DRUG NAME: Cisplatin
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Evaluation of Response to Neoadjuvant Chemotherapy for Esophageal Cancer: PET Response Criteria in Solid Tumors Versus Response Evaluation Criteria in Solid Tumors
Journal of Nuclear Medicine, published on May 11, 2012 as doi:10.2967/jnumed.111.098699 Evaluation of Response to Neoadjuvant Chemotherapy for Esophageal Cancer: PET Response Criteria in Solid Tumors Versus Response Evaluation Criteria in Solid Tumors Masahiro Yanagawa*1, Mitsuaki Tatsumi*1,2, Hiroshi Miyata3, Eiichi Morii4, Noriyuki Tomiyama1, Tadashi Watabe2, Kayako Isohashi2, Hiroki Kato2, Eku Shimosegawa2, Makoto Yamasaki3, Masaki Mori3, Yuichiro Doki3, and Jun Hatazawa2 1Department of Radiology, Osaka University Graduate School of Medicine, Suita-city, Osaka, Japan; 2Department of Nuclear Medicine and Tracer Kinetics, Osaka University Graduate School of Medicine, Suita-city, Osaka, Japan; 3Department of Gastroenterological Surgery, Osaka University Graduate School of Medicine, Suita-city, Osaka, Japan; and 4Department of Pathology, Osaka University Graduate School of Medicine, Suita-city, Osaka, Japan onstrate the correlation between therapeutic responses and Recently, PET response criteria in solid tumors (PERCIST) have prognosis in patients with esophageal cancer receiving neoadju- been proposed as a new standardized method to assess vant chemotherapy. However, PERCIST was found to be the chemotherapeutic response metabolically and quantitatively. strongest independent predictor of outcomes. Given the signifi- The aim of this study was to evaluate therapeutic response to cance of noninvasive radiologic imaging in formulating clinical neoadjuvant chemotherapy for locally advanced esophageal treatment strategies, PERCIST might be considered more suit- cancer, comparing PERCIST with the currently widely used able for evaluation of chemotherapeutic response to esophageal response evaluation criteria in solid tumors (RECIST). Methods: cancer than RECIST. Fifty-one patients with locally advanced esophageal cancer who Key Words: RECIST; PERCIST; 18F-FDG PET; esophageal cancer; received neoadjuvant chemotherapy (5-fluorouracil, adriamycin, response to therapy and cisplatin), followed by surgery were studied. -

Induction with Mitomycin C, Doxorubicin, Cisplatin And
British Journal of Cancer (1999) 80(12), 1962–1967 © 1999 Cancer Research Campaign Article no. bjoc.1999.0627 Induction with mitomycin C, doxorubicin, cisplatin and maintenance with weekly 5-fluorouracil, leucovorin for treatment of metastatic nasopharyngeal carcinoma: a phase II study RL Hong1, TS Sheen2, JY Ko2, MM Hsu2, CC Wang1 and LL Ting3 Departments of 1Oncology, 2Otolaryngology and 3Radiation Therapy, National Taiwan University Hospital, National Taiwan University, No. 7, Chung-Shan South Road, Taipei 10016, Taiwan Summary The combination of cisplatin and 5-fluorouracil (5-FU) (PF) is the most popular regimen for treating metastatic nasopharyngeal carcinoma (NPC) but it is limited by severe stomatitis and chronic cisplatin-related toxicity. A novel approach including induction with mitomycin C, doxorubicin and cisplatin (MAP) and subsequent maintenance with weekly 5-FU and leucovorin (FL) were designed with an aim to reduce acute and chronic toxicity of PF. Thirty-two patients of NPC with measurable metastatic lesions in the liver or lung were entered into this phase II trial. Mitomycin C 8 mg m–2, doxorubicin 40 mg m–2 and cisplatin 60 mg m–2 were given on day 1 every 3 weeks as initial induction. After either four courses or remission was achieved, patients received weekly dose of 5-FU 450 mg m–2 and leucovorin 30 mg m–2 for maintenance until disease progression. With 105 courses of MAP given, 5% were accompanied by grade 3 and 0% were accompanied by grade 4 stomatitis. The dose-limiting toxicity of MAP was myelosuppression. Forty per cent of courses had grade 3 and 13% of courses had grade 4 leukopenia. -

Arsenic Trioxide Is Highly Cytotoxic to Small Cell Lung Carcinoma Cells
160 Arsenic trioxide is highly cytotoxic to small cell lung carcinoma cells 1 1 Helen M. Pettersson, Alexander Pietras, effect of As2O3 on SCLC growth, as suggested by an Matilda Munksgaard Persson,1 Jenny Karlsson,1 increase in neuroendocrine markers in cultured cells. [Mol Leif Johansson,2 Maria C. Shoshan,3 Cancer Ther 2009;8(1):160–70] and Sven Pa˚hlman1 1Center for Molecular Pathology, CREATE Health and 2Division of Introduction Pathology, Department of Laboratory Medicine, Lund University, 3 Lung cancer is the most frequent cause of cancer deaths University Hospital MAS, Malmo¨, Sweden; and Department of f Oncology-Pathology, Cancer Center Karolinska, Karolinska worldwide and results in 1 million deaths each year (1). Institute and Hospital, Stockholm, Sweden Despite novel treatment strategies, the 5-year survival rate of lung cancer patients is only f15%. Small cell lung carcinoma (SCLC) accounts for 15% to 20% of all lung Abstract cancers diagnosed and is a very aggressive malignancy Small cell lung carcinoma (SCLC) is an extremely with early metastatic spread (2). Despite an initially high aggressive form of cancer and current treatment protocols rate of response to chemotherapy, which currently com- are insufficient. SCLC have neuroendocrine characteristics bines a platinum-based drug with another cytotoxic drug and show phenotypical similarities to the childhood tumor (3, 4), relapses occur in the absolute majority of SCLC neuroblastoma. As multidrug-resistant neuroblastoma patients. At relapse, the efficacy of further chemotherapy is cells are highly sensitive to arsenic trioxide (As2O3) poor and the need for alternative treatments is obvious. in vitro and in vivo, we here studied the cytotoxic effects Arsenic-containing compounds have been used in tradi- of As2O3 on SCLC cells. -

Immunohistochemical Detection of WT1 Protein in a Variety of Cancer Cells
Modern Pathology (2006) 19, 804–814 & 2006 USCAP, Inc All rights reserved 0893-3952/06 $30.00 www.modernpathology.org Immunohistochemical detection of WT1 protein in a variety of cancer cells Shin-ichi Nakatsuka1, Yusuke Oji2, Tetsuya Horiuchi3, Takayoshi Kanda4, Michio Kitagawa5, Tamotsu Takeuchi6, Kiyoshi Kawano7, Yuko Kuwae8, Akira Yamauchi9, Meinoshin Okumura10, Yayoi Kitamura2, Yoshihiro Oka11, Ichiro Kawase11, Haruo Sugiyama12 and Katsuyuki Aozasa13 1Department of Clinical Laboratory, National Hospital Organization Osaka Minami Medical Center, Kawachinagano, Osaka, Japan; 2Department of Biomedical Informatics, Osaka University Graduate School of Medicine, Suita, Osaka, Japan; 3Department of Surgery, National Hospital Organization Osaka Minami Medical Center, Kawachinagano, Osaka, Japan; 4Department of Gynecology, National Hospital Organization Osaka Minami Medical Center, Kawachinagano, Osaka, Japan; 5Department of Urology, National Hospital Organization Osaka Minami Medical Center, Kawachinagano, Osaka, Japan; 6Department of Pathology, Kochi Medical School, Kohasu, Oko-cho, Nankoku City, Kochi, Japan; 7Department of Pathology, Osaka Rosai Hospital, Sakai, Osaka, Japan; 8Department of Pathology, Osaka Medical Center and Research Institute of Maternal and Child Health, Izumi, Osaka, Japan; 9Department of Cell Regulation, Faculty of Medicine, Kagawa University, Miki-cho, Kida-gun, Kagawa, Japan; 10Department of Surgery, Osaka University Graduate School of Medicine, Suita, Osaka, Japan; 11Department of Molecular Medicine, Osaka University Graduate School of Medicine, Suita, Osaka, Japan; 12Department of Functional Diagnostic Science, Osaka University Graduate School of Medicine, Suita, Osaka, Japan and 13Department of Pathology, Osaka University Graduate School of Medicine, Suita, Osaka, Japan WT1 was first identified as a tumor suppressor involved in the development of Wilms’ tumor. Recently, oncogenic properties of WT1 have been demonstrated in various hematological malignancies and solid tumors. -

Prognostic Factors Affecting Mortality in Patients with Esophageal Gists
JBUON 2020; 25(1): 497-507 ISSN: 1107-0625, online ISSN: 2241-6293 • www.jbuon.com Email: [email protected] ORIGINAL ARTICLE Prognostic factors affecting mortality in patients with esophageal GISTs Dimitrios Schizas1, George Bagias2, Prodromos Kanavidis1, Demetrios Moris1, Eleftherios Spartalis3, Christos Damaskos3, Nikolaos Garmpis3, Ioannis Karavokyros1, Evangelos P. Misiakos4, Theodore Liakakos1 11st Department of Surgery, Laikon General Hospital, National and Kapodistrian University of Athens, Athens, Greece; 2Clinic for General, Visceral and Transplant Surgery, Hannover Medical School, Hannover, Germany; 32nd Department of Propedeutic Surgery, Laikon General Hospital, National and Kapodistrian University of Athens, Athens, Greece; 43rd Department of Surgery, Attikon University Hospital, National and Kapodistrian University of Athens, Athens, Greece. Summary Purpose: Esophageal gastrointestinal stromal tumors (54.3%), followed by tumor enucleation (45.7%). The median (GISTs) compose a very rare clinical entity, representing follow-up period was 34 months; tumor recurrence occurred 0.7% of all GISTs. Therefore, the clinicopathological factors in 18 cases (18.9%) and 19 died of disease (19.2%). The over- that affect mortality are currently not adequately examined. all survival rate was 75.8%. We found out that tumor size We reviewed individual cases of esophageal GISTs found in and high mitotic rate (>10 mitosis per hpf) were significant the literature in order to identify the prognostic factors af- prognostic factors for survival. Presence of symptoms, ul- fecting mortality. ceration, and tumor necrosis as well as tumor recurrence were also significant prognostic factors (p<0.01). Methods: MEDLINE, EMBASE, and the Cochrane Library were systematically searched to identify clinical studies and Conclusions: Esophageal GISTs’ tumor size and mitotic case reports referring to esophageal GISTs. -

Pharmacotherapy of Impaired Mucociliary Clearance in Non-CF Pediatric Lung Disease
Pediatric Pulmonology 42:989–1001 (2007) State of the Art Pharmacotherapy of Impaired Mucociliary Clearance in Non-CF Pediatric Lung Disease. A Review of the Literature 1 1 1,2 Ruben Boogaard, MD, * Johan C. de Jongste, MD, PhD, and Peter J.F.M. Merkus, MD, PhD Summary. Mucoactive agents are used to treat a variety of lung diseases involving impaired mucociliary clearance or mucus hypersecretion. The mucoactive agents studied most frequently are N-acetylcysteine (NAC), recombinant human DNase (rhDNase), and hypertonic saline. Studies on the efficacy of these have been mainly conducted in adults, and in patients with cystic fibrosis (CF). The exact role of mucoactive agents in children with non-CF lung disease is not well established. We present an overview of the current literature reporting clinical outcome measures of treatment with NAC, rhDNase, and hypertonic saline in children. Pediatr Pulmonol. 2007; 42:989–1001. ß 2007 Wiley-Liss, Inc. Key words: mucolytic; sulfhydryl compounds; N-acetylcysteine; dornase alfa; hyper- tonic saline; respiratory tract disease. INTRODUCTION One possible means to evaluate a mucoactive agent is to assess its effect on mucociliary clearance (MCC) or cough Mucus clearance is an important primary innate airway clearance with the use of radiolabeled aerosol. Discussing defense mechanism, and our understanding of the key this subject is outside the scope of this review. Moreover, parameters underlying its function has grown rapidly in the studies on mucoactive agents in CF patients, and studies last decade.1,2 Impaired mucus clearance or mucus hyper- on physiotherapy or secretion clearance techniques in secretion are important clinical features in diseases such as (pediatric) lung disease patients have been reviewed by cystic fibrosis (CF), recurrent bronchitis, asthma, and others, and will therefore not be discussed in this review. -

Supportive Care Medications
th Clinical Pharmacy Guide: Cancer Drug Treatment Assessment and Review 5 Edition Supportive Care Medications Contents Introduction ................................................................................................................. 2 Supportive Care Information in Protocols .................................................................... 2 Antidiarrheals .............................................................................................................. 5 Loperamide ............................................................................................................. 5 Antiemetics .................................................................................................................. 6 Emetogenicity .......................................................................................................... 7 Types of Chemotherapy-Induced Nausea and Vomiting .......................................... 7 Classifications of Antiemetics .................................................................................. 8 Anti-infective Agents .................................................................................................. 10 Antibiotics .............................................................................................................. 10 Antivirals ................................................................................................................ 11 Arthralgias/Myalgias ................................................................................................. -

The Diagnostic and Prognostic Value of a Liquid Biopsy for Esophageal Cancer: a Systematic Review and Meta-Analysis
cancers Review The Diagnostic and Prognostic Value of a Liquid Biopsy for Esophageal Cancer: A Systematic Review and Meta-Analysis Daisuke Matsushita 1,* , Takaaki Arigami 2 , Keishi Okubo 1, Ken Sasaki 1, Masahiro Noda 1, Yoshiaki Kita 1, Shinichiro Mori 1, Yoshikazu Uenosono 3, Takao Ohtsuka 1 and Shoji Natsugoe 4 1 Department of Digestive Surgery, Breast and Thyroid Surgery, Kagoshima University Graduate School of Medical and Dental Sciences, Kagoshima 890-8520, Japan; [email protected] (K.O.); [email protected] (K.S.); [email protected] (M.N.); [email protected] (Y.K.); [email protected] (S.M.); [email protected] (T.O.) 2 Department of Onco-biological Surgery, Kagoshima University Graduate School of Medical and Dental Sciences, Kagoshima 890-8520, Japan; [email protected] 3 Department of Surgery, Jiaikai Imamura General Hospital, Kagoshima 890-0064, Japan; [email protected] 4 Department of Surgery, Gyokushoukai Kajiki Onsen Hospital, Aira 899-5241, Japan; [email protected] * Correspondence: [email protected]; Tel.: +81-99-275-5361; Fax: +81-99-265-7426 Received: 9 September 2020; Accepted: 18 October 2020; Published: 21 October 2020 Simple Summary: The “liquid biopsy” is a novel concept for detecting circulating biomarkers in the peripheral blood of patients with various cancers, including esophageal cancer. There are two main methods to identify circulating cancer related biomarkers such as morphological techniques or molecular biological techniques. -

Combination of Oxoplatin with Other FDA-Approved Oncology Drugs
International Journal of Molecular Sciences Article Theoretical Prediction of Dual-Potency Anti-Tumor Agents: Combination of Oxoplatin with Other FDA-Approved Oncology Drugs José Pedro Cerón-Carrasco Reconocimiento y Encapsulación Molecular, Universidad Católica San Antonio de Murcia Campus los Jerónimos, 30107 Murcia, Spain; [email protected] Received: 16 April 2020; Accepted: 2 July 2020; Published: 3 July 2020 Abstract: Although Pt(II)-based drugs are widely used to treat cancer, very few molecules have been approved for routine use in chemotherapy due to their side-effects on healthy tissues. A new approach to reducing the toxicity of these drugs is generating a prodrug by increasing the oxidation state of the metallic center to Pt(IV), a less reactive form that is only activated once it enters a cell. We used theoretical tools to combine the parent Pt(IV) prodrug, oxoplatin, with the most recent FDA-approved anti-cancer drug set published by the National Institute of Health (NIH). The only prerequisite imposed for the latter was the presence of one carboxylic group in the structure, a chemical feature that ensures a link to the coordination sphere via a simple esterification procedure. Our calculations led to a series of bifunctional prodrugs ranked according to their relative stabilities and activation profiles. Of all the designed molecules, the combination of oxoplatin with aminolevulinic acid as the bioactive ligand emerged as the most promising strategy by which to design enhanced dual-potency oncology drugs. Keywords: cancer; drug design; organometallics; platinum-based drugs; bifunctional compounds; theoretical tools 1. Introduction The unexpected discovery of the bioactivity of Pt salts by Rosenberg about 60 years ago opened the door to a new type of cancer treatment: chemotherapy with transition metals [1]. -
Tumor Budding Is Associated with an Increased Risk of Lymph Node
Modern Pathology (2014) 27, 1578–1589 1578 & 2014 USCAP, Inc All rights reserved 0893-3952/14 $32.00 Tumor budding is associated with an increased risk of lymph node metastasis and poor prognosis in superficial esophageal adenocarcinoma Michael S Landau1, Steven M Hastings1, Tyler J Foxwell1, James D Luketich2, Katie S Nason2 and Jon M Davison1 1Department of Pathology, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA and 2Department of Cardiothoracic Surgery, University of Pittsburgh School of Medicine, Pittsburgh, PA, USA The treatment approach for superficial (stage T1) esophageal adenocarcinoma critically depends on the pre-operative assessment of metastatic risk. Part of that assessment involves evaluation of the primary tumor for pathologic characteristics known to predict nodal metastasis: depth of invasion (intramucosal vs submucosal), angiolymphatic invasion, tumor grade, and tumor size. Tumor budding is a histologic pattern that is associated with poor prognosis in early-stage colorectal adenocarcinoma and a predictor of nodal metastasis in T1 colorectal adenocarcinoma. In a retrospective study, we used a semi-quantitative histologic scoring system to categorize 210 surgically resected, superficial (stage T1) esophageal adenocarcinomas according to the extent of tumor budding (none, focal, and extensive) and also evaluated other known risk factors for nodal metastasis, including depth of invasion, angiolymphatic invasion, tumor grade, and tumor size. We assessed the risk of nodal metastasis associated with tumor budding in univariate analyses and controlled for other risk factors in a multivariate logistic regression model. In all, 41% (24 out of 59) of tumors with extensive tumor budding (tumor budding in Z3 20X microscopic fields) were metastatic to regional lymph nodes, compared with 10% (12 out of 117) of tumors with no tumor budding, and 15% (5 out of 34) of tumors with focal tumor budding (Po0.001). -
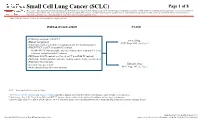
Small Cell Lung Cancer (SCLC) Algorithm
Small Cell Lung Cancer (SCLC) Page 1 of 8 Disclaimer: This algorithm has been developed for MD Anderson using a multidisciplinary approach considering circumstances particular to MD Anderson’s specific patient population, services and structure, and clinical information. This is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient's care. This algorithm should not be used to treat pregnant women. Note: Consider Clinical Trials as treatment options for eligible patients. INITIAL EVALUATION STAGE ● Pathology consistent with SCLC Limited Stage ● History and physical AJCC Stage I-III2, see Page 2 ● Laboratory studies to include hematological and full chemistry panels ● FDG PET/CT and CT chest with IV contrast ○ If FDG PET/CT not available: nuclear medicine bone scan and CT chest, abdomen, and pelvis with IV contrast ● MRI brain with IV contrast (preferred) or CT head with IV contrast ● MRI spine, lumbar puncture and bone marrow aspirate/biopsy as indicated ● Pulmonary function tests 1 Extensive Stage ● Lifestyle risk assessment AJCC Stage IV3, see Page 3 ● Molecular profiling (for never smokers) AJCC = American Joint Committee on Cancer 1 See Physical Activity, Nutrition, and Tobacco Cessation algorithms; ongoing reassessment of lifestyle risks should be a part of routine clinical practice 2 Limited stage: Stage I-III (T any, N any, M0) per AJCC 8th edition or disease confined to the ipsilateral hemithorax -

Cisplatin and Etoposide (Lung)
Cisplatin and Etoposide (lung) _____________________________________________________________________________________________ Indication First line chemotherapy for patients with small cell lung cancer (SCLC), who have a good performance status (WHO PS 0-2). Concomitant radiotherapy may start with cycle 2. ICD-10 codes Codes pre-fixed with C34 Regimen details Day Drug Dose Route 1 Cisplatin 75-80mg/m² IV infusion 1 Etoposide 100mg/m² IV infusion 2 and 3 or Etoposide 100mg/m² IV infusion 2 and 3 Etoposide 200mg/m2 PO Cycle frequency 21 days Number of cycles 4 - 6 cycles (usually 4) Administration Cisplatin is administered in 500mL sodium chloride 0.9% over 60 minutes following the pre and post hydration protocol below. Infusion Fluid & Additives Volume Infusion Time Sodium Chloride 0.9% 1000mL 1 hour Mannitol 20% 200mL 30 minutes OR Mannitol 10% 400mL 30 minutes Ensure urine output > 100mL / hour prior to giving cisplatin. Give a single dose of furosemide 20mg iv if necessary. Cisplatin 500mL 1 hour Sodium Chloride 0.9% + 2g MgSO4 + 1000mL 2 hours 20mmol KCl TOTAL 2700mL or 2900mL 4 hours 30 minutes Note: Patients with magnesium or potassium below the normal range should have 2g MgSO4 and 20mmol KCl added to the pre-hydration bag and the duration of the infusion increased to 2 hours. All patients must be advised to drink at least 2 litres of fluid over the following 24 hours. IV etoposide is administered in 1000mL sodium chloride 0.9% and infused over a minimum of 1 hour. Version 1 Review date June 2018 Page 1 of 4 Oral etoposide is available as 50mg and 100mg capsules.