ESC Guidelines on Diabetes, Pre-Diabetes And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Aug. 13 Vs. Phoenix.Indd
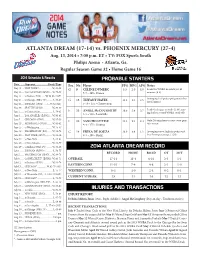
ATLANTA DREAM (17-14) vs. PHOENIX MERCURY (27-4) Aug. 13, 2014 • 7:00 p.m. ET • TV: FOX Sports South Philips Arena • Atlanta, Ga. Regular Season Game 32 • Home Game 16 2014 Schedule & Results PROBABLE STARTERS Date .........Opponent ....................Result/Time Pos. No. Player PPG RPG APG Notes May 11 .....NEW YORK^ .......................W, 63-58 G 9 CÉLINE DUMERC 3.3 2.0 4.0 Leads the WNBA in assists per 40 May 16 .....SAN ANTONIO (SPSO) ....W, 79-75 5-7 • 145 • France minutes (8.9) May 17 .....at Indiana (FSS) .......W, 90-88 (2OT) Averaging 15.9 points per game in her May 24 .....at Chicago (NBA TV) .......... L, 73-87 G 15 TIFFANY HAYES 13.2 3.0 2.6 last 15 games May 25 .....INDIANA (SPSO) ...... L, 77-82 (OT) 5-10 • 155 • Connecticut May 30 .....SEATTLE (SPSO) ................W, 80-69 F 35 ANGEL McCOUGHTRY 19.0 5.4 3.7 Leads the league in steals (2.48), aim- June 1 .......at Connecticut .......................L, 76-85 ing for her second WNBA steals title June 3 .......LOS ANGELES (ESPN2) ....W, 93-85 6-1 • 160 • Louisville June 7 .......CHICAGO (SPSO) ..............W, 97-59 F 20 SANCHO LYTTLE 12.4 9.2 2.4 Only Dream player to start every game June 13 .... MINNESOTA (SPSO) .........W, 85-82 6-4 • 175 • Houton this season June 15 .... at Washington ......................W, 75-67 June 18 .... WASHINGTON (FSS) ........W, 83-73 C 14 ERIKA DE SOUZA 13.9 8.9 1.2 Averaging career highs in points and June 20 .... NEW YORK (SPSO) ...........W, 85-64 6-5 • 190 • Brazil free throw percentage (.720) June 22 ... -

2006 WNBA Trading Cards Checklist
2006 WNBA Trading Cards Checklist Base Cards # Card Title [ ] 001 World Champions/Sacramento Monarchs Team Card [ ] 002 Lindsay Whalen (Connecticut Sun) [ ] 003 Tamika Whitmore (Indiana Fever) [ ] 004 Tangela Smith (Charlotte Sting) [ ] 005 Alana Beard (Washington Mystics) [ ] 006 Chicago Sky Team Card [ ] 007 Vickie Johnson (San Antonio Silver Stars) [ ] 008 Kelly Schumacher (New York Liberty) [ ] 009 Plenette Pierson (Detroit Shock) [ ] 010 Sheryl Swoopes (Houston Comets) [ ] 011 Los Angeles Sparks Team Card [ ] 012 Katie Douglas (Connecticut Sun) [ ] 013 Nicole Ohlde (Minnesota Lynx) [ ] 014 Anna DeForge (Indiana Fever) [ ] 015 Swin Cash (Detroit Shock) [ ] 016 Kelly Miller (Phoenix Mercury) [ ] 017 Kara Lawson (Sacramento Monarchs) [ ] 018 Shameka Christon (New York Liberty) [ ] 019 Dominique Canty (Houston Comets) [ ] 020 Sue Bird (Seattle Storm) [ ] 021 Detroit Shock Team Card [ ] 022 Margo Dydek (Connecticut Sun) [ ] 023 Shannon Johnson (San Antonio Silver Stars) [ ] 024 Chandi Jones (Minnesota Lynx) [ ] 025 Cheryl Ford (Detroit Shock) [ ] 026 Katie Feenstra (San Antonio Silver Stars) [ ] 027 Ashley Battle (New York Liberty) [ ] 028 Tammy Sutton-Brown (Charlotte Sting) [ ] 029 Deanna Jackson (Chicago Sky) [ ] 030 Yolanda Griffith (Sacramento Monarchs) [ ] 031 Minnesota Lynx Team Card [ ] 032 Asjha Jones (Connecticut Sun) [ ] 033 Nicole Powell (Sacramento Monarchs) [ ] 034 Sancho Lyttle (Houston Comets) [ ] 035 Nykesha Sales (Connecticut Sun) [ ] 036 LaToya Thomas (San Antonio Silver Stars) [ ] 037 Nikki Teasley (Washington Mystics) -

Complete Program
25th Topical Meeting of the International Society of Electrochemistry i Program of the 25th Topical Meeting of the International Society of Electrochemistry New electrochemical processes for energy and the environment 12-15 May 2019 Toledo, Spain Organized by: Division 5 Electrochemical Process Engineering and Technology Division 7 Physical Electrochemistry ISE Region Spain TY O CIE F EL O E S C L T A R N O C O I H T E A M N I R S E T T R Y N I • ii 25th Topical Meeting of the International Society of Electrochemistry International Society of Electrochemistry Chemin du Closelet 2 1006 Lausanne Switzerland Copyright © 2019 All rights reserved. No part of this work may be reproduced, stored in a retrieval system or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without prior written permission of the Publisher. No responsibility is assumed by the Publisher for any injury and/or damage to persons or property as a matter of product liability, negligence or otherwise, or from any use or operation of any methods, products, instructions or ideas contained in the material herein. Printed in Spain 25th Topical Meeting of the International Society of Electrochemistry iii Organizing Committee Karel Bouzek, UCT Prague, Czech Republic Angel Cuesta, University of Aberdeen, UK Enrique Herrero, University of Alicante, Spain (co-chair) François Lapicque, University of Lorraine, France Manuel A. Rodrigo, University of Castilla-La Mancha, Spain (co-chair) Mark Symes, University of Glasgow, UK Local -

2011 Atlanta Dream Roster
1 TABLE OF CONTENTS General Information WNBA Court Diagram …………………….103 Table of Contents . .2 MEDIA INFORMATION OPPONENTS 2010 Atlanta Dream Schedule . .3 Chicago Sky ……………………………..105 Quick Facts ……………… . ... 3 Connecticut Sun ………………………….105 General Media Information . …… 4 Indiana Fever …………………………….106 Los Angeles Sparks ……………………...106 DREAM FRONT OFFICE Minnesota Lynx ………………………….107 Office Directory …………………………….6 New York Liberty ………………………..107 Owner Bios ………………………………..7-8 Phoenix Mercury …………………………108 Front office Bios ………………………… 9-12 San Antonio Silver Stars …………………108 Seattle Storm ……………………………..109 MEET THE TEAM Tulsa Shock ………………………………110 Dream Roster & Pronunciations.……………14 Washington Mystics ……………………...110 Marynell Meadors ……………………….15-16 2010 Regular Season in Review …….111-116 Carol Ross …………………………………..17 Fred Williams ………………………………18 Sue Panek …………………………………..19 PHILIPS ARENA Kim Moseley ……………………………… 20 General Arena Information …………117-118 Seating and Ticket Information ………….119 Spotter‘s Chart ………………………………21 Dream Roster ………………………………..22 Alison Bales ………………………………23-24 Felicia Chester ……………………………….25 Iziane Castro Marques …………………..26-28 Erika De Souza ………………………….29-30 Lindsey Harding …………………………31-32 Sandora Irvin …………………………….33-34 Shalee Lehning ………………………….35-36 Sancho Lyttle ……………………………37-38 Angel McCoughtry ……………………...39-40 Shannon McCallum ………………………...41 Coco Miller ……………………………...42-44 Armintie Price …………………………..45-46 Brittainey Raven …………………………47-48 DREAM HISTORY Key Dates …………………………………50-51 All-Time Results ……………………………..52 Draft History ……………………………...53-54 All-Time Roster …………………………..55-57 All-Time Transactions ……………………57-59 2010 Season in Review …………………...60-61 2009 Season in Review …………..……….62-63 2008 Season in Review …………………...64-65 WNBA & QUICK FACTS WNBA Quick Facts ………………………67-73 WNBA Timeline …………………………73-87 2010 WNBA PR Contacts ……………….88-90 WNBA Award Winners ………………..91-101 2 SCHEDULE & QUICK FACTS 2011 Atlanta Dream Schedule ADDRESS: ATLANTA DREAM MAY 225 Peachtree Street NE 2011 PRESEASON Sun. -

2014 Seattle Storm Media Guide
1 StormBasketball.com TABLE OF CONTENTS 2014 Schedule ................................................................................................................................................4 Seattle Storm Front Office ...........................................................................................................................7 2014 Key Dates, KeyArena & Ticket Info ...................................................................................................8 WNBA Cares ...................................................................................................................................................9 Force 10 Hoops LLC .....................................................................................................................................11 2014 Storm Roster .........................................................................................................................................20-47 2013 In Review ................................................................................................................................................48-54 WNBA Info .......................................................................................................................................................55-141 Team History ....................................................................................................................................................142-184 WNBA Opponents .........................................................................................................................................185-208 -

ESC Guidelines on Diabetes, Pre-Diabetes, And
European Heart Journal (2013) 34, 3035–3087 ESC GUIDELINES doi:10.1093/eurheartj/eht108 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD The Task Force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD). Downloaded from Authors/Task Force Members: Lars Ryde´n* (ESC Chairperson) (Sweden), Peter J. Grant* (EASD Chairperson) (UK), Stefan D. Anker (Germany), Christian Berne (Sweden), Francesco Cosentino (Italy), Nicolas Danchin (France), Christi Deaton (UK), Javier Escaned (Spain), Hans-Peter Hammes (Germany), http://eurheartj.oxfordjournals.org/ Heikki Huikuri (Finland), Michel Marre (France), Nikolaus Marx (Germany), Linda Mellbin (Sweden), Jan Ostergren (Sweden), Carlo Patrono (Italy), Petar Seferovic (Serbia), Miguel Sousa Uva (Portugal), Marja-Riita Taskinen (Finland), Michal Tendera (Poland), Jaakko Tuomilehto (Finland), Paul Valensi (France), Jose Luis Zamorano (Spain) ESC Committee for Practice Guidelines (CPG): Jose Luis Zamorano (Chairperson) (Spain), Stephan Achenbach (Germany), Helmut Baumgartner (Germany), Jeroen J. Bax (Netherlands), He´ctor Bueno (Spain), Veronica Dean by guest on September 19, 2014 (France), Christi Deaton (UK), Çetin Erol (Turkey), Robert Fagard (Belgium), Roberto Ferrari (Italy), David Hasdai (Israel), Arno W. Hoes (Netherlands), Paulus Kirchhof (Germany UK), Juhani Knuuti (Finland), Philippe Kolh (Belgium), -
June 1998: NBA Draft Special
“Local name, national Perspective” $4.95 © Volume 4 Issue 8 1998 NBA Draft Special June 1998 BASKETBALL FOR THOUGHT by Kris Gardner, e-mail: [email protected] Garnett—$126 M; and so on. Whether I’m worth the money Lockout, Boycott, So What... or not, if someone offered me one of those contract salaries, ime is ticking by patrio- The I’d sign in a heart beat! (Right and July 1st is tism in owners Jim McIlvaine!) quickly ap- 1992 want a In order to compete with proaching. All when hard the rising costs, the owners signs point to the owners he salary cap raise the prices of the tickets. locking out the players wore with no Therefore, as long as people thereby delaying the start of the salary ex- buy the tickets, the prices will the free agent signing pe- Ameri- emptions continue to rise. Hell, real riod. As a result of the im- can similar to people can’t afford to attend pending lockout, the players flag the NFL’s games now; consequently, union has apparently de- draped salary cap corporations are buying the cided to have the 12 mem- over and the seats and filling the seats with bers selected to represent the his players suits. USA in this summer’s World Team © The players have wanted Championships in Greece ...the owners were rich when they entered the league and to get rid of the salary cap for boycott the games. Big deal there aren’t too many legal jobs where tall, athletic, and, in years and still maintain that and so what. -

NEW YORK LIBERTY Liberty Statistics Presented By
NEW YORK LIBERTY Liberty statistics presented by MEDIA CONTACT: Vincent Novicki | [email protected] | (212) 465-5962 | @nyliberty | #ShowUp 2017 SCHEDULE/RESULTS WNBA PLAYOFFS 2ND ROUND: NEW YORK LIBERTY VS. WASHINGTON MYSTICS MAY NEW YORK LIBERTY (0-0) PRESEASON vs. Tuesday, May 2 vs. Los Angeles W, 81-65 1-0 WASHINGTON MYSTICS (1-0) (at Mohegan Sun Arena) Wednesday, May 3 vs. Chicago L, 75-86 1-1 Sunday, Sept. 10 • 5:00 PM (EST) (at Mohegan Sun Arena) New York, N.Y. (Madison Square Garden) Sunday, May 7 CONNECTICUT L, 57-79 1-2 TV: ESPN2 (at Columbia University) TALE OF THE TAPE (*Regular Season Stats) REGULAR SEASON PPG OPP. PPG FG% OPP FG% 3PT% OPP 3PT% FT% RPG APG SPG TO BLK Saturday, May 13 SAN ANTONIO W, 73-64 1-0 NEW YORK 79.7 76.6 .425 .408 .332 .333 .779 38.7 16.7 6.1 13.1 3.9 Thursday, May 18 MINNESOTA (ESPN 2) L, 71-90 1-1 Tuesday, May 23 at Phoenix W, 69-67 2-1 WASHINGTON 81.7 81.0 .416 .432 .317 .365 .843 36.3 16.4 6.3 12.1 4.6 Friday, May 26 at Seattle L, 81-87 2-2 Tuesday, May 30 LOS ANGELES (ESPN 2) L, 75-90 2-3 NEW YORK LIBERTY PROBABLE STARTERS JUNE Friday, June 2 DALLAS W, 93-89 3-3 NO. NAME POS. HT. PPG RPG APG MPG College Sunday, June 4 PHOENIX W, 88-72 4-3 1 Shavonte Zellous G 5-10 11.7 4.0 2.8 29.1 Pittsburgh Wednesday, June 7 ATLANTA W, 76-61 5-3 Averaging career highs in both rebounding and assists; ranks 3rd on the Liberty in scoring Sunday, June 11 SEATTLE W, 94-86 6-3 Wednesday, June 14 at Connecticut L, 76-96 6-4 7 Kia Vaughn C 6-4 5.8 4.9 0.7 19.6 Rutgers Friday, June 16 at Dallas W, 102-93 (OT) 7-4 -

Denis Bobrakov About Business Principles, Life Rules and Personal
CORPORATE NEWSPAPER January, 2018 / № 9 DENIS BOBRAKOV ABOUT BUSINESS PRINCIPLES, LIFE RULES AND PERSONAL 02 NEW YEAR WITH NEW MEMBERS. LET’S GET ACQUIANTED! 06 FIRST CARGO IN 2018. THE FIRST DAY OF THE YEAR WILL STAND FOR THE WHOLE YEAR 11 BACK TO STUDENTS’ DAYS! COVER STORY KEEPING OLD TRADITIONS WE CREATE NEW ONES ACEXPress is issued since 2013. As time passed the number of readers has increased, the newspaper today is issued in the English and Russian languages and the number of pages as well as the number of ACEX Alliance members is growing. Five new companies joined the Alliance at the end of 2017. LET’S GET TO KNOW alongside with other Alliance members,” Dmitriy Sorokin, EACH OTHER Sales Director at Narva Logistics comments their Shipco Transport Saint Petersburg entering the Alliance. Advantages • Convenient location of the warehousing complex • 24 h cargo handling service Farasoobar Int’l, Iran The Company’s expertise is in sea freight (LCL) from the Saint Petersburg port in 290 directions. The deliveries are carried out on a weekly basis. Advantages • Convenient fixed schedule • 20 days payment delay Narva Logistics, Estonia The experts of the Iranian company offer freight forwarding via Iran to CIS, Afghanistan and Iraq and do multimodal shipments and project freight forwarding via Iran abroad and in the country. “The main reasons of joining several networks is presenting our country and introducing how Narva Logistics is a warehouse and logistics safe can be trade conditions in this sector of operator in the North-Eastern Estonia. Persian Gulf and Middle East and creating new “We entered ACEX not only because of the markets and demands in the region to encourage companys’ business development but because of the traders and partners to use this secured route,” advantageous cooperation for projects’ execution Farzad Saffarzadeh, CEO at Farasoobar Int’l 2 COVER STORY Forwarder & Shipping AG Global Logistics, Azerbaijan Agency comments on their joining the Alliance. -

2011 New York Liberty Media Guide (.Pdf)
~ 2 ~ TABLE OF CONTENTS WNBA Key Dates 2005 Game-by-Game Results Media Guidelines 2006 Game-by-Game Results 2011 New York Liberty Staff Directory 2007 Game-by-Game Results 2008 Game-by-Game Results Executive Management 2009 Game-by-Game Results James Dolan 2009 Game-by-Game Results Hank J. Ratner 2010 Game-by-Game Results Scott O’Neil Year-by-Year Results Franchise Leaders Basketball Operations Seasonal Leaders John Whisenant Opening Night Rosters Jill Culbertson All-Time Highs/Lows Monique Ambers All-Time Highs/Lows at MSG Lady Grooms All-Time Highs/Lows on the Road Lisa White Single Game Bests Lisa Callahan All-Time Liberty Playoff History Dr. Jo Hannafin All-Time Team Playoff Records Dr. Marci Goolsby All-Time Individual Playoffs Records MSG Training Center Playoff Franchise Leaders 2011 New York Liberty Players WNBA 2011 Roster History of the WNBA Essence Carson 2011 WNBA PR Contacts Quanitra Hollingsworth 2010 Final Standings Leilani Mitchell 2010 WNBA Stats Leaders Plenette Pierson Year-by-Year vs. Opponents Cappie Pondexter All Teams Nicole Powell Sidney Spencer In the Community Kia Vaughn Garden of Dreams Jessica Breland Maddie Sydney Colson Dance Teams Alex Montgomery WNBA in the Community 2010 Season in Review The World’s Most Famous Arena 2010 Game-by-Game Recaps Madison Square Garden History 2010 Team Highs/Lows MSG Network 2010 Individual Highs Prudential Center Seating Chart 2010 Final Team Statistics 2010 Win/Loss Breakdown 2010 Miscellaneous Statistics Editors All-Time New York Liberty History Stacey Escudero; Ashley-Simone -

KAPLAN CONSTRUCTION SPECIAL from 5 P.M
The Battalion PORTS Wednesday *June 18,191 through August, with the winners of have won Olympic gold medals. The WNBA team rosters WNBA team rosters the Eastern and Western conferences ABL, on the other hand, limits each team Eastern Conference Western Conference Preview and the two teams with the next best to two foreign-born players. Charlotte Sting Los Angeles Sparks Continued from Page 3 records advancing to single-elimina “The WNBA has the best players No. Name Pos. Ht. College No. Name College tion playoff games. from around the world,” Ackerman Katasha Artis F 6-0 Northeastern ’95 42 Linda Burgess bama '92 55 Michi Atkins Texas Tech ’96 32 Daedra Charles nnessee '91 “I think (the WNBA) is going to The league features Olympians and said. “These women have been play 23 Vicky Bullett Maryland ’89 12 Katrina Colleton land '93 3 Andrea Congre£iy|||i' . Mercer '92/Great Britian 21 Tamecka Dixon^ is'97 50 Sharon ManniQ^om^1 work and work well,” he said. “If I was ing in obscurity overseas. People’s N.C. State '91 34 Travesa GanJ, tar '94 spending sports marketing bucks it 51 Rhonda Mapp N.C. State '92 9 Lisa Leslii heads will turn when they see the skill 32 Andrea Stinson N.C. State '91 4 Mwadi Mai ^ ^ If I was spending Tora Super J. Virginia '97 11 Penny Tolei*^ Long Beach State • would be in women’s professional of these women.” - Berkeley ’93/Yugoslavia Milica Vukadii 10 Jamila Wideman Stanford '97 basketball.” Indeed. The WNBA game will be Debra Williams Louisiana Tech '96 28 Zheng Haixia ‘ ’‘’’SS&.'xPI&B China Head coach - Marynell Meadors The year-old ABL, operating with played at a level that will shock fans, Head coach - Linda Sharp Cleveland Rockers much less TV exposure and corporate sports marketing Phoenix Mercury with an up-tempo, physical style like Name Pos. -

2018 Atlanta Dream Media Guide 2 2018 ATLANTA DREAM SCHEDULE
1 @AtlantaDream 2018 Atlanta Dream Media Guide 2 2018 ATLANTA DREAM SCHEDULE Sun, May 20 at Dallas Arlington, Texas 3:00 p.m. Twitter Wed, May 23 at Chicago Chicago, Ill. 12:00 p.m. Sat, May 26 Dallas McCamish Pavilion 6:00 p.m. FSSE Tues, May 29 Minnesota McCamish Pavilion 7:00 p.m. Twitter Sun, June 3 Phoenix McCamish Pavilion 3:00 p.m. FSSE Tues, June 5 Connecticut McCamish Pavilion 8:00 p.m. FSSO Fri, June 8 at Las Vegas Las Vegas, Nev. 3:00 p.m. Sun, June 10 at Seattle Seattle, Wash. 7:00 p.m. Tues, June 12 at Los Angeles Los Angeles, Calif. 10:30 p.m. Thurs, June 14 Indiana McCamish Pavilion 11:30 a.m. FSSO/NBATV Sat, June 16 at Indiana Indianapolis, Ind. 7:00 p.m. Tues, June 19 at New York White Plains, NY 7:00 p.m. Fri, June 22 Connecticut McCamish Pavilion 7:00 p.m. FSSE Wed, June 27 at Chicago Chicago, Ill. 12:00 p.m. Fri, June 29 at Minnesota Minneapolis, Minn. 8:00 p.m. NBATV Sun, July 1 at Indiana Indianapolis, Ind. 5:00 p.m. Fri, July 6 Seattle McCamish Pavilion 7:00 p.m. FSSE Sun, July 8 Phoenix McCamish Pavilion 3:00 p.m. FSSE Wed, July 11 at Washington Washington, D.C. 11:30 a.m. Fri, July 13 Indiana McCamish Pavilion 7:00 p.m. FSSE Sun, July 15 Washington McCamish Pavilion 3:00 p.m. FSSE Tues, July 17 at Connecticut Uncasville, Conn.