ardal plwyfi: Cellan, Llanbedr Pont Steffan, Llanbedr Wledig, Llanfair Clydogau, Llangybi, Llanllwni, Llanwenog, Llanwnnen, Llanybydder, Llanycrwys ac Uwch Gaeo a Phencarreg Athrawes Ysgol Cadwyn Siarad Sul am dros arall o Cyhoeddus 40 mlynedd gyfrinachau y C.Ff.I. Tudalen 7 Tudalen 16 Tudalen 26 Dyffryn Teifi o dan garped o eira Rhai o blant Ysgol Carreg Hirfaen yn slejo pan nad oedd ysgol. Disgyblion Dosbarth y Babanod Llanwnnen gyda’u dynion eira! Bach o bopeth . Manon Richards Brenhines Clybiau Ffermwyr Ifanc Ceredigion ac Emyr Clwb Ffermwyr Ifanc Llanllwni. Codwyd swm teilwng o £1470.53 yn y Evans Ffermwr Ifanc y flwyddyn yn cyflwyno siec am £657 i swyddogion Sioe a Threialon Cŵn defaid gyda’r elw yn mynd tuag at Uned Gofal y Fron, cangen Llanybydder o Diabetes UK Cymru sef Mair Evans (chwith), a Betty Ysbyty Llanelli. Cyfrannwyd cyfanswm y casgliad sef £83.72 o’r Cwrdd Jones a Bet Davies (dde), arian a godwyd mewn Cymanfa Ganu a drefnwyd Diolchgarwch i Adran yr Urdd, Llanfihangel-ar-Arth a chyflwynwyd arian gan Manon ac Emyr ac a gynhaliwyd yng Nghapel y Groes Llanwnnen. y Canu Carolau o £715.04 i St John’s. Yn y llun mae cynrychiolwyr Adran yr Urdd, Llanfihangel-ar-Arth, St John’s, Mr a Mrs Davies ar ran Ysbyty Llanelli ac aelodau’r clwb. Swyddogion Sefydliad y Merched Coedmor, Ann Lewis, Elma Phillips, Pwyllgor ‘Apêl y Gors 09’ yn cyflwyno siec am£40,36 .64 i’r Chwaer Gwyneth Morgan a Joyce Williams yn cyflwyno sieciau am £170 yr un i Tim Linda Jones a’r Chwaer Hilary Jones o Uned Dydd Chemotherapy, Ysbyty Dicker a Gethin Jones, Cyd-Ymatebwyr Cyntaf Llambed [First Response] Glangwili, Caerfyrddin. -
![Wastewater Growth IAP Response [WWS2 – Lines 25, 26 and 30]](https://docslib.b-cdn.net/cover/7818/wastewater-growth-iap-response-wws2-lines-25-26-and-30-927818.webp)
Wastewater Growth IAP Response [WWS2 – Lines 25, 26 and 30]
IAP Response Ref B.22.WSH.CE.A1 Wastewater Growth IAP Response [WWS2 – Lines 25, 26 and 30] 1 April 2019 PR19 Business Plan Supporting Information Page 1 of 15 IAP Response – Ref CE.A1 Contents 1. OFWAT’S COST EFFICIENCY CHALLENGE .................................................................................................. 3 2. SUMMARY OF OUR RESPONSE TO THE INITIAL ASSESSMENT BY OFWAT ................................................ 3 3. WASTEWATER GROWTH ENHANCEMENT MODEL ................................................................................... 4 4. SEWER FLOODING ................................................................................................................................... 5 5. GWILI GWENDRAETH GROWTH ............................................................................................................. 12 PR19 Business Plan Supporting Information Page 2 of 15 IAP Response – Ref CE.A1 1. Ofwat’s cost efficiency challenge We have carefully reviewed Ofwat’s approach to modelling Wastewater Growth expenditure. Ofwat have combined the costs for new developments and growth, growth at sewage treatment works and reducing risks of sewer flooding into one wastewater growth assessment, stating that these areas are interlinked with each other and are driven by population increase and demand growth. Our review has demonstrated that the results of the modelling are materially skewed by the inclusion of a significant outlier in Hafren Dyfrdwy. In addition, the modelling does not adequately account for all -

NHS Wales Decarbonisation Strategic Delivery Plan
NHS Wales Decarbonisation Strategic Delivery Plan 2021-2030 (including Technical Appendices) Published March 2021 NHS Wales Decarbonisation Strategic Delivery Plan Who we are Established in 2001, the Carbon Trust works with businesses, governments and institutions around the world, helping them contribute to, and benefit from, a more sustainable future through carbon reduction, resource efficiency strategies, and commercialising low carbon businesses, systems and technologies. The Carbon Trust: • works with corporates and governments, helping them to align their strategies with climate science and meet the goals of the Paris Agreement; • provides expert advice and assurance, giving investors and financial institutions the confidence that green finance will have genuinely green outcomes; and • supports the development of low carbon technologies and solutions, building the foundations for the energy system of the future. Headquartered in London, the Carbon Trust has a global team of over 200 staff, representing over 30 nationalities, based across five continents. 1 NHS Wales Decarbonisation Strategic Delivery Plan The Carbon Trust’s mission is to accelerate the move to a sustainable, low carbon economy. It is a world leading expert on carbon reduction and clean technology. As a not-for-dividend group, it advises governments and leading companies around the world, reinvesting profits into its low carbon mission. The NHS Wales Shared Services Partnership (NWSSP) is an independent organisation, owned and directed by NHS Wales. NWSSP supports -

Pre-Industrial Swansea: Siting and Development
34 PRE-INDUSTRIAL SWANSEA: SITING AND DEVELOPMENT Gerald Gabb Abstract This article is an investigation of what, in the eleventh or twelfth century, drew its founders to the location where Swansea grew up, why their successors remained there, and how and why the settlement developed the form it did. Starting with the Norse origins of Swansea followed by its Norman developments, the article draws on what limited evidence is available, including archaeological evidence from recent excavations. The article considers the importance of Swansea’s topography as a trading port and discusses some of its important medieval buildings, including the castle and major churches. This article is an investigation of what, in the eleventh or twelfth century, drew its founders to the location where Swansea grew up, why their successors remained there, and how and why the settlement developed the form it did. It addresses data from at least seven centuries, across which continuities figure strongly. Even when John Evans published his ‘Plan of Swansea’ in 1823 the area of the town had only crept a little beyond the perimeter of the town walls of the fourteenth century.1 Industrialization was soon to trigger rapid expansion, but what follow are some thoughts on the slower changes which came before that. Two things should be borne in mind. In any study of this sort, direct evidence is minimal. To adopt the technique of reductio ad absurdum for a moment, there is no extant report made by a steward to the first lord of Gower, Henry, Earl of Warwick, on the best place for his caput castle and town, nor, and this is less ludicrous, a burgess minute from the 1640s on where the new market house should go. -
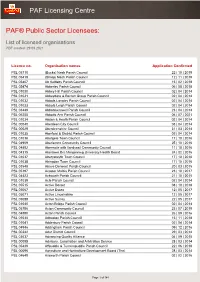
List of Licensed Organisations PDF Created: 29 09 2021
PAF Licensing Centre PAF® Public Sector Licensees: List of licensed organisations PDF created: 29 09 2021 Licence no. Organisation names Application Confirmed PSL 05710 (Bucks) Nash Parish Council 22 | 10 | 2019 PSL 05419 (Shrop) Nash Parish Council 12 | 11 | 2019 PSL 05407 Ab Kettleby Parish Council 15 | 02 | 2018 PSL 05474 Abberley Parish Council 06 | 08 | 2018 PSL 01030 Abbey Hill Parish Council 02 | 04 | 2014 PSL 01031 Abbeydore & Bacton Group Parish Council 02 | 04 | 2014 PSL 01032 Abbots Langley Parish Council 02 | 04 | 2014 PSL 01033 Abbots Leigh Parish Council 02 | 04 | 2014 PSL 03449 Abbotskerswell Parish Council 23 | 04 | 2014 PSL 06255 Abbotts Ann Parish Council 06 | 07 | 2021 PSL 01034 Abdon & Heath Parish Council 02 | 04 | 2014 PSL 00040 Aberdeen City Council 03 | 04 | 2014 PSL 00029 Aberdeenshire Council 31 | 03 | 2014 PSL 01035 Aberford & District Parish Council 02 | 04 | 2014 PSL 01036 Abergele Town Council 17 | 10 | 2016 PSL 04909 Aberlemno Community Council 25 | 10 | 2016 PSL 04892 Abermule with llandyssil Community Council 11 | 10 | 2016 PSL 04315 Abertawe Bro Morgannwg University Health Board 24 | 02 | 2016 PSL 01037 Aberystwyth Town Council 17 | 10 | 2016 PSL 01038 Abingdon Town Council 17 | 10 | 2016 PSL 03548 Above Derwent Parish Council 20 | 03 | 2015 PSL 05197 Acaster Malbis Parish Council 23 | 10 | 2017 PSL 04423 Ackworth Parish Council 21 | 10 | 2015 PSL 01039 Acle Parish Council 02 | 04 | 2014 PSL 05515 Active Dorset 08 | 10 | 2018 PSL 05067 Active Essex 12 | 05 | 2017 PSL 05071 Active Lincolnshire 12 | 05 -

Deposit - Revised Carmarthenshire Local Development Plan 2018 – 2033
Deposit - Revised Carmarthenshire Local Development Plan 2018 – 2033 Draft for Reporting Revised Carmarthenshire Local Development Plan 2018 - 2033 Foreword To be inserted Deposit Draft – Version for Reporting i Revised Carmarthenshire Local Development Plan 2018 - 2033 Contents: Page No: Policy Index iii How to View and Comment on the Deposit Revised LDP vi 1. Introduction 1 2. What is the Deposit Plan? 3 3. Influences on the Plan 7 4. Carmarthenshire - Strategic Context 12 5. Issues Identification 25 6. A Vision for ‘One Carmarthenshire’ 28 7. Strategic Objectives 30 8. Strategic Growth and Spatial Options 36 9. A New Strategy 50 10. The Clusters 62 11. Policies 69 12. Monitoring and Implementation 237 13. Glossary 253 Appendices: Appendix 1: Context – Legislative and National Planning Policy Guidance Appendix 2: Regional and Local Strategic Context Appendix 3: Supplementary Planning Guidance Appendix 4: Minerals Sites Appendix 5: Active Travel Routes Appendix 6: Policy Assessment Appendix 7: Housing Trajectory Appendix 8: Waste Management Facilities Deposit Draft – Version for Reporting ii Revised Carmarthenshire Local Development Plan 2018 - 2033 Policy Index Page No. Strategic Policy – SP1: Strategic Growth 70 • SG1: Regeneration and Mixed Use Sites 72 • SG2: Reserve Sites 73 • SG3: Pembrey Peninsula 75 Strategic Policy – SP2: Retail and Town Centres 76 • RTC1: Carmarthen Town Centre 82 • RTC2: Protection of Local Shops and Facilities 84 • RTC3: Retail in Rural Areas 85 Strategic Policy – SP3: A Sustainable Approach to Providing New