Drug Formulary 2019
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medicaid) Enhanced Care Plus (HARP) 2021 Drug Formulary Emblemhealth Enhanced Care and Enhanced Care Plus Formulary 2021 Formulary (List of Covered Drugs
Enhanced Care (Medicaid) Enhanced Care Plus (HARP) 2021 Drug Formulary EmblemHealth Enhanced Care and Enhanced Care Plus Formulary 2021 Formulary (List of Covered Drugs) PLEASE READ: THIS DOCUMENT CONTAINS INFORMATION ABOUT some of the drugs covered by your plan. When this drug list (formulary) refers to “we,” “us,” or “our,” it means EmblemHealth. When it refers to “plan” or “our plan,” it means EmblemHealth Enhanced Care (Medicaid) or Enhanced Care Plus (HARP). This document includes a list of the drugs (formulary) for our plan which is current as of 10/1/2021. For a complete updated formulary, please call Customer Service at 888-447-7364 (TTY: 711). Our hours are 8 am to 6 pm, Monday through Friday and 10 am to 1 pm, Saturday and Sunday. A representative will be happy to help. You can also check our website at emblemhealth.com. You must use network pharmacies to use your prescription drug benefit. The formulary and pharmacy network may change. Effective Oct. 1, 2021, New York State Medicaid will implement a single statewide Medication Assisted Treatment (MAT) formulary for opioid dependence agents and opioid antagonists. i EMBLEMHEALTH ENHANCED CARE AND ENHANCED CARE PLUS FORMULARY What is the EmblemHealth Enhanced Care and Enhanced Care Plus Formulary? A formulary is a list of covered drugs selected by our plan with help from a team of health care professionals. It represents the prescription therapies believed to be a necessary part of a quality treatment program. Our plan will cover the drugs listed in our formulary as long as the drug is medically necessary, the prescription is filled at a plan network pharmacy, and other plan rules are followed. -

OTC Brand Name Extensions Joseph A
University of the Pacific Scholarly Commons School of Pharmacy and Health Sciences Faculty Thomas J. Long School of Pharmacy and Health Articles Sciences 6-1-2004 OTC Brand Name Extensions Joseph A. Woelfel University of the Pacific, [email protected] Follow this and additional works at: https://scholarlycommons.pacific.edu/phs-facarticles Part of the Pharmacy and Pharmaceutical Sciences Commons Recommended Citation Woelfel, J. A. (2004). OTC Brand Name Extensions. Pharmacist’s Letter & Prescriber’s Letter, 20(6), 1–5. https://scholarlycommons.pacific.edu/phs-facarticles/72 This Article is brought to you for free and open access by the Thomas J. Long School of Pharmacy and Health Sciences at Scholarly Commons. It has been accepted for inclusion in School of Pharmacy and Health Sciences Faculty Articles by an authorized administrator of Scholarly Commons. For more information, please contact [email protected]. ® Detail-Document #200613 −This Detail-Document accompanies the related article published in− ® PHARMACIST’S LETTER / PRESCRIBER’S LETTER June 2004 ~ Volume 20 ~ Number 200613 OTC Brand Name Extensions Some Selected Expected Primary Actual Primary Ingredients Nonprescription Ingredient Product Lines Examples of U.S. Brand Name Extensions Alka-Seltzer4,5 Aspirin There are many different Alka-Seltzer products. Alka-Seltzer Original, Lemon Lime, and Extra Strength all contain aspirin. Alka-Seltzer Morning Relief contains aspirin plus caffeine. Alka-Seltzer PM contains aspirin plus diphenhydramine. The following products contain acetaminophen with other ingredients but no aspirin: Alka-Seltzer Plus Cold Effervescent Tablets and Liqui-Gels, Alka-Seltzer Plus Cold & Sinus, Alka-Seltzer Plus Night-Time Cold Effervescent Tablets and Liqui-Gels, Alka-Seltzer Plus Cold and Cough Liqui-Gels, and Alka-Seltzer Plus Nose and Throat. -

Over the Counter Medications After Kidney Donation
OVER THE COUNTER MEDICATIONS AFTER KIDNEY DONATION • Check this list before taking any over the counter medicine and take it as directed on the package • You may use the store-brand product instead of the brand names listed below (make sure active ingredients match) • This list does not include every over the counter product. • Call the transplant pharmacist or transplant team if you would like to take a medicine that is not on this list or if you have a question about any medicine Symptom Safe NOT Safe without transplant team ok • Constipation Senokot (senna) plain or –S • Colace (docusate) Fleets phospho-soda Increase the fluids and fiber (bran, • Miralax Fleet enema fresh fruits & vegetables) in your diet • Dulcolax (bisacodyl) Diarrhea Increase your fluid intake. • Imodium (loperamide) Notify your doctor for diarrhea lasting more than 2 days • Tylenol (acetaminophen)* • Non-aspirin pain-reliever* NSAIDs (non-steroidal anti-inflammatory drugs) *Do not take more than 3000 mg in such as: Headache, 24 hours (6 extra strength or 9 Advil, Motrin (Ibuprofen) Muscle Ache, regular strength pills) Aleve (Naproxen) Other Aches & Pains Nuprin • Voltaren Notify your doctor immediately if you Excedrin® • Midol have a fever with your headache Aspirin (ok to take once a day for heart, can cause stomach Cataflam (diclofenac) ulcers if used for pain) Orudis (ketoprofen) • Ben-Gay Not safe if you take blood pressure Not safe for ANY • Coricidin HBP medicine or have Allergy/Cold kidney donors • Mucinex (plain & DM) borderline high blood • Robitussin -

Witches Every Month? the Social Construction of Premenstrual Syndrome
Western Michigan University ScholarWorks at WMU Master's Theses Graduate College 4-1990 Witches Every Month? The Social Construction of Premenstrual Syndrome Suzanne Latham Follow this and additional works at: https://scholarworks.wmich.edu/masters_theses Part of the Sociology Commons Recommended Citation Latham, Suzanne, "Witches Every Month? The Social Construction of Premenstrual Syndrome" (1990). Master's Theses. 1034. https://scholarworks.wmich.edu/masters_theses/1034 This Masters Thesis-Open Access is brought to you for free and open access by the Graduate College at ScholarWorks at WMU. It has been accepted for inclusion in Master's Theses by an authorized administrator of ScholarWorks at WMU. For more information, please contact [email protected]. WITCHES EVERY MONTH? THE SOCIAL CONSTRUCTION OF PREMENSTRUAL SYNDROME by Suzanne Latham A Thesis Submitted to the Faculty of The Graduate College in partial fulfillment of the requirements for the Degree of Master of Arts Department of Sociology Western Michigan University Kalamazoo, Michigan April 1990 Reproduced with permission of the copyright owner. Further reproduction prohibited without permission. ACKNOWLEDGEMENTS I had no idea before beginning this thesis how arduous the project would be. Without the help and support of a few key people in my life, I doubt I would have been able to finish on time, if at all. So, at this point, I want to thank these people for their encouragement and let them know their support was appreciated. I would like to thank Karen Rice, who not only typed my thesis, but also acted as an editor and advisor in the process. I wish to thank my family for having the courage to ask me over and over, "How is the thesis coming?" Thank you to my committee members, James Petersen and Ronald Kramer, who gave me their views on the subject, but didn't insist that I take them. -

Pain Drug Comparison Chart Karen Pantazis, M.D
Information provided by Sutter Health’s MyLifeStages and pain management specialist Pain Drug Comparison Chart Karen Pantazis, M.D. Painkillers are among the most commonly used drugs in the United States. Deciding which to use deserves careful consideration. Use this quick comparison chart to COMMON SENSE help guide a conversation with your doctor about which CONSIDERATIONS medications are best and safest for you. • Talk with your doctor about medication dosage and possible contraindications. • Never take any drugs when you are pregnant without first consulting your doctor. • Exercise caution with sensitive groups such as children, the elderly and those with serious health conditions. OVER THE COUNTER Classification Brand Name Generic Name Best Used For Common Side Effects Warnings Bayer Aspirin Minor aches and pains, fever • GI bleeding • May contribute to Bufferin reduction and • Increased bleeding macular degeneration anti-inflammatory • Ulcers • Risk of Reyes syndrome in children Ascriptin and teens Aspirin Ecotrin • Do not combine with blood thinner Family St. Joseph’s medication • Can cause tinnitus in high doses • Can cause kidney problems Tylenol Acetaminophen Pain and fever • Itching/swelling • Liver damage possible if you take Excedrin reduction (especially of the face/ more than recommended dose or you tongue/throat) drink alcohol. Acetaminophen • Rash • OTC cough and flu products contain • Dizziness acetaminophen. It can add up quickly. • Bloody stools Limit total dose per day to 2000 mg. • Stomach bleeding Advil Ibuprofen, -
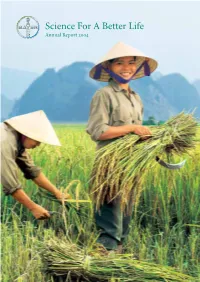
Bayer Annual Report 2004
Science For A Better Life Annual Report Bayer Group Key Data Bayer Annual Report 2004 Bayer Group 2003 2004 Change € million in % Net sales 28,567 29,758 + 4.2 EBITDA1) 3,616 4,130 + 14.2 Operating result [EBIT] (1,119) 1,808 • Income (loss) before income taxes (1,994) 985 • Net income (loss) (1,361) 603 • Gross cash flow2) 2,864 3,210 + 12.1 Net cash flow3) 3,293 2,450 – 25.6 Stockholders’ equity 12,213 12,268 + 0.5 Total assets 37,445 37,804 + 1.0 Capital expenditures 1,739 1,275 – 26.7 Employees at year end 115,400 113,000 – 2.1 Personnel expenses 7,906 7,306 – 7.6 Research and development expenses 2,404 2,107 – 12.4 Bayer AG 2003 2004 Change in % Total dividend payment in € million 365 402 + 10.1 Dividend per share in € 0.50 0.55 + 10.0 1) EBITDA = operating result (EBIT) plus depreciation and amortization 2) Gross cash flow = operating result (EBIT) plus depreciation and amortization, minus income taxes, minus gains/plus losses on retirements of noncurrent assets, plus/minus changes in pension provisions 3) Net cash flow = cash flow from operating activities according to IAS 7 Ten-Year Financial Summary Bayer Annual Report 2004 Bayer Group 1995 1996 1997 1998 1999 € million Net sales 22,793 24,853 28,124 28,062 27,320 Sales outside Germany 80.5% 82.2% 83.9% 83.6% 84.3% Sales of foreign consolidated companies 63.4% 65.4% 67.0% 67.5% 68.3% Operating result [EBIT] 2,102 2,306 3,077 3,155 3,357 Income (loss) before income taxes 2,140 2,282 2,611 2,728 2,836 Income (loss) after taxes 1,238 1,405 1,509 1,615 2,018 Noncurrent assets 9,437 -
Bayer Aktiengesellschaft
SECURITIES AND EXCHANGE COMMISSION FORM 20FR12B/A Form for initial registration of a class of securities of foreign private issuers pursuant to Section 12(b) [amend] Filing Date: 2002-01-14 SEC Accession No. 0000950133-02-000119 (HTML Version on secdatabase.com) FILER BAYER AKTIENGESELLSCHAFT Mailing Address Business Address BAYERWERK, GEBAEUDE W1 BAYERWERK, GEBAEUDE W1 CIK:1144145| Fiscal Year End: 1231 KAISER-WILHELM-ALLEE, KAISER-WILHELM-ALLEE, Type: 20FR12B/A | Act: 34 | File No.: 001-16829 | Film No.: 2509089 D-51368 LEVERKUSEN D-51368 LEVERKUSEN SIC: 8880 American depositary receipts GERMANY I8 00000 GERMANY I8 000000 492143081933 Copyright © 2012 www.secdatabase.com. All Rights Reserved. Please Consider the Environment Before Printing This Document AS FILED WITH THE SECURITIES AND EXCHANGE COMMISSION ON JANUARY 14, 2002 -------------------------------------------------------------------------------- -------------------------------------------------------------------------------- UNITED STATES SECURITIES AND EXCHANGE COMMISSION WASHINGTON, D.C. 20549 ------------------------------------ Amendment No. 1 to FORM 20-F <Table> <S> <C> <C> (Mark One) [X] REGISTRATION STATEMENT PURSUANT TO SECTION 12(b) OR 12(g) OF THE SECURITIES EXCHANGE ACT OF 1934 OR [ ] ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 OR [ ] TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 Commission file number </Table> BAYER AKTIENGESELLSCHAFT (Exact name of Registrant as specified in its charter) BAYER CORPORATION* (Translation of Registrant's name into English) FEDERAL REPUBLIC OF GERMANY (Jurisdiction of incorporation or organization) BAYERWERK, GEBAUDE W1 KAISER-WILHELM-ALLEE 51368 LEVERKUSEN, GERMANY (Address of principal executive offices) ------------------------------------ Securities registered or to be registered pursuant to Section 12(b) of the Act. -
When Matters of the Heart Matter Most
When matters of the heart matter most A tool to encourage a heart-to-heart on your OTC analgesic recommendation Your analgesic recommendation: A matter worth talking about Your patients who have cardiovascular disease or take other medications may not know that acetaminophen and NSAIDs are different, or how they can affect their heart. The American Heart Association identifies acetaminophen as a pain relief option to try first for patients with, or at high risk for, cardiovascular disease1 TYLENOL® does not interfere with the benefits of aspirin heart therapy the way ibuprofen can2 TYLENOL® won’t compromise blood pressure control the way NSAIDs sometimes can3 TYLENOL® won’t interfere with certain high blood pressure medications the way NSAIDs sometimes can3,4 NSAIDs, except aspirin, increase the risk of heart attack, heart failure, and stroke5 Counseling tip! As a healthcare professional, you may recommend TYLENOL® up to 4000 mg/day* Every medicine matters Remind patients to always read and follow the product label and never take multiple products that contain the same active ingredient at the same time. This may help reduce harmful side effects. Common medicines that contain acetaminophen OTC Rx Alka-Seltzer®† Mucinex® Endocet® Tylox® BENADRYL® NyQuil® Fioricet® Ultracet® Comtrex® DayQuil® Lorcet® Vicodin® Contac® Pamprin® Lortab® Coricidin® Robitussin® Maxidone® Dimetapp® SUDAFED®‡ Norco® Dristan®† Tavist® Percocet® Excedrin®† Theraflu® Roxicet™ FeverAll® TYLENOL® TYLENOL® with Codeine Goody’s®† Vanquish® Midol®† Vicks® Common medicines that contain an NSAID OTC Rx Advil® Dristan®† Celebrex® Lodine® Aleve® Ecotrin® Clinoril® Mobic® Alka-Seltzer®† Excedrin®† Daypro® Naproxen Anacin® Goody’s®† Dolobid® Relafen® Bayer® Midol®† Feldene® Toradol® BC®† MOTRIN® Ibuprofen Ultracet® Bufferin® Inocin® Vicoprofen® This is not a complete list. -

Getting Into Your Head(Ache): Advertising Content for OTC Analgesics!
Getting into Your Head(ache): Advertising Content for OTC Analgesics Simon P. Anderson,y Federico Cilibertoz and Jura Liaukonytex Marketing Science Institute Working Paper February 2008 Abstract The over-the-counter analgesics market is characterized by substantial advertising expenditures by the top brands. Advertising-to-sales ratios in this industry range from 20-50%, and are more than 7 times higher than the average for all industrial sectors. We use a novel dataset where we code the product characteristics featured in adver- tisements. For comparative advertisements, we record the rival products mentioned as well as the characteristics used for comparisons. We provide a comprehensive, …ve-year description of the number and types of characteristics mentioned in ads as well as the ad expenditures spent on emphasizing particular characteristics. The content analysis highlights the role of di¤erent types of advertising in enhancing product di¤erentiation. We then consider some theoretical hypotheses and test them with our data. First, we …nd that leading brands will be targeted most. Second, the fraction of compara- tive advertising is highest for new brands, and those with low market shares. Third, comparative advertising targets rival brands rather than stablemates. Fourth, there is only limited support for the idea that each characteristic will be advertised by only one product. However, we …nd that nationally advertised brands tend to specialize in which characteristics they advertise the most. Fifth, comparative advertising claims are more likely for experience rather than credence attributes. Finally, we …nd that usually comparative advertising targets products with active ingredients di¤erent from that of the attacking product. -

Medication Guide Before and After Surgery
Name: _______________ DOB: ________________ MEDICATION GUIDE § DO NOT take Vitamin E, red wine, Advil, Aleve, midol, naproxen, ibuprofen, aspirin, Motrin, indomethicin, or any medications that are Nonsteroidal Antiinflammatory Drug (NSAID) for 10 days before surgery, and 10 days after surgery. § It is recommended to stop taking any estrogen containing medications including birth control 10 days prior to surgery and do not resume until 10 days after surgery. If you have an implantable device, you do NOT need to remove it. § Nausea can occur from anesthesia or from the oxycodone. You may take Zofran for nausea but make sure you stay hydrated if this happens. § You do not need an antibiotic for this procedure. § You will be prescribed Celebrex (celecoxib), Gabapentin, Zofran(ondansetron), and Oxycodone. § Sometimes insurance does not cover Celebrex and the costs is ~$80-100. You may choose not to fill this prescription if you do not want to. § Please pickup Tylenol/Acetaminophen, Colace, and a bottle of Hibiclens at your pharmacy. 10 Days before Surgery: STOP all Vitamin E, red wine, and Aspirin, Motrin, Advil, Ibuprofen, Aleve, Naprosyn, Midol, Indomethicin or any anti-inflammatory medications. If you are not sure, please ask. You may take Tylenol/Acetaminophen. Day before Surgery: Cleanse area with Hibiclens (Chlorhexidine) for any surgery below the neck. Take Gabapentin 300 mg in the evening No Food or Drink after Midnight, this includes snacks, gum, crackers, and coffee. Name: _______________ DOB: ________________ Day of Surgery: Morning (before surgery): No Food or Drink Cleanse area with Hibiclens for any surgery below the neck. Take (with small sip of water): • Gabapentin 300 mg • Celebrex 400 mg (2 x 200 mg capsules) • Tylenol/acetaminophen 1000 mg (2 extra-strength tabs) • Approved morning medications After Surgery: Drink plenty of fluids. -

211733Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 211733Orig1s000 OTHER REVIEW(S) U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research Office of Drug Evaluation IV (ODE IV) Office of Biostatistics (OB) Integrated Review Label Comprehension Study Application Type/Number NDA 211733 Drug Name(s) Advil ® Dual Action with Acetaminophen (Ibuprofen 125 mg / Acetaminophen 250 mg Tablets) Indication(s) Pain reliever Applicant/sponsor Pfizer Inc. Date(s) Submission Date: November 21, 2019 PDUFA Goal Date: February 29, 2020 Reviewers Amanda Pike-McCrudden, MAA, Social Science Analyst, Division of Nonprescription Drugs (DNPD) Sai Dharmarajan PhD, Statistical Reviewer, Division of Biometrics VII (DB7) Elande Baro, PhD, Statistical Reviewer, DB7 Concurring Reviewer Yong Ma, PhD, Team Leader, DB7 Jody Green, MD, Clinical Team Leader, DNPD Tertiary Reviewer Mat Soukup, PhD, Deputy Director, DB7 Karen Mahoney, MD, Deputy Director, DNPD Project Manager Sally Doan, DNPD 1 Reference ID: 4567115 Table of Contents Executive Summary....................................................................................................................................4 1. Introduction and Background ...........................................................................................................4 1.1 Overview ......................................................................................................................................4 1.2 Data Sources .................................................................................................................................4 -

Nsaids Non- Steroidal Anti-Inflammatory Drug(S)
NSAIDs Non- Steroidal Anti- Inflammatory Drug(s) This is one of the most commonly used classes of drugs in the world. They are generally effective for pain and inflammation, but can have numerous side effects and complications that may require further medical attention. Generic Name Trade Name Tablet Size Ibuprofen* Advil, Motrin 200, 600, 800mg Naproxen* Aleve, Midol, Naprosyn 200, 220mg Nabumetone Relafen 500, 750mg Meloxicam Mobic 7.5, 15mg Diclofenac Cambia, Cataflam, Voltaren 50,75, 100 mg Ketorolac Toradol I.V. formulation Etodolac - 200-600mg Sulindac Clinoril 150, 200mg Indomethacin Indocin 25, 50, 75 mg Celecoxib Celebrex 50-400mg Salsalate - 500, 750mg *Available over the counter without a prescription. We STRONGLY recommend that you NOT take NSAIDs if you have chronic kidney disease (CKD), high blood pressure (hypertension), fluid retention (edema), or a condition requiring blood thinners such as: aspirin, Plavix, and/or warfarin (Coumadin). SPECIAL CASES: Aspirin–May be prescribed or recommended as 81mg or 325mg daily for prevention of heart attack and stroke by your other physicians. • These doses are generally thought to have minimal side effects and not adversely affect your kidney function. • Taking doses higher than this for headaches or pain relief will have the same risks as other NSAIDs. Acetaminophen (Tylenol)– Generally safe for use with other blood thinners, and does not affect kidney function. • Can cause liver toxicity in doses exceeding a total of 4,000mg in 24 hours. • Used as a component of other narcotic pain