Blake's Pouch Cyst
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Review of Spinal Cord Basics of Neuroanatomy Brain Meninges
Review of Spinal Cord with Basics of Neuroanatomy Brain Meninges Prof. D.H. Pauža Parts of Nervous System Review of Spinal Cord with Basics of Neuroanatomy Brain Meninges Prof. D.H. Pauža Neurons and Neuroglia Neuron Human brain contains per 1011-12 (trillions) neurons Body (soma) Perikaryon Nissl substance or Tigroid Dendrites Axon Myelin Terminals Synapses Neuronal types Unipolar, pseudounipolar, bipolar, multipolar Afferent (sensory, centripetal) Efferent (motor, centrifugal, effector) Associate (interneurons) Synapse Presynaptic membrane Postsynaptic membrane, receptors Synaptic cleft Synaptic vesicles, neuromediator Mitochondria In human brain – neurons 1011 (100 trillions) Synapses – 1015 (quadrillions) Neuromediators •Acetylcholine •Noradrenaline •Serotonin •GABA •Endorphin •Encephalin •P substance •Neuronal nitric oxide Adrenergic nerve ending. There are many 50-nm-diameter vesicles (arrow) with dark, electron-dense cores containing norepinephrine. x40,000. Cell Types of Neuroglia Astrocytes - Oligodendrocytes – Ependimocytes - Microglia Astrocytes – a part of hemoencephalic barrier Oligodendrocytes Ependimocytes and microglial cells Microglia represent the endogenous brain defense and immune system, which is responsible for CNS protection against various types of pathogenic factors. After invading the CNS, microglial precursors disseminate relatively homogeneously throughout the neural tissue and acquire a specific phenotype, which clearly distinguish them from their precursors, the blood-derived monocytes. The ´resting´ microglia -

Subarachnoid Trabeculae: a Comprehensive Review of Their Embryology, Histology, Morphology, and Surgical Significance Martin M
Literature Review Subarachnoid Trabeculae: A Comprehensive Review of Their Embryology, Histology, Morphology, and Surgical Significance Martin M. Mortazavi1,2, Syed A. Quadri1,2, Muhammad A. Khan1,2, Aaron Gustin3, Sajid S. Suriya1,2, Tania Hassanzadeh4, Kian M. Fahimdanesh5, Farzad H. Adl1,2, Salman A. Fard1,2, M. Asif Taqi1,2, Ian Armstrong1,2, Bryn A. Martin1,6, R. Shane Tubbs1,7 Key words - INTRODUCTION: Brain is suspended in cerebrospinal fluid (CSF)-filled sub- - Arachnoid matter arachnoid space by subarachnoid trabeculae (SAT), which are collagen- - Liliequist membrane - Microsurgical procedures reinforced columns stretching between the arachnoid and pia maters. Much - Subarachnoid trabeculae neuroanatomic research has been focused on the subarachnoid cisterns and - Subarachnoid trabecular membrane arachnoid matter but reported data on the SAT are limited. This study provides a - Trabecular cisterns comprehensive review of subarachnoid trabeculae, including their embryology, Abbreviations and Acronyms histology, morphologic variations, and surgical significance. CSDH: Chronic subdural hematoma - CSF: Cerebrospinal fluid METHODS: A literature search was conducted with no date restrictions in DBC: Dural border cell PubMed, Medline, EMBASE, Wiley Online Library, Cochrane, and Research Gate. DL: Diencephalic leaf Terms for the search included but were not limited to subarachnoid trabeculae, GAG: Glycosaminoglycan subarachnoid trabecular membrane, arachnoid mater, subarachnoid trabeculae LM: Liliequist membrane ML: Mesencephalic leaf embryology, subarachnoid trabeculae histology, and morphology. Articles with a PAC: Pia-arachnoid complex high likelihood of bias, any study published in nonpopular journals (not indexed PPAS: Potential pia-arachnoid space in PubMed or MEDLINE), and studies with conflicting data were excluded. SAH: Subarachnoid hemorrhage SAS: Subarachnoid space - RESULTS: A total of 1113 articles were retrieved. -

Diencephalic–Mesencephalic Junction Dysplasia: a Novel Recessive Brain Malformation
doi:10.1093/brain/aws162 Brain 2012: 135; 2416–2427 | 2416 BRAIN A JOURNAL OF NEUROLOGY Diencephalic–mesencephalic junction dysplasia: a novel recessive brain malformation Maha S. Zaki,1 Sahar N. Saleem,2 William B. Dobyns,3 A. James Barkovich,4 Hauke Bartsch,5 Anders M. Dale,5 Manzar Ashtari,6,7 Naiara Akizu,8 Joseph G. Gleeson8 and Ana Maria Grijalvo-Perez8 1 Department of Clinical Genetics, Division of Human Genetics and Genome Research, National Research Centre, Cairo 12311, Egypt 2 Department of Radiology, Cairo University, Cairo, Egypt 3 Department of Paediatrics, Seattle Children’s Research Institute, Seattle, WA 98195-6320, USA 4 Department of Radiology and Biomedical Imaging, University of California, San Francisco, 94143, USA 5 Multimodal Imaging Laboratory (MMIL), Departments of Radiology and Neurosciences, University of California, San Diego, 92093 USA 6 Diffusion Tensor Image Analyses and Brain Morphometry Centre, Children’s Hospital of Philadelphia, Philadelphia, PA 19104, USA 7 Department of Radiology, Children’s Hospital of Philadelphia, Philadelphia, PA 19104, USA 8 Neurogenetics Laboratory, Howard Hughes Medical Institute, Department of Neurosciences and Paediatrics, Rady Children’s Hospital, University of California, San Diego, 92093 USA Correspondence to: Dr Maha S. Zaki, Department of Clinical Genetics, Division of Human Genetics and Genome Research, National Research Centre, El-Tahrir Street, Dokki, Cairo 12311, Egypt E-mail: [email protected] or [email protected] We describe six cases from three unrelated consanguineous Egyptian families with a novel characteristic brain malformation at the level of the diencephalic–mesencephalic junction. Brain magnetic resonance imaging demonstrated a dysplasia of the diencephalic–mesencephalic junction with a characteristic ‘butterfly’-like contour of the midbrain on axial sections. -

Ultrasound Findings in Neonatal Meningitis—A Pictorial Review
Review Article Neonatal cranial sonography: ultrasound findings in neonatal meningitis—a pictorial review Nishant Gupta1, Hemal Grover2, Itisha Bansal3, Kusum Hooda4, Joshua M. Sapire5, Rama Anand6, Yogesh Kumar7 1Department of Radiology, Saint Vincent’s Medical Center, Bridgeport, CT, USA; 2Department of Neuroradiology, NYU Lagone Medical Center, New York, NY, USA; 3Department of Anesthesiology, New York Methodist Hospital, Brooklyn, New York, USA; 4Department of Radiology, Yale New Haven Health at Bridgeport Hospital, Bridgeport, CT, USA; 5Department of Neuroradiology, Saint Vincent’s Medical Center, Bridgeport, CT, USA; 6Department of Pediatric Radiology, Kalawati Saran Children Hospital, Shaheed Bhagat Singh Marg, New Delhi, India; 7Department of Neuroradiology, Yale New Haven Health at Bridgeport Hospital, Bridgeport, CT, USA Correspondence to: Nishant Gupta, MD, PDCC. Department of Radiology and Imaging, Saint Vincent’s Medical Center, 2800 Main Street, Bridgeport, CT 06606, USA. Email: [email protected]. Abstract: Neonatal bacterial meningitis is a common manifestation of late onset neonatal sepsis. Cranial sonography (CRS) has a crucial role in assessment of infants with clinical suspicion of bacterial meningitis as well as follows up of its complications. CRS is performed with high frequency transducer through anterior fontanelle in both coronal and sagittal planes. Various sonographic findings range from echogenic and widened sulci, ventriculomegaly, ventriculitis, hydrocephalus, extra-axial fluid collections, cerebritis -

Chapter III: Case Definition
NBDPN Guidelines for Conducting Birth Defects Surveillance rev. 06/04 Appendix 3.5 Case Inclusion Guidance for Potentially Zika-related Birth Defects Appendix 3.5 A3.5-1 Case Definition NBDPN Guidelines for Conducting Birth Defects Surveillance rev. 06/04 Appendix 3.5 Case Inclusion Guidance for Potentially Zika-related Birth Defects Contents Background ................................................................................................................................................. 1 Brain Abnormalities with and without Microcephaly ............................................................................. 2 Microcephaly ............................................................................................................................................................ 2 Intracranial Calcifications ......................................................................................................................................... 5 Cerebral / Cortical Atrophy ....................................................................................................................................... 7 Abnormal Cortical Gyral Patterns ............................................................................................................................. 9 Corpus Callosum Abnormalities ............................................................................................................................. 11 Cerebellar abnormalities ........................................................................................................................................ -

Ventriculomegaly
Great Ormond Street Hospital for Children NHS Foundation Trust: Information for Families Ventriculomegaly This information sheet from Great Ormond Street Hospital (GOSH) explains the causes, symptoms and treatment of ventriculomegaly and hydrocephalus and where to get help. Ventricles are cavities within the brain filled Without signs of increased pressure in the with cerebro-spinal fluid (CSF) acting as a brain (hydrocephalus), ventriculomegaly most ‘cushion’. CSF also supplies nutrients to the likely will not cause any problems. However, brain. The brain has four ventricles: two it can be linked with hydrocephalus and other lateral ventricles, the third ventricle and the problems. Ventriculomegaly can be diagnosed fourth ventricle. during pregnancy and occurs in around two CSF is created within the brain and flows from per cent of all pregnancies. the lateral ventricles into the third ventricle. It then flows through a narrow tube (the What causes cerebral aqueduct) into the fourth ventricle which lies towards the base of the brain. From ventriculomegaly? the fourth ventricle, it flows around the spinal In many cases, we do not know what causes cord and over the surface of the brain before ventriculomegaly (in the absence of any raised being re-absorbed. CSF pressure) but it can occur if there has been Ventriculomegaly is the medical term used to brain damage for any reason leading to loss describe enlargement of the ventricles of the of brain tissue. Often however it is a “chance” brain. Hydrocephalus is the term used when finding and when the ventricles are only a enlargement of the ventricles has been caused little enlarged of little significance. -

CT Based Study of Frontal Horn Ratio and Ventricular Index in South Indian Population
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 16, Issue 7 Ver. VI (July. 2017), PP 55-59 www.iosrjournals.org CT Based Study of Frontal Horn Ratio And Ventricular Index in South Indian Population *Dr.Arun Kumar S. MD1, Dr.S.MeenaKumari DMRD.,DNB.2, 3 4 Dr.A.Pavithra DNB. ,Dr.R.Saraswathy DMRD. 1(Associate Professor, Department of Radiology, Karpagam Faculty of Medical Sciences and Research, India) 2(Consultant Radiologist, Department of Radiology, Karpagam Faculty of Medical Sciences and Research, India) 3(Consultant Radiologist, Department of Radiology, Karpagam Faculty of Medical Sciences and Research, India) 4(Consultant Radiologist, Department of Radiology, Karpagam Faculty of Medical Sciences and Research, India) Corresponding author: *Dr. S.MeenaKumari DMRD.,DNB., Abstract: Introduction: Assessment of ventricular morphology and dimensions plays a crucial role in a wide range of clinical conditions associated with ventricular enlargement such as CNS infections, meningitis, and brain tumors . Of all the ventricular dimensions, linear ratios of lateral ventricles are the simplest to enumerate and also to reproduce. Objective: The aim of our study is to establish standard reference values for Frontal Horn Ratio (FHR) and Bicaudate - Frontal Index or Ventricular index using Computed Tomogram (CT) for normal South Indian population. Materials And Methods: One hundred subjects, with normal CT brain, were analyzed for this study retrospectively. Plain CT brain of all the patients was performed in Siemens Somatom Scope Multislice CT scanner. Results: In our study there was no statistically significant difference in mean FHR and ventricular index between genders. -

Morphometric Analysis of Ventricular System of Human Brain - a Study by Dissection Method
Jemds.com Original Research Article Morphometric Analysis of Ventricular System of Human Brain - A Study by Dissection Method Prabahita Baruah1, Purujit Choudhury2, Pradipta Ray Choudhury3 1Department of Anatomy, Silchar Medical College and Hospital, Silchar, Assam, India. 2Department of Surgery, Gauhati Medical College and Hospital, Guwahati, Assam, India. 3Department of Anatomy, Silchar Medical College and Hospital, Silchar, Assam, India. ABSTRACT BACKGROUND It is often a challenge to determine if the brain ventricles are within normal limits Corresponding Author: or swollen with the age of the patient. With a standardized and comparable system, Dr. Purujit Choudhury, it is therefore necessary to define normal ventricular size ranges. Cadaveric Associate Professor, dissection is always considered the gold standard of anatomical education. Present Department of Surgery, Gauhati Medical College and Hospital, work is undertaken to study morphometric analysis of lateral, third & fourth Guwahati, Assam, India. ventricles by dissection method. Morphometric assessment of the ventricular E-mail: [email protected] system is helpful in the diagnosis as well as classification of hydrocephalus and in the evaluation and monitoring of ventricular system enlargement during DOI: 10.14260/jemds/2020/121 ventricular shunt therapy. Financial or Other Competing Interests: METHODS None. Different parameters of all parts of lateral ventricle, third and fourth ventricle were How to Cite This Article: measured with digital vernier caliper in cadaveric brain specimens. The brain Baruah P, Choudhury P, Choudhury PR. specimens were obtained from dead bodies subjected to post-mortem Morphometric analysis of ventricular examinations in the Department of Forensic Medicine and from the dead bodies system of human brain- a study by voluntarily donated to the Department of Anatomy, Silchar Medical College, Silchar. -

Longitudinal Volumetric Assessment of Ventricular Enlargement in Pet Dogs Trained for Functional Magnetic Resonance Imaging (Fmri) Studies
veterinary sciences Article Longitudinal Volumetric Assessment of Ventricular Enlargement in Pet Dogs Trained for Functional Magnetic Resonance Imaging (fMRI) Studies 1, 2, , 2,3 2 4 Eva Gunde y,Kálmán Czeibert * y , Anna Gábor ,Dóra Szabó , Anna Kis , Attila Arany-Tóth 1, Attila Andics 2,3,Márta Gácsi 2,5 and Enik˝oKubinyi 2 1 Department and Clinic of Surgery and Ophthalmology, University of Veterinary Medicine, 1078 Budapest, Hungary; [email protected] (E.G.); [email protected] (A.A.-T.) 2 Department of Ethology, Institute of Biology, ELTE Eötvös Loránd University, 1117 Budapest, Hungary; [email protected] (A.G.); [email protected] (D.S.); [email protected] (A.A.); [email protected] (M.G.); [email protected] (E.K.) 3 MTA-ELTE (Hungarian Academy of Sciences–Eötvös Loránd University) ‘Lendulet¯ Neuroethology of Communication Research Group, 1117 Budapest, Hungary 4 Psychobiology Research Group, Institute of Cognitive Neuroscience and Psychology, Research Centre for Natural Sciences, 1117 Budapest, Hungary; [email protected] 5 MTA-ELTE Comparative Ethology Research Group, 1117 Budapest, Hungary * Correspondence: [email protected] These authors contributed equally to the work reported in this paper. y Received: 4 August 2020; Accepted: 2 September 2020; Published: 4 September 2020 Abstract: Background: Recent studies suggest that clinically sound ventriculomegaly in dogs could be a preliminary form of the clinically significant hydrocephalus. We evaluated changes of ventricular volumes in awake functional magnetic resonance imaging (fMRI) trained dogs with indirectly assessed cognitive abilities over time (thus avoiding the use of anaesthetics, which can alter the pressure). Our research question was whether ventricular enlargement developing over time would have any detrimental effect on staying still while being scanned; which can be extrapolated to the ability to pay attention and to exert inhibition. -

Lateral Atlanto-Occipital Space Puncture
CLINICAL ARTICLE J Neurosurg 129:146–152, 2018 A new method of subarachnoid puncture for clinical diagnosis and treatment: lateral atlanto-occipital space puncture Dianrong Gong, BS, Haiyan Yu, MS, and Xiaoling Yuan, MD Department of Neurology, Liaocheng People’s Hospital, Liaocheng, Shandong, China OBJECTIVE Lumbar puncture may not be suitable for some patients needing subarachnoid puncture, while lateral C1–2 puncture and cisterna magna puncture have safety concerns. This study investigated lateral atlanto-occipital space puncture (also called lateral cisterna magna puncture) in patients who needed subarachnoid puncture for clinical diagnosis or treatment. The purpose of the study was to provide information on the complications and feasibility of this technique and its potential advantages over traditional subarachnoid puncture techniques. METHODS In total, 1008 lateral atlanto-occipital space puncture procedures performed in 667 patients were retrospec- tively analyzed. The success rate and complications were also analyzed. All patients were followed up for 1 week after puncture. RESULTS Of 1008 lateral atlanto-occipital space punctures, 991 succeeded and 17 failed (1.7%). Fifteen patients (2.25%) reported pain in the ipsilateral external auditory canal or deep soft tissue, 32 patients (4.80%) had a transient increase in blood pressure, and 1 patient (0.15%) had intracranial hypotension after the puncture. These complications resolved fully in all cases. There were no serious complications. CONCLUSIONS Lateral atlanto-occipital space puncture is a feasible technique of subarachnoid puncture for clinical diagnosis and treatment. It is associated with a lower rate of complications than lateral C1–2 puncture or traditional (sub- occipital) cisterna magna puncture. -

Brachycephaly and Cerebrospinal Fluid Disorders
life Review The Need for Head Space: Brachycephaly and Cerebrospinal Fluid Disorders Clare Rusbridge 1,2,* and Penny Knowler 1 1 Faculty of Health & Medical Sciences, School of Veterinary Medicine, University of Surrey, Guildford GU2 7AL, UK; [email protected] 2 Fitzpatrick Referrals, Godalming GU7 2QQ, UK * Correspondence: [email protected] Abstract: Brachycephalic dogs remain popular, despite the knowledge that this head conformation is associated with health problems, including airway compromise, ocular disorders, neurological dis- ease, and other co-morbidities. There is increasing evidence that brachycephaly disrupts cerebrospinal fluid movement and absorption, predisposing ventriculomegaly, hydrocephalus, quadrigeminal cistern expansion, Chiari-like malformation, and syringomyelia. In this review, we focus on cere- brospinal fluid physiology and how this is impacted by brachycephaly, airorhynchy, and associated craniosynostosis. Keywords: ventriculomegaly; hydrocephalus; Chiari malformation; syringomyelia; canine; cran- iosynostosis; supracollicular fluid collection; quadrigeminal cistern; lateral aperture; sleep disordered breathing; brachycephalic obstructive airway disease 1. Introduction Brachycephalic dogs and cats have proved to be increasingly popular since they Citation: Rusbridge, C.; Knowler, P. were introduced to Europe in Victorian times. This rising popularity defies a high preva- The Need for Head Space: lence of conformation-related morbidity, including breathing, ocular, and neurological Brachycephaly and Cerebrospinal disorders [1,2]. Brachycephaly in domestic pets is a consequence of selecting for juvenile Fluid Disorders. Life 2021, 11, 139. characteristics of a flattened face and a rounded head [3]. Calvarial doming associated https://doi.org/10.3390/life11020139 with wide zygomatic arches and a wide, flattened, or convex palate is compensation for premature closure of skull-base sutures, including the basispheno-presphenoid syn- Academic Editor: Edgar Lehr chondrosis and spheno-occipital synchondrosis [4,5]. -
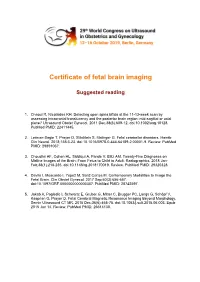
Certificate of Fetal Brain Imaging
Certificate of fetal brain imaging Suggested reading 1. Chaoui R, Nicolaides KH. Detecting open spina bifida at the 11-13-week scan by assessing intracranial translucency and the posterior brain region: mid-sagittal or axial plane? Ultrasound Obstet Gynecol. 2011 Dec;38(6):609-12. doi:10.1002/uog.10128. PubMed PMID: 22411445. 2. Lerman-Sagie T, Prayer D, Stöcklein S, Malinger G. Fetal cerebellar disorders. Handb Clin Neurol. 2018;155:3-23. doi:10.1016/B978-0-444-64189-2.00001-9. Review: PubMed PMID: 29891067. 3. Choudhri AF, Cohen HL, Siddiqui A, Pande V, Blitz AM. Twenty-Five Diagnoses on Midline Images of the Brain: From Fetus to Child to Adult. Radiographics. 2018 Jan- Feb;38(1):218-235. doi:10.1148/rg.2018170019. Review. PubMed PMID: 29320328. 4. Davila I, Moscardo I, Yepez M, Sanz Cortes M. Contemporary Modalities to Image the Fetal Brain. Clin Obstet Gynecol. 2017 Sep;60(3):656-667. doi:10.1097/GRF.0000000000000307. PubMed PMID: 28742597. 5. Jakab A, Pogledic I, Schwartz E, Gruber G, Mitter C, Brugger PC, Langs G, Schöpf V, Kasprian G, Prayer D. Fetal Cerebral Magnetic Resonance Imaging Beyond Morphology. Semin Ultrasound CT MR. 2015 Dec;36(6):465-75. doi:10.1053/j.sult.2015.06.003. Epub 2015 Jun 14. Review. PubMed PMID: 26614130. Ultrasound Obstet Gynecol 2007; 29: 109–116 Published online in Wiley InterScience (www.interscience.wiley.com). DOI: 10.1002/uog.3909 GUIDELINES Sonographic examination of the fetal central nervous system: guidelines for performing the ‘basic examination’ and the ‘fetal neurosonogram’ INTRODUCTION Some abnormalities may be visible in the first and early second trimesters6–11.