Introduction to Paediatric Dentistry 9-3-2020.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pediatric Oral Pathology. Soft Tissue and Periodontal Conditions
PEDIATRIC ORAL HEALTH 0031-3955100 $15.00 + .OO PEDIATRIC ORAL PATHOLOGY Soft Tissue and Periodontal Conditions Jayne E. Delaney, DDS, MSD, and Martha Ann Keels, DDS, PhD Parents often are concerned with “lumps and bumps” that appear in the mouths of children. Pediatricians should be able to distinguish the normal clinical appearance of the intraoral tissues in children from gingivitis, periodontal abnormalities, and oral lesions. Recognizing early primary tooth mobility or early primary tooth loss is critical because these dental findings may be indicative of a severe underlying medical illness. Diagnostic criteria and .treatment recommendations are reviewed for many commonly encountered oral conditions. INTRAORAL SOFT-TISSUE ABNORMALITIES Congenital Lesions Ankyloglossia Ankyloglossia, or “tongue-tied,” is a common congenital condition characterized by an abnormally short lingual frenum and the inability to extend the tongue. The frenum may lengthen with growth to produce normal function. If the extent of the ankyloglossia is severe, speech may be affected, mandating speech therapy or surgical correction. If a child is able to extend his or her tongue sufficiently far to moisten the lower lip, then a frenectomy usually is not indicated (Fig. 1). From Private Practice, Waldorf, Maryland (JED); and Department of Pediatrics, Division of Pediatric Dentistry, Duke Children’s Hospital, Duke University Medical Center, Durham, North Carolina (MAK) ~~ ~ ~ ~ ~ ~ ~ PEDIATRIC CLINICS OF NORTH AMERICA VOLUME 47 * NUMBER 5 OCTOBER 2000 1125 1126 DELANEY & KEELS Figure 1. A, Short lingual frenum in a 4-year-old child. B, Child demonstrating the ability to lick his lower lip. Developmental Lesions Geographic Tongue Benign migratory glossitis, or geographic tongue, is a common finding during routine clinical examination of children. -

6 Development of the Teeth: Root and Supporting Structures Nagat M
AVERY Chap.06 27-11-2002 10:09 Pagina 108 108 II Development of the Teeth and Supporting Structures 6 Development of the Teeth: Root and Supporting Structures Nagat M. ElNesr and James K. Avery Chapter Outline Introduction Introduction... 108 Objectives... 108 Root development is initiated through the contributions Root Sheath Development... 109 of the cells originating from the enamel organ, dental Single-Root Formation... 110 papilla, and dental follicle. The cells of the outer enamel Multiple-Root Formation... 111 epithelium contact the inner enamel epithelium at the Root Formation Anomalies... 112 base of the enamel organ, the cervical loop (Figs. 6.1 and Fate of the Epithelial Root Sheath (Hertwig's Sheath)... 113 6.2A). Later, with crown completion, the cells of the cer- Dental Follicle... 114 vical loop continue to grow away from the crown and Development of (Intermediate) Cementum... 116 become root sheath cells (Figs. 6.2B and 6.3). The inner Cellular and Acellular Cementum... 116 root sheath cells cause root formation by inducing the Development of the Periodontal Ligament... 117 adjacent cells of the dental papilla to become odonto- Development of the Alveolar Process... 119 blasts, which in turn will form root dentin. The root Summary... 121 sheath will further dictate whether the tooth will have Self-Evaluation Review... 122 single or multiple roots. The remainder of the cells of the dental papilla will then become the cells of the root pulp.The third compo- nent in root formation, the dental follicle, is the tissue that surrounds the enamel organ, the dental papilla, and the root. -

Lecture 2 – Bone
Oral Histology Summary Notes Enoch Ng Lecture 2 – Bone - Protection of brain, lungs, other internal organs - Structural support for heart, lungs, and marrow - Attachment sites for muscles - Mineral reservoir for calcium (99% of body’s) and phosphorous (85% of body’s) - Trap for dangerous minerals (ex:// lead) - Transduction of sound - Endocrine organ (osteocalcin regulates insulin signaling, glucose metabolism, and fat mass) Structure - Compact/Cortical o Diaphysis of long bone, “envelope” of cuboid bones (vertebrae) o 10% porosity, 70-80% calcified (4x mass of trabecular bone) o Protective, subject to bending/torsion/compressive forces o Has Haversian system structure - Trabecular/Cancellous o Metaphysis and epiphysis of long bone, cuboid bone o 3D branching lattice formed along areas of mechanical stress o 50-90% porosity, 15-25% calcified (1/4 mass of compact bone) o High surface area high cellular activity (has marrow) o Metabolic turnover 8x greater than cortical bone o Subject to compressive forces o Trabeculae lined with endosteum (contains osteoprogenitors, osteoblasts, osteoclasts) - Woven Bone o Immature/primitive, rapidly growing . Normally – embryos, newborns, fracture calluses, metaphyseal region of bone . Abnormally – tumors, osteogenesis imperfecta, Pagetic bone o Disorganized, no uniform orientation of collagen fibers, coarse fibers, cells randomly arranged, varying mineral content, isotropic mechanical behavior (behavior the same no matter direction of applied force) - Lamellar Bone o Mature bone, remodeling of woven -

Effect of Posters and Mobile-Health Education Strategies on Teething Beliefs and Oral Health Knowledge Among Mothers in Nairobi
EFFECT OF POSTERS AND MOBILE-HEALTH EDUCATION STRATEGIES ON TEETHING BELIEFS AND ORAL HEALTH KNOWLEDGE AMONG MOTHERS IN NAIROBI. DR. REGINA MUTAVE JAMES REGISTRATION NUMBER: V91/96427/2014 Department of Periodontology/Community and Preventive Dentistry THESIS SUBMITTED IN FULFILMENT OF THE DOCTOR OF PHILOSOPHY DEGREE (PhD) IN COMMUNITY AND PREVENTIVE DENTISTRY, UNIVERSITY OF NAIROBI DECLARATION: I, Regina Mutave James hereby declare that this is my original work and that it has not been submitted by any other person for research purpose, degree or otherwise in any other university or institution. Signed ………………………………………. Date ………………………………. Regina Mutave James R.M.J PhD Thesis - 2015 Page i SUPERVISORS’ DECLARATION This research thesis has been submitted for the fulfillment of the requirement for the award of PhD in Community and Preventive Dentistry with our approval as supervisors. Supervisors: Signed ………………………………..Date……………………………. Prof. Loice W. Gathece BDS., MPH., PhD( Nbi). Department of Periodontology/ Community and Preventive Dentistry, University of Nairobi. Signed ………………………………..Date……………………………. Prof. Arthur M. Kemoli BDS (Nbi)., MSc (UvA)., PhD (UvA). Department of Pediatric Dentistry and Orthodontics, University of Nairobi. R.M.J PhD Thesis - 2015 Page ii DEDICATION To the Almighty, for His unending Grace! R.M.J PhD Thesis - 2015 Page iii ACKNOWLEDGEMENTS My PhD studies including this thesis were made possible by the financial support that I received from the University of Nairobi, and I am grateful for the opportunity. I wish to thank my supervisors Prof. Loice Gathece and Prof Arthur Kemoli who were always there to offer guidance and encouragement throughout the process. My sincere appreciation for my family and friends who stood by me even when I had no time for them and especially my children Erick, Aileen, Mbithe and Jynette. -

A Global Compendium of Oral Health
A Global Compendium of Oral Health A Global Compendium of Oral Health: Tooth Eruption and Hard Dental Tissue Anomalies Edited by Morenike Oluwatoyin Folayan A Global Compendium of Oral Health: Tooth Eruption and Hard Dental Tissue Anomalies Edited by Morenike Oluwatoyin Folayan This book first published 2019 Cambridge Scholars Publishing Lady Stephenson Library, Newcastle upon Tyne, NE6 2PA, UK British Library Cataloguing in Publication Data A catalogue record for this book is available from the British Library Copyright © 2019 by Morenike Oluwatoyin Folayan and contributors All rights for this book reserved. No part of this book may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior permission of the copyright owner. ISBN (10): 1-5275-3691-2 ISBN (13): 978-1-5275-3691-3 TABLE OF CONTENTS Foreword .................................................................................................. viii Introduction ................................................................................................. 1 Dental Development: Anthropological Perspectives ................................. 31 Temitope A. Esan and Lynne A. Schepartz Belarus ....................................................................................................... 48 Natallia Shakavets, Alexander Yatzuk, Klavdia Gorbacheva and Nadezhda Chernyavskaya Bangladesh ............................................................................................... -

Developmental Biology of Cementum
Int. J. Dev. Biol. 45: 695-706 (2001) Review Developmental Biology of Cementum THOMAS G.H. DIEKWISCH* Allan G. Brodie Laboratory for Craniofacial Genetics, University of Illinois at Chicago, USA CONTENTS Origins of cementum - a scientific "whodunit" ........................................................................695 Loss of ameloblast continuity and insertion of mesenchymal cells from the dental follicle proper ................................................................................................697 Initial cementum matrix deposition by mesenchymal cells in proximity to non-secretory epithelial cells ...................................................................................699 Cementogenesis at the tooth cervix and at the cemento-enamel junction .............................700 Early removal of HERS from the root surface in humans as seen in the Gottlieb collection ..............................................................................................701 Role of amelogenins in cementogenesis ................................................................................702 Possible mechanism of cementoblast induction .....................................................................704 Summary ................................................................................................................................704 KEY WORDS: Cementum, Hertwig’s epithelial root sheath, Gottlieb, amelogenin, periodontium Tooth cementum is a bone-like mineralized tissue secreted by Origins of cementum - a scientific -

Initiation to Eruption
Head and Neck embryology Tooth Development Review head and neckblk embryology Initiation to eruption Skip Review Initiation Initiation stomodeum Epithelial cells (dental lamina) During 6th week, ectoderm in stomodeum forms horseshoe shaped mass of oral epithelium mesenchyme Basement membrane mesenchyme Initiation of anterior primary teeth Epithelial cells in horseshoe Dental lamina begins begins the sixth to seventh week form dental lamina growing into mesenchyme of development, initiation of additional At site where tooth will be teeth follows and continues for years Dental Lamina – Initiation Supernumerary tooth PREDICT what would happen if an extra tooth was initiated. Mesiodens 1 Bud Stage – eighth week Bud Stage Epithelium (dental Lamina) Dental lamina grows down into mesenchyme at site of tooth. Mesenchyme starts to change composition in response mesenchyme PREDICT what would happen if two tooth buds fused together or one tooth bud split in half. Fusion/Gemination Cap stage – week 9 By week 9, all germ layers of future tooth have formed ElEnamel organ (ename ll)l only) Dental papilla (dentin and pulp) Fusion Gemination Dental sac (cementum, PDL, Alveolar bone) PREDICT how you would know if it was mesenchyme fusion or gemination Cap Stage Successional Dental Lamina Each primary tooth germ has epithelium a successional lamina that becomes a permanent tooth Succedaneous teeth replace a deciduous tooth, nonsuccedaneous do not IDENTIFY nonsuccedaneous teeth mesenchyme PREDICT What occurs if no successional lamina forms? 2 Congenitally -

QUICK ORAL HEALTH FACTS ABOUT the YOUNG Dr Ng Jing Jing, Dr Wong Mun Loke
ORAL health IN PRIMARY CARE UNIT NO. 2 QUICK ORAL HEALTH FACTS ABOUT THE YOUNG Dr Ng Jing Jing, Dr Wong Mun Loke ABSTRACT Table 1. Eruption sequence of Primary Dentition This article sheds light on the sequence of teeth eruption Primary Upper Teeth Primary Lower Teeth in the young and teething problems; highlights the importance and functions of the primary dentition and Central Incisors: 8-13 months Central Incisors: 6-10 months provides a quick overview of common developmental Lateral Incisors: 8-13 months Lateral Incisors: 10-16 months dental anomalies and other dental conditions in Canines: 16-23 months Canines: 16-23 months children. First Molars: 16-23 months First Molars: 13-19 months Second Molars: 25-33 months Second Molars: 23-31 months SFP2011; 37(1) Supplement : 10-13 Table 2. Eruption sequence of Adult Dentition Adult Upper Teeth Adult Lower Teeth INTRODUCTION Central Incisors: 7-8 years Central Incisors: 6-7 years The early years are always full of exciting moments as we observe Lateral Incisors: 8-9 years Lateral Incisors: 7-8 years our children grow and develop. One of the most noticeable Canines: 11-12 years Canines: 9-10 years aspects of their growth and development is the eruption of First Premolars: 10-11 years First Premolars: 10-11 years teeth. The first sign of a tooth in the mouth never fails to Second Premolars: 11-12 years Second Premolars: 11-12 years attract the attention of the parent and child. For the parent, it First Molars: 6-7 years First Molars: 6-7 years marks an important developmental milestone of the child but Second Molars: 12-13 years Second Molars: 11-13 years for the child, it can be a source of irritation brought on by the Third Molars: 18-25 years Third Molars: 18-25 years whole process of teething. -

172-173 Harada.Pmd
International symposium of Maxillofacial & Oral Regenerative Biology in Okayama 2005 Cell dynamics in the Growth and Differentiation of Dental Epithelium during Tooth Development: Stratum Intermedium Cells Originated From Inner Enamel Epithelium Hidemitsu Harada Department of Oral Anatomy & Developmental Biology, Osaka University Graduate School of Dentistry 1-8, Yamadaoka, Suita, Osaka 565-0871, Japan Abstract:The stratum intermedium develops as flattened cell layer on the proximal side of the ameloblast layer during the bell stage of tooth development. Stratum intermedium cells strongly express alkaline phosphatase (ALP) activity and have been considered to play a complementary role in the enamel mineralization, however the origin and/or the role of these cells have not been elucidated. In the present study, we focused on the lineage of stratum intermedium cells in continuously growing rodent incisors and analyzed it by using DiI tracers experiment and using the incisors organ culture. The results indicated that some stratum intermedium cells were originated from the inner enamel epithelium. Immunohistochemical and in situ hybridization studies showed that the stratum intermedium cells expressed the Notch-1, Notch-2, and Hes1, while the inner enamel epithelium and ameloblasts expressed their ligands Jagged-1. Furthermore, we examined th role of Notch signaling in the development of the stratum intermedium cells by use of the dental epithelial cell line, HAT-7. Recombinant Jagged1 protein enhanced the appearance of the stratum intermedium cells in HAT-7.On the other hand, anti-sense Notch1 decreased the number of stratum intermedium cells.Taken together, we propose a hypothesis that the lineage of the stratum intermedium differentiates from the ameloblasts lineage through Notch signaling. -
AIPET Syllabus for Periodontology – Paper – II
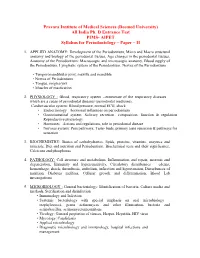
Pravara Institute of Medical Sciences (Deemed University) All India Ph. D Entrance Test PIMS- AIPET Syllabus for Periodontology – Paper – II 1. APPLIED ANATOMY: Development of the Periodontium, Micro and Macro structural anatomy and biology of the periodontal tissues, Age changes in the periodontal tissues, Anatomy of the Periodontium: Macroscopic and microscopic anatomy, Blood supply of the Periodontium, Lymphatic system of the Periodontium, Nerves of the Periodontium • Temporomandibular joint, maxilla and mandible • Nerves of Periodontium. • Tongue, oropharynx • Muscles of mastication 2. PHYSIOLOGY : Blood, respiratory system --enumerate of the respiratory diseases which are a cause of periodontal diseases (periodontal medicine), Cardiovascular system: Blood pressure, normal ECG, shock • Endocrinology—hormonal influences on periodontium • Gastrointestinal system: Salivary secretion—composition, function & regulation Reproductive physiology • Hormones –Actions and regulations, role in periodontal disease • Nervous system: Pain pathways, Taste- buds, primary taste sensation & pathways for sensation 3. BIOCHEMISTRY: Basics of carbohydrartes, lipids, proteins, vitamins, enzymes and minerals, Diet and nutrition and Periodontium, Biochemical tests and their significance, Calcicum and phosphorus 4. PATHOLOGY: Cell structure and metabolism, Inflammation and repair, necrosis and degeneration, Immunity and hypersensitivity, Circulatory disturbances – edema, hemorrhage, shock, thrombosis, embolism, infarction and hypertension, Disturbances of -

AMELOGENSIS Mean the Process of Production & Development (Mineralization) of Enamel, and Begins When the Crown Is Forming During the Bell Stage of Tooth Development
Lec. 6 Dr. Ali H. Murad AMELOGENSIS Mean the process of production & development (mineralization) of enamel, and begins when the crown is forming during the bell stage of tooth development. A- Life cycle of the ameloblast: The life span of the cells of the inner enamel epithelium can be divided into six stages. 1-morphogenic stage: the inner enamel epithelium interacts with the adjacent mesenchymal cells of dental papillae, determining the shape of the dentinioenamel junction & the crown. During this morphogenic stage the cells are short columnar, with large oval nuclei. Terminal bars appear represent points of close contact between cells. The inner enamel epithelium is separated from the C.T of dental papillae by basal lamina. 2-organizing stage: the inner enamel epithelium cells become longer & come into close contact with C.T. cells of the pulp which differentiate into odontoblasts. The 1st appearance of dentin is a critical phase in the life cycle of the inner enamel epithelium as it’s in contact with the C.T. of dental papillae; it receives nutrient material from the blood vessels of this tissue. When dentin forms, it cuts off the ameloblasts from their original source of nourishment, then they are supplied by the capillaries that surround & penetrate the outer enamel epithelium. 3-formative stage: the ameloblasts enter their formative stage after the 1st layer of dentin has been formed. During formation of the enamel matrix the ameloblasts retain the same length & arrangement. The earliest change is the development of cell process on the ameloblast surface, which penetrate the predentin & known as Tome’s processes. -

It's Only Teething…
OPINION personal view It’s only teething… A report of the myths and modern approaches to teething M. P. Ashley1 Paediatric dentistry is not my usual field of work. I am now based ter, come off best’. Gastrointestinal disorders and contamination of foodstuffs were more almost entirely in restorative dentistry and it is five years since I frequent in the summer. worked in the dental department of a children’s hospital. An essay In medieval times, animal substances on teething would appear to be an unusual choice of topic. With the were still being rubbed into the gums and current professional climate of ‘general professional education’ and teething infants were encouraged to chew ‘lifelong learning’ I can easily justify my time and effort studying a on hard objects such as roots. In 1429, Von Louffenberg, a German priest, summarised subject somewhat removed from my regular work. However, to be the care of a teething baby. completely honest, I have reached that age when many of my ‘Now when your baby’s teeth appear, you friends, relatives and colleagues are enjoying the sleepless nights must of these take prudent care. that accompany expanding families. Add to this the fact that I have For teething comes with grievous pain, so recently married into a family of midwives, health visitors, nurses to my word take heed again. When now the teeth are pushing and new mothers. I was not sure that I was giving the best, most up through, to rub the gums thou thus shall to date advice when asked about teething.