28 Apr 2021 Public Accounts Committee: Genomic
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Actions Reporting
PROGRAMME FOR GOVERNMENT Q1 REPORTING 2017 ACTIONS Actions The Programme for Government ‘Our Island - a special place to live and work’ was approved by Tynwald in January 2017 and in April 2017 a performance framework, ‘Delivering a Programme for Government’, was also approved. The ‘Programme for Government 2016-21’ is a strategic plan that outlines measurable goals for Government. The Council of Ministers have committed to providing a public update against the performance framework on a quarterly basis. This report provides an update on performance through monitoring delivery of the actions committed to. The first quarter for 2017/18 ran April, May, June and reporting for this period has been undertaken during the past 4 weeks. Information has been provided from across Government Departments, Boards and Offices, and the Cabinet Office have collated these to provide this report on Key Performance Indicators. The Programme for Government outlines a number of initial actions that were agreed by the Council of Ministers which will help take Government closer to achieving its overall objectives and outcomes. Departments Boards and Offices have developed action plans to deliver these actions and this report provides an update status report on delivery against these action plans. POLITICAL OUTCOME TITLE Q1 Data Comment SPONSOR Promote and drive the Enterprise Development Fund and Martyn Perkins ensure it is delivering jobs and new businesses for our GREEN We have an economy where Chairman OFT local entrepreneurship is Island supported and thriving -
Newsletter from the West of the Island
Geoffrey Ray Harmer Boot MHK for MHK for Glenfaba & Peel Glenfaba & Peel Minister of Minister of Environment Food Infrastructure & Agriculture (DOI) (DEFA) Tynwald: 01624 685485 Tynwald: 01624 685596 Mobile: 07624 381497 Mobile: 07624 215577 www.geoffreyboot.org Spring 2017 www.rayharmer.im [email protected] [email protected] Glenfaba & Peel Welcome to our first newsletter from the West of the Island. We both gave a commitment during the election to stay in touch, part of that commitment revolved around hard copy newsletters as we are aware that not everyone has access to websites, Facebook and Twitter. Programme for Government One of the most important tasks for any new administration is to put together a Programme for Government for the next five years. In the past this has been a lengthy process, sometimes taking up to 18 months. After the election in September and our appointments to the Council of Ministers, the Chief Minister was determined we echo his sentiments by putting together a programme as quickly as possible but as inclusively as possible. Consultation with all MHKs started almost immediately and there were invitations for participation in the preparation for the programme to interested external parties including businesses. As a result a 100 days after the election the Programme for Government 2016 – 2021 was approved unanimously by Tynwald. The programme is available on this link www.gov.im/media/1354840/ programme-for-government.pdf and it is not our intention to go into great detail in this newsletter but there are three strategic objectives which are overarching aims of the Council of Ministers in the long term and approved by all members. -

Programme for Government Actions Q2 Y2
Page 1 of 19 PROGRAMME FOR GOVERNMENT ACTIONS Q2 Y2 Actions The Programme for Government ‘Our Island - a special place to live and work’ was approved by Tynwald in January 2017 and in April 2017 a performance framework, ‘Delivering a Programme for Government’, was also approved. The ‘Programme for Government 2016-21’ is a strategic plan that outlines measurable goals for Government. The Council of Ministers have committed to providing a public update against the performance framework on a quarterly basis. In March 2018 Tynwald approved a revised and updated Programme for Government for year two; 2018-19. KEY: Green: Project progressing to plan Amber: Project may need assistance in the future; currently handling within the project team but management team: be aware Red: Escalation: project team need help to resolve a problem Blue: Action is completed or superseded and has been closed Sub Lead Political End Outcome Ref Action Y2 Q1 Y2 Q2 Comm Dept Sponsor Date Promote and drive the Enterprise Development Fund Lawrie Hooper, Mar- 1.1 and ensure it is delivering jobs and new businesses for AMBER AMBER NSG DfE MHK 21 our Island We have an economy Partner with business to offer skills, training and Lawrie Hooper, Dec- 1.2 GREEN GREEN NSG DESC where local accreditations MHK 21 entrepreneur ship is Increase the uptake of our new products, like the AMBER Lawrie Hooper, Mar- supported 1.3 GREEN NSG DfE alternative banking regime and crowdfunding MHK 21 and thriving and more Carry out the TT/MGP economic assessment report for Alex Allinson, June- -

Bilateral Visit from Tynwald, Isle of Man 25 – 27 October 2017 Houses of Parliament, London
[insert map of the region] 1204REPORT/ISLEOFMAN17 Bilateral Visit from Tynwald, Isle of Man 25 – 27 October 2017 Houses of Parliament, London Final Report Contents About the Commonwealth Parliamentary Association UK ........................................................................................ 3 Summary ............................................................................................................................................................................ 4 Project Overview ............................................................................................................................................................. 5 Project Aim & Objectives ............................................................................................................................................... 5 Participants & Key Stakeholders ................................................................................................................................... 6 Key Issues .......................................................................................................................................................................... 6 Results of the Project ..................................................................................................................................................... 8 Next Steps ....................................................................................................................................................................... 10 Acknowledgements -
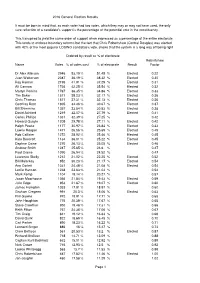
2016 General Election Statistics Summary
2016 General Election Results It must be born in mind that, as each voter had two votes, which they may or may not have used, the only sure reflection of a candidate's support is the percentage of the potential vote in the constituency. This transpired to yield the same order of support when expressed as a percentage of the entire electorate This tends to endorse boundary reforms but the fact that Chris Robertshaw (Central Douglas) was elected with 42% of the most popular LOSING candidate's vote, shows that the system is a long way off being right Ordered by result as % of electorate Robertshaw Name Votes % of votes cast % of electorate Result Factor Dr Alex Allinson 2946 53.19 % 51.45 % Elected 0.22 Juan Watterson 2087 36.19 % 38.32 % Elected 0.30 Ray Harmer 2195 41.91 % 37.29 % Elected 0.31 Alf Cannan 1736 42.25 % 35.54 % Elected 0.32 Martyn Perkins 1767 36.35 % 34.86 % Elected 0.33 Tim Baker 1571 38.23 % 32.17 % Elected 0.36 Chris Thomas 1571 37.31 % 32.13 % Elected 0.36 Geoffrey Boot 1805 34.46 % 30.67 % Elected 0.37 Bill Shimmins 1357 33.54 % 30.53 % Elected 0.38 David Ashford 1219 32.07 % 27.79 % Elected 0.41 Carlos Phillips 1331 32.39 % 27.25 % 0.42 Howard Quayle 1205 29.78 % 27.11 % Elected 0.42 Ralph Peake 1177 30.97 % 26.84 % Elected 0.43 Lawrie Hooper 1471 26.56 % 25.69 % Elected 0.45 Rob Callister 1272 28.92 % 25.46 % Elected 0.45 Kate Beecroft 1134 36.01 % 25.22 % Elected 0.45 Daphne Caine 1270 26.13 % 25.05 % Elected 0.46 Andrew Smith 1247 25.65 % 24.6 % 0.47 Paul Craine 1090 26.94 % 24.52 % 0.47 Laurence Skelly 1212 21.02 -

Actions Reporting
PROGRAMME FOR GOVERNMENT Q1 REPORTING 2019/20 DEPARTMENT ACTIONS 1 DEPARTMENT ACTIONS The Programme for Government ‘Our Island - a special place to live and work’ was approved by Tynwald in January 2017 and in April 2017 a performance framework, ‘Delivering a Programme for Government’, was also approved. The ‘Programme for Government 2016-21’ is a strategic plan that outlines measurable goals for Government. The Council of Ministers have committed to providing a public update against the performance framework on a quarterly basis. This report provides an update on performance through monitoring delivery of the actions committed to. The first quarter for 2019/20 ran April, May and June 2019. Information has been provided from across Government Departments, Boards and Offices, and the Cabinet Office have collated these to provide this report. The Programme for Government outlines a number of initial actions that were agreed by the Council of Ministers which will help take Government closer to achieving its overall objectives and outcomes. Departments Boards and Offices have developed action plans to deliver these actions and this report provides an update status report on delivery against these action plans. 2 Q2 Q3 Q4 Q1 Lead Lead Sub Ref Action Comment Political Sponsor End Date 2018/19 2018/19 2018/19 2019/20 Department Committee We have an economy where local entrepreneurship is supported and thriving and more new businesses are choosing to call the Isle of Man home 1.1.01 Promote and drive the Enterprise This action was Department -
Legislative Council Elections Bill Was One of Only Two Items to Pass Through Both Branches and Be Promulgated on Tynwald Hill Within the Same Year
Tynwald Annual Report Parliamentary year 2016/2017 We hope you will find this report useful. If you would like to comment on any aspect of it, please contact: The Clerk of Tynwald Office of the Clerk of Tynwald Legislative Buildings Finch Road Douglas Isle of Man IM1 3PW Get in touch Twitter : @tynwaldinfo Telephone: +44 (0)1624 685500 Email: [email protected] An electronic copy of this report can be found at: www.tynwald.org.im © Office of the Clerk of Tynwald Copyright 2017 The text of this document may be reproduced free of charge in any format or medium providing that it is reproduced accurately and not used in a misleading or derogatory context. The material must be acknowledged as copyright of the Office of the Clerk of Tynwald and the title of the document specified. PP 2017/0145 2 Tynwald Annual Report 2016/2017 Contents Foreword by the Presiding Officers 4 1867 Celebrations 6 Changes in Political Membership 8 The Work of the Legislature 10 Tynwald Day 18 Interparliamentary Engagement 26 Education and Outreach 34 The Clerk of Tynwald’s Office 42 Appendix 48 3 PRESIDENT OF TYNWALD The Hon Stephen Charles Rodan BSc (Hons) MRPharmS MLC SPEAKER OF THE HOUSE OF KEYS The Hon Juan Paul Watterson BA FCA CMgr FCMI SHK foreword 4 Tynwald Annual Report 2016/2017 Welcome to the Tynwald Annual Report 2016/7 2016 saw the 150th anniversary of the House of Keys Elections Act 1866. In 2017 we celebrated the 150th anniversary of the first elections which took place under that Act, with polling taking place in the first week of April 1867. -
2018-Nn-0012
Isle of Man Branch Report of the Chairman of the Branch Executive Committee for the period January 2017 to December 2017 Introduction 1. The aims of the Commonwealth Parliamentary Association are to promote knowledge of the constitutional, legislative, economic, social and cultural aspects of parliamentary democracy. It does this among other things by arranging Commonwealth Parliamentary Conferences, and other conferences, seminars, meetings and study groups; and by promoting visits between Members of the Branches of the Association. 2. This year saw the Isle of Man celebrate the 150th anniversary of the first popular election of the House of Keys, previously a self-elected body. 1867 was a date of pivotal significance in the advancement of Manx parliamentary democracy and a number of events took place to celebrate this anniversary in Manx political history. Farewells 3. 2017 saw the departure of just one CPA member: Mr Tony Wild was a member of the Legislative Council from 2011 to 2017 and an active member of the Isle of Man Branch. He represented the Isle of Man at regional conferences in Scotland in 2012 and the Falkland Islands in 2013, and attended a study visit to Westminster in 2012. On-Island activities in 2017 4. In February 2017 we were delighted to welcome Mr Akbar Khan, the Secretary- General of the Commonwealth Parliamentary Association, on his first visit to the Isle of Man, as part of a CPA parliamentary strengthening programme. During his visit Mr Khan delivered four CPA roadshows to schools in the Island, reaching more than 200 students; the roadshows focused on three core Commonwealth values - diversity, development and democracy. -
P R O C E E D I N G S
T Y N W A L D C O U R T O F F I C I A L R E P O R T R E C O R T Y S O I K O I L Q U A I Y L T I N V A A L P R O C E E D I N G S D A A L T Y N HANSARD Douglas, Tuesday, 4th October 2016 All published Official Reports can be found on the Tynwald website: www.tynwald.org.im/business/hansard Supplementary material provided subsequent to a sitting is also published to the website as a Hansard Appendix. Reports, maps and other documents referred to in the course of debates may be consulted on application to the Tynwald Library or the Clerk of Tynwald’s Office. Volume 134, No. 1 ISSN 1742-2256 Published by the Office of the Clerk of Tynwald, Legislative Buildings, Finch Road, Douglas, Isle of Man, IM1 3PW. © High Court of Tynwald, 2016 TYNWALD COURT, TUESDAY, 4th OCTOBER 2016 Present: The President of Tynwald (Hon. S C Rodan) In the Council: The Lord Bishop of Sodor and Man (The Rt Rev. R M E Paterson), The Acting Attorney General (Mr J L M Quinn), Mr D M Anderson, Mr M R Coleman, Mr C G Corkish MBE, Mr D C Cretney, Hon. T M Crookall, Mr R W Henderson, Mr J R Turner and Mr T P Wild, with Mr J D C King, Deputy Clerk of Tynwald. In the Keys: The Speaker (Hon. -

Tynwald Annual Report 2019/2020 Engage with Tynwald on Twitter @Tynwaldinfo
PP 2020/0187 Tynwald Annual Report Parliamentary Year 2019/2020 Tynwald Annual Report 2019/2020 Engage with Tynwald on Twitter @tynwaldinfo Get live updates during Tynwald sittings from @tynwaldlive We hope you will find this report useful. If you would like to comment on any aspect of it, please contact: The Clerk of Tynwald Office of the Clerk of Tynwald Legislative Buildings Finch Road Douglas Isle of Man IM1 3PW Telephone: +44 (0)1624 685500 Email: [email protected] An electronic copy of this report can be found at: http://www.tynwald.org.im/bu siness/pp/Reports/2020-PP-187 Tynwald Annual Report 2019/2020 Contents Page 2 Foreword 3 The Isle of Man and COVID-19 4 Changes in Membership 9 The Work of Legislature 18 Tynwald Day 2020 23 Inter Parliamentary Engagement 29 Education and Outreach 31 The Office of the Clerk of Tynwald 3 Tynwald Annual Report 2019/2020 Tynwald Annual Report 2019/2020 Foreword President of Tynwald Speaker of the House of Keys The Hon. Stephen Charles Rodan The Hon. Juan Paul Watterson BA OBE Bsc (Hons) MRPharmS MLC (Hons) BFP FCA CMgr FCMI FRSA SHK This has been a particularly difficult year. Political life was, of course, dominated in spring and early summer by the ravages of the COVID-19 pandemic, as in the rest of the world. We have been lucky in the Isle of Man that we have been spared some of the worst impact of this terrible disease; our hearts go out to those people who have lost loved ones or experienced the dangers and discomforts which the virus can bring. -

Hansard Business Search Template
4. Nomination of Chief Minister – Mr Howard Quayle elected In accordance with section 2 of the Council of Ministers Act 1990, to nominate one Member of Tynwald for appointment as Chief Minister. The Members proposed for nomination are: Mrs K J Beecroft Mr A L Cannan Hon R H Quayle The President: Hon. Members, we now turn to our Order Paper. The main business of today is the election of a Chief Minister. This election is governed by section 2 of the Council of Ministers Act 1990 and also by Standing Orders 1.5, 2.4A, 3.17A and 5.3, as amended by the recent change to Standing Orders, Standing Order 3.17B. Three members have been proposed: Mrs Kate Beecroft, proposed by Mr Lawrie Hooper and seconded by Ms Julie Edge; Mr Alfred Cannan, proposed by Mr Chris Thomas and seconded by Mr Martyn Perkins; and Mr Howard Quayle, proposed by Mr David Ashford and seconded by Mr Ray Harmer. I intend to take the nominations in alphabetical order of the nominees. I will therefore invite the proposer and seconder of the nomination of the Hon. Member for Douglas South, Mrs Beecroft, followed by the proposer and seconder of the nomination of the Hon. Member for Ayre and Michael, Mr Cannan, and then the Hon. Member for Middle, Mr Quayle. Following established practice, I shall allow Hon. Members’ proposing and seconding nominees to speak in support of that nominee, but I shall not allow other speeches. I remind Hon. Members of the procedure which is in two parts. -

MHK) Sent: 05 April 2017 09:04 To: Phillips, Roger Cc: Bill Shimmins; Chief Minister; Martyn Perkins Subject: Nomination of Candidate for Legislative Council Vacancy
From: Caine, Daphne (MHK) Sent: 05 April 2017 09:04 To: Phillips, Roger Cc: Bill Shimmins; Chief Minister; Martyn Perkins Subject: Nomination of candidate for Legislative Council vacancy Dear Roger I would like to nominate Mrs Jane Poole-Wilson for the vacancy on the Legislative Council. Bill Shimmins MHK has agreed to second her nomination, which is supported by Howard Quayle MHK and Martyn Perkins MHK. Manxborn and raised, Mrs Poole-Wilson is a qualified solicitor who has worked as an employment lawyer and HR training specialist working with a variety of mainly financial services companies in the United Kingdom, Europe and Asia. Alongside her international consultancy work, she was the Isle of Man Legal Aid Deputy Certifying Officer from 2007 to 2010. She has also gained experience in volunteering roles, most recently as a Trustee of St Christopher’s Isle of Man and Parent Governor at Marown School. Knowing Jane from thespian circles and aware that she intended to take a break from her high- flying career to focus on family responsibilities, I approached her to request she consider allowing me to put her name forward for consideration by Members for the Legislative Council vacancy. I am certain Jane’s quick understanding, legal background, communication skills, wide interests and her compassion and enthusiasm for the Isle of Man make her an ideal candidate for the upper chamber and I would ask Members to see the attached biography for more information. Contact details are: Mrs Jane Poole-Wilson [Address Supplied] Lesh yeearreeyn share – with best wishes Daphne Caine MHK for Garff Legislative Buildings Finch Road Douglas Isle of Man IM1 3PW British Isles Jane Poole-Wilson (nee Kissack) Born and grew up on the Isle of Man.