The Impact of Political Devolution on the Uk's Health Services
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Criminological Policy Mobilities and Sex Work: Understanding the Movement of the ‘Swedish Model’ to Northern Ireland
Northumbria Research Link Citation: McMenzie, Laura, Cook, Ian and Laing, Mary (2019) Criminological policy mobilities and sex work: Understanding the movement of the ‘Swedish model’ to Northern Ireland. British Journal of Criminology, 59 (5). pp. 1199-1216. ISSN 0007-0955 Published by: Oxford University Press URL: https://doi.org/10.1093/bjc/azy058 <https://doi.org/10.1093/bjc/azy058> This version was downloaded from Northumbria Research Link: http://nrl.northumbria.ac.uk/36688/ Northumbria University has developed Northumbria Research Link (NRL) to enable users to access the University’s research output. Copyright © and moral rights for items on NRL are retained by the individual author(s) and/or other copyright owners. Single copies of full items can be reproduced, displayed or performed, and given to third parties in any format or medium for personal research or study, educational, or not-for-profit purposes without prior permission or charge, provided the authors, title and full bibliographic details are given, as well as a hyperlink and/or URL to the original metadata page. The content must not be changed in any way. Full items must not be sold commercially in any format or medium without formal permission of the copyright holder. The full policy is available online: http://nrl.northumbria.ac.uk/pol i cies.html This document may differ from the final, published version of the research and has been made available online in accordance with publisher policies. To read and/or cite from the published version of the research, please visit the publisher’s website (a subscription may be required.) doi:10.1093/bjc/azy058 BRIT. -
Keith Mcbride, Clerk to Committee for Health
Committee for Health Room 410 Parliament Buildings Ballymiscaw Stormont Belfast BT4 3XX Tel: +44 (0)28 9052 1634 Northern Ireland Assembly To: Christine Darrah, Clerk to Committee for Justice From: Keith McBride, Clerk to Committee for Health Date: 29 April 2021 Subject: Damages (Return on Investments) Bill – Departmental response Christine At its meeting today the Committee for Health considered the reply from the Department of Health to the Damages (Return on Investments) Bill. The Committee acknowledged and noted its content and agreed to inform the Committee for Justice of its acknowledgement. For completeness please find enclosed a copy of the reply from the Department of Health. Keith McBride Clerk, Committee for Health Enc. Wendy Patterson DALO Department of Health Castle Buildings Stormont Belfast BT4 3SQ Our Ref.: C95/21 16 April 2021 Dear Wendy, Re: Committee for Justice Damages (Return on Investment) Bill At the meeting on 15 April 2021 the Committee for Health considered correspondence received from the Committee for Justice regarding the Damages (Return on Investment) Bill. The Bill passed Second Stage on 9 March 2021 and the Committee Stage commenced on 10 March 2021. The Committee is aware that the Department of Health has also been invited to submit written evidence on the Bill. Members agreed to write to the Department to get its views on the Bill and its impact in relation to the Department of Health. The Committee also requested to be copied into any response the Department provides to the Committee for Justice. Please forward this submission by 07 May 2021. Yours sincerely, Keith McBride Clerk Committee for Health Committee for Health Room 410, Parliament Buildings, Stormont, Belfast BT4 3XX Telephone: (028) 9052 1634 E-mail: [email protected] follow us on Twitter: @NIAHealth . -

Leverhulme-Funded Monitoring Programme
Leverhulme-funded monitoring programme Northern Ireland report 5 November 2000 Contents Summary Robin Wilson 3 Storm clouds gather Robin Wilson 4 Devolved government Robin Wilson Liz Fawcett 10 The assembly Rick Wilford 17 The media Greg McLaughlin 28 Public attitudes and identity (Nil return) Intergovernmental relations John Coakley Graham Walker 32 Relations with the EU Elizabeth Meehan 43 Relations with local government (Nil return) Finance Robin Wilson 47 Devolution disputes (Nil return) Political parties and elections Duncan Morrow Rick Wilford 49 Public policies Duncan Morrow 55 2 Summary It was the best, but also the worst, of times in Northern Ireland during this quarter. The four-party executive finally agreed in October what it would substantively do after 30 months of high- (or, perhaps, low-) political manoeuvring between the ethno- nationalist protagonists. Here, at last, was a draft Programme for Government. One, indeed, with a confidence-building message of ‘making a difference’; one, too, with some ‘joined-up’ sophistication and the capacity thus to cement the partisan ministerial fiefdoms. Here, also, was a draft budget, for the first time reflecting regional priorities. Meanwhile, there was patient work in the assembly—if criticism of its lack of transparency—and the Civic Forum met. But a poll showed confidence in the agreement falling—sharply amongst Catholics, to rock-bottom amongst Protestants. And the institutions of the agreement—their interdependence meaning shocks destabilise the whole baroque architecture—came under increasing strain. The failure of the policing commission to generate a consensual report led to a Police Bill both unionists and nationalists opposed. Ethnic hurt mobilised (or, perhaps, exploited) in the Protestant community over the loss of the Royal Ulster Constabulary name (symbolising its 302 victims) struck a body-blow to David Trimble as Ulster Unionist Party leader and first minister, as the Democratic Unionists—undermining the executive by their absence—won a hitherto safe UUP seat. -

A Democratic Design? the Political Style of the Northern Ireland Assembly
A Democratic Design? The political style of the Northern Ireland Assembly Rick Wilford Robin Wilson May 2001 FOREWORD....................................................................................................3 EXECUTIVE SUMMARY .................................................................................4 Background.........................................................................................................................................7 Representing the People.....................................................................................................................9 Table 1 Parties Elected to the Assembly ........................................................................................10 Public communication......................................................................................................................15 Table 2 Written and Oral Questions 7 February 2000-12 March 2001*........................................17 Assembly committees .......................................................................................................................20 Table 3 Statutory Committee Meetings..........................................................................................21 Table 4 Standing Committee Meetings ..........................................................................................22 Access to information.......................................................................................................................26 Table 5 Assembly Staffing -
Peter Robinson DUP Reg Empey UUP Robin Newton DUP David Walter Ervine PUP Naomi Rachel Long Alliance Michael Stewart Copeland UUP
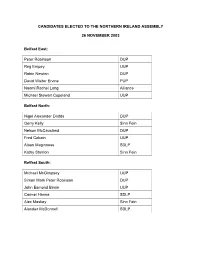
CANDIDATES ELECTED TO THE NORTHERN IRELAND ASSEMBLY 26 NOVEMBER 2003 Belfast East: Peter Robinson DUP Reg Empey UUP Robin Newton DUP David Walter Ervine PUP Naomi Rachel Long Alliance Michael Stewart Copeland UUP Belfast North: Nigel Alexander Dodds DUP Gerry Kelly Sinn Fein Nelson McCausland DUP Fred Cobain UUP Alban Maginness SDLP Kathy Stanton Sinn Fein Belfast South: Michael McGimpsey UUP Simon Mark Peter Robinson DUP John Esmond Birnie UUP Carmel Hanna SDLP Alex Maskey Sinn Fein Alasdair McDonnell SDLP Belfast West: Gerry Adams Sinn Fein Alex Atwood SDLP Bairbre de Brún Sinn Fein Fra McCann Sinn Fein Michael Ferguson Sinn Fein Diane Dodds DUP East Antrim: Roy Beggs UUP Sammy Wilson DUP Ken Robinson UUP Sean Neeson Alliance David William Hilditch DUP Thomas George Dawson DUP East Londonderry: Gregory Campbell DUP David McClarty UUP Francis Brolly Sinn Fein George Robinson DUP Norman Hillis UUP John Dallat SDLP Fermanagh and South Tyrone: Thomas Beatty (Tom) Elliott UUP Arlene Isobel Foster DUP* Tommy Gallagher SDLP Michelle Gildernew Sinn Fein Maurice Morrow DUP Hugh Thomas O’Reilly Sinn Fein * Elected as UUP candidate, became a member of the DUP with effect from 15 January 2004 Foyle: John Mark Durkan SDLP William Hay DUP Mitchel McLaughlin Sinn Fein Mary Bradley SDLP Pat Ramsey SDLP Mary Nelis Sinn Fein Lagan Valley: Jeffrey Mark Donaldson DUP* Edwin Cecil Poots DUP Billy Bell UUP Seamus Anthony Close Alliance Patricia Lewsley SDLP Norah Jeanette Beare DUP* * Elected as UUP candidate, became a member of the DUP with effect from -

Ongoing Reforms and Policy Developments
Published on Eurydice (https://eacea.ec.europa.eu/national-policies/eurydice) Overall national education strategy and key objectives Northern Ireland Assembly 2017-2022 mandate An early election of the Northern Ireland Assembly was held on 2 March 2017. This followed the resignation, on 9 January 2017, of the Deputy First Minister Martin McGuinness and the subsequent collapse of the power-sharing Executive. Following the election, the Northern Ireland parties were unable to reach agreement on the formation of a new Executive. There followed a period of three years in which there were no executive ministers and the Northern Ireland Assembly did not sit. In early 2020, following an extended period of political talks, an Executive was formed and ministers were appointed; DUP leader Arlene Foster was appointed Northern Ireland's first minister, while Sinn Féin's Michelle O'Neill was appointed deputy first minister. The Northern Ireland Assembly reconvened on 11 January 2020. The return to devolved government in Northern Ireland was on the basis of a deal set out in New Decade, New Approach [1], a document published by the UK Government and the Irish Government, and endorsed by all five main political parties in Northern Ireland. New Decade, New Approach sets out the immediate priorities for the restored Northern Ireland Executive, including the following commitments on education: The Executive will resolve the teachers’ industrial dispute and address resourcing pressures in schools, to ensure that every school has a sustainable core budget to deliver quality education. The Executive will establish an external, independent review of education provision, with a focus on securing greater efficiency in delivery costs, raising standards, access to the curriculum for all pupils, and the prospects of moving towards a single education system. -

INTRODUCTION 1. I Refer to Both the 'National State' and the 'Nation-State' Simply As the 'Nation-State'. Strictly S
Notes INTRODUCTION 1. I refer to both the ‘national state’ and the ‘nation-state’ simply as the ‘nation-state’. Strictly speaking, the state is a ‘national state’ when its centralized, autonomous and differentiated structures uphold legitimate authority within a boundary which contains multiple regions. However, a nation-state exists only where the citizenry share a common code of national identity expressed in language, religion, myth and custom. The majority of modern European states are quintessentially national states, while only a small minority, ostensibly the Republic of Ireland and Sweden, could satisfactorily qualify as nation-states (Tilly, 1990, pp. 2–3). 2. A proliferation of smaller parties emerged to stand, with modest suc- cess, in the 1996 election to the Northern Ireland Forum. These par- ties recorded the following percentage share of the vote in this election: the UK Unionist Party (UKU), 3.69 per cent; the Progressive Unionist Party (PUP), 3.47 per cent; the Ulster Democratic Party (UDP), 2.22 per cent; the Women’s Coalition, 1.03 per cent; and, Labour, 0.85 per cent (Irish Times, 1 June 1996). It is appreciated that the fringe parties represent distinct positions in the spectrum of Northern Ireland poli- tics. However, limited space prevents a detailed consideration of these positions. 3. In the 1994 election to the European Parliament the percentage of the vote secured by these five main political parties in Northern Ire- land was as follows: DUP, 29.15 per cent; UUP, 23.83 per cent; APNI, 4.13 per cent; SDLP, 28.93 per cent; Sinn Féin, 9.86 per cent – giving a combined total of 95.9 per cent. -

Committee for Health Meeting Minutes of Proceedings 22 October 2020
Northern Ireland Assembly COMMITTEE FOR HEALTH MINUTES OF PROCEEDINGS Thursday, 22 October 2020 Senate Chamber, Parliament Buildings Present: Mr Colm Gildernew (Chairperson) Ms Pam Cameron MLA (Deputy Chairperson)* Ms Paula Bradshaw MLA* Mr Gerry Carroll MLA Mr Alan Chambers MLA* Mr Alex Easton MLA Ms Órlaithí Flynn MLA* Mr Colin McGrath MLA* Mr Pat Sheehan MLA In Attendance: Ms Éilis Haughey (Clerk) Ms Jean Barkley (Assistant Assembly Clerk) Mr Jonathan Lamont (Clerical Supervisor) *These Members attended the meeting via video-conference. The meeting commenced at 9.33 am in public session. 1. Apologies None. 2. Chairperson’s Business i. The Chairperson advised that Mr Alex Easton would be leaving the Committee and he thanked Mr Easton for his contribution to the work of the Health Committee. ii. The Chairperson advised that the Deputy Chairperson was self-isolating after receiving an exposure notification from the StopCOVID NI proximity app and encouraged members of the public to download and use the app. 3. Draft Minutes The Committee agreed the minutes of the meetings held on 13 and 15 October 2020. 1 4. Matters Arising i. The Chairperson reminded Members that at the previous week’s meeting the Committee had agreed to forward correspondence from the Committee for Finance, to the Department of Health, seeking details on bids submitted to the Department of Finance; and requested Members’ agreement that relevant documents be shared with the Finance Committee to assist with their work on the Review of Financial Processes. Agreed: The Committee agreed to forward financial returns from the Department of Health to the Committee for Finance. -

Constituency Profiles for Further and Higher Education in Northern Ireland
COUNTMAKE EDUCATION CONSTITUENCY PROFILES FOR FURTHER AND HIGHER EDUCATION IN NORTHERN IRELAND CONSTITUENCY PROFILES FOR FURTHER AND HIGHER EDUCATION MAKE EDUCATION COUNT IN NORTHERN IRELAND Introduction It’s 2010 – the second decade of the 21st century – and it remains a stark reality that Northern Ireland is still riddled with some of the more dire statistics in the UK, when it comes to educational attainment and employment. Northern Ireland is bottom of UK tables that measure employment rates and people with qualifications, according to UCU analysis. Just over two-thirds of people in Northern Ireland (69.7%) are employed, the worst percentage of the UK's 12 regions. The South East of England tops the table with over three-quarters of people (78.5%) employed. The average is 74%. Northern Ireland has the highest percentage of people without qualifications. One in five (21.8%) have no qualifications, which is a long way off the national average of 12.4%. Northern Ireland fares slightly better when it comes to the percentage of people with a degree though. Over a quarter of people (25.7%) have a degree, which puts Northern Ireland in the middle of the regions' table but still some way behind the average of 29%. Contents Political constituency analysis 03 Lagan Valley 13 Summary of key findings 03 Mid Ulster 14 Constituency profiles Newry and Amargh 15 Belfast East 05 North Antrim 16 Belfast North 06 North Down 17 Belfast South 07 South Antrim 18 Belfast West 08 South Down 19 East Antrim 09 Strangford 20 East Londonderry 10 Upper Bann 21 -
UP DUP A4 Manifesto FINAL AW
PROTECTING THE TAXPAYER CONTROLLING THE COST OF GOVERNMENT campaign03THE DUP’S VISION FOR DEVOLUTION FAIR DEAL MANIFESTO THE CHOICE FOR UNIONISTS THE BELFAST AGREEMENT OR A NEW AGREEMENT? THE UUP RECORD OF FAILURE 2003 ADIARY OF DECLINE OUR FULL MANIFESTO DUP MINISTERS INSIDE THIS MAGAZINE ARECORD OF ACHIEVEMENT DELIVERING AN EFFECTIVE POLICE SERVICE WORKING FOR BETTER POLICING THE BELFAST AGREEMENT MESSAGE FROM IS WRECKING NORTHERN IRELAND: THE LEADER: This election is Ulster’s date with destiny. I DON’T WANT It is the chance to put things right, to give a mandate to a strong and united Democratic Unionist team and to negotiate a new agreement. Stop and think how much has happened since 10th April 1998. Has it been the journey we were promised? The destruction of the RUC,the withdrawal of the Army,the release of terrorist FOUR prisoners,the elevation of Sinn Fein/IRA members to government office without evidence of the destruction of weaponry,the creation of ever-expanding all-Ireland institutions,the lawless state of our Province,the ever-growing list of breaches of MORE YEARS IRA and loyalist so-called ceasefires,the disregard of the views of peaceful and democratic politicians in favour of the spokesmen of terrorist organisations. OF Now imagine where Northern Ireland will be in another For unionist voters who face the prospect of Sinn four years if we allow the concessions to continue: Fein/IRA becoming the largest nationalist party in the Assembly the choice is clear - do they want republicans Terrorists running the police,a joint -
The DUP Offers an Unrivalled Constituency Service
DUP DELIVERING FOR UNIONISTSKEEPING UNIONISM NUMBER 1 KEEPING OUR PROMISES A RECORD OF ACHIEVEMENT NO TURNING BACK STRENGTH IN NEGOTIATIONS UNRIVALLED CONSTITUENCY REPRESENTATION TIME TO MOVE ON SEND A MESSAGE TO GOVERNMENT RESPECTING SENIOR CITIZENS SAFE FROM CRIME OPPOSING WATER CHARGES TACKLING RACISM GETTING SERIOUS ABOUT ROAD SAFETY SAVING GRAMMAR SCHOOLS REVIEW OF PUBLIC ADMINISTRATION OUR ROLE AT WESTMINSTER A ROLE IN THE AFFAIRS OF THE NATION PARLIAMENTARY AND LOCAL GOVERNMENT Manifesto2005 DUP : DELIVERING FOR UNIONISTS “Sinn Fein is in the doghouse. The pan-nationalist front has been consigned to the political dustbin.The political process is at a standstill and the DUP has the whip hand.” Paul Colgan Irish Echo, 16th February 2005 Even our opponents bear witness that after years in decline,unionism is finally on top. Don’t let Trimble wreck it. 2 www.dup2win.com PARLIAMENTARY AND LOCAL GOVERNMENT ELECTIONS Manifesto2005 Vote DUP:Everywhere! Paisley Simpson Foster Wilson www.dup2win.com 3 Manifesto2005 PARLIAMENTARY AND LOCAL GOVERNMENT ELECTIONS INTRODUCTION: For the first time in a generation unionism has leadership that’s working. Just remember what it was like only eighteen months ago when the Ulster Unionist Party was in charge. Republicans won concession after concession while unionism was in retreat. In every negotiation republicans exploited the weakness of the UUP and were allowed to dictate t heir own terms. Now,all that has changed.Today it is the DUP’s agenda that dominates the political process with London, Dublin and Washington accepting our demands as fundamental prerequisites. The pan-nationalist front has been fractured and Sinn Fein is more isolated than ever before. -

Northern Ireland Assembly Elections 2011
Northern Ireland Assembly Elections: 2011 RESEARCH PAPER 11/42 18 May 2011 Elections on 5 May 2011 resulted in little change in the overall party composition of the Northern Ireland Assembly. Gains and losses by individual parties involved just one or two seats. 108 Assembly Members were elected by Single Transferrable Vote, 6 Members for each of 18 constituencies. Following the 2011 elections the two largest parties in the Assembly are the DUP (38 MLAs) and Sinn Féin (29 MLAs). Richard Cracknell Recent Research Papers 11/26 Unemployment by Constituency 16.03.11 11/27 Economic Indicators, Budget update 22.03.11 11/28 Police Reform and Social Responsibility Bill: Committee 24.03.11 Stage Report 11/29 Economic Indicators, April 2011 05.04.11 11/30 Direct taxes: rates and allowances 2011/12 06.04.11 11/31 Health and Social Care Bill: Committee Stage Report 06.04.11 11/32 Localism Bill: Committee Stage Report 12.04.11 11/33 Unemployment by Constituency, April 2011 14.04.11 11/34 London Olympic Games and Paralympic Games (Amendment) Bill 21.04.11 [Bill 165 of 2010-12] 11/35 Economic Indicators, May 2011 03.05.11 11/36 Energy Bill [HL] [Bill 167 of 2010-12] 04.05.11 11/37 Education Bill: Committee Stage Report 05.05.11 11/38 Social Indicators 06.05.11 11/39 Legislation (Territorial Extent) Bill: Committee Stage Report 11.05.11 Research Paper Contributing Authors: Richard Cracknell Jeremy Hardacre This information is provided to Members of Parliament in support of their parliamentary duties and is not intended to address the specific circumstances of any particular individual.