Download BIA's Concussion in Sport Policy Paper
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Physiological Demands of Competitive Basketball Kenji Narazaki University of Colorado Boulder
University of Nebraska at Omaha DigitalCommons@UNO Journal Articles Department of Biomechanics 6-2009 Physiological demands of competitive basketball Kenji Narazaki University of Colorado Boulder Kris E. Berg University of Nebraska at Omaha, [email protected] Nicholas Stergiou University of Nebraska at Omaha, [email protected] Bing Chen University of Nebraska-Lincoln Follow this and additional works at: https://digitalcommons.unomaha.edu/biomechanicsarticles Part of the Biomechanics Commons Recommended Citation Narazaki, Kenji; Berg, Kris E.; Stergiou, Nicholas; and Chen, Bing, "Physiological demands of competitive basketball" (2009). Journal Articles. 131. https://digitalcommons.unomaha.edu/biomechanicsarticles/131 This Article is brought to you for free and open access by the Department of Biomechanics at DigitalCommons@UNO. It has been accepted for inclusion in Journal Articles by an authorized administrator of DigitalCommons@UNO. For more information, please contact [email protected]. Physiological demands of competitive basketball K. Narazaki1, K. Berg2, N. Stergiou2, B. Chen3 1Department of Integrative Physiology, University of Colorado at Boulder, Boulder, Colorado, USA, 2School of Health, Physical Education & Recreation, University of Nebraska at Omaha, Omaha, Nebraska, USA, 3Department of Electronics Engineering, University of Nebraska at Lincoln, Omaha, Nebraska, USA Corresponding author: Kris Berg, School of Health, Physical Education & Recreation, University of Nebraska at Omaha, 6001 Dodge Street HPER Building Room 207, Omaha, Nebraska 68182-0216, USA. Tel: 11 402 554 2670, Fax: 11 402 554 3693, E-mail: [email protected] ABSTRACT: The aim of this study was to assess physiological demands of competitive basketball by measuring oxygen consumption (VO2) and other variables during practice games. Each of 12 players (20.4 ± 1.1 years) was monitored in a 20-min practice game, which was conducted in the same way as actual games with the presence of referees and coaches. -

Analysis of Concussion Management Policies and Procedures Among Athletic Trainers in the Four Divisions of NCAA Collegiate Football
Graduate Theses, Dissertations, and Problem Reports 2010 Analysis of concussion management policies and procedures among athletic trainers in the four divisions of NCAA collegiate football James D. Dorneman Jr. West Virginia University Follow this and additional works at: https://researchrepository.wvu.edu/etd Recommended Citation Dorneman, James D. Jr., "Analysis of concussion management policies and procedures among athletic trainers in the four divisions of NCAA collegiate football" (2010). Graduate Theses, Dissertations, and Problem Reports. 4581. https://researchrepository.wvu.edu/etd/4581 This Thesis is protected by copyright and/or related rights. It has been brought to you by the The Research Repository @ WVU with permission from the rights-holder(s). You are free to use this Thesis in any way that is permitted by the copyright and related rights legislation that applies to your use. For other uses you must obtain permission from the rights-holder(s) directly, unless additional rights are indicated by a Creative Commons license in the record and/ or on the work itself. This Thesis has been accepted for inclusion in WVU Graduate Theses, Dissertations, and Problem Reports collection by an authorized administrator of The Research Repository @ WVU. For more information, please contact [email protected]. Analysis of Concussion Management Policies and Procedures among Athletic Trainers in the Four Divisions of NCAA Collegiate Football James D. Dorneman Jr., BS, ATC Thesis submitted to the College of Physical Activity and Sport Sciences At West Virginia University In partial fulfillment of the requirements for the degree of Master of Science in Athletic Training Michelle A. Sandrey, Ph.D, ATC, Chair Lynn Housner, Ph.D. -

Consensus Statement on Concussion in Sport
Downloaded from bjsm.bmj.com on March 12, 2013 - Published by group.bmj.com Consensus statement Consensus statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012 Editor’s choice Scan to access more free content Paul McCrory,1 Willem H Meeuwisse,2,3 Mark Aubry,4,5,6 Bob Cantu,7,8 JiříDvořák,9,10,11 Ruben J Echemendia,12,13 Lars Engebretsen,14,15,16 Karen Johnston,17,18 Jeffrey S Kutcher,19 Martin Raftery,20 Allen Sills,21 Brian W Benson,22,23,24 Gavin A Davis,25 Richard G Ellenbogen,26,27 Kevin Guskiewicz,28 Stanley A Herring,29,30 Grant L Iverson,31 Barry D Jordan,32,33,34 James Kissick,6,35,36,37 Michael McCrea,38 Andrew S McIntosh,39,40,41 David Maddocks,42 Michael Makdissi,43,44 Laura Purcell,45,46 Margot Putukian,47,48 Kathryn Schneider,49 Charles H Tator,50,51,52,53 Michael Turner54 ▸ Additional material is PREAMBLE SECTION 1: SPORT CONCUSSION AND published online only. To view This paper is a revision and update of the recommen- ITS MANAGEMENT these files please visit the journal online (http://dx.doi. dations developed following the 1st (Vienna 2001), The Zurich 2012 document examines the sport org/10.1136/bjsports-2013- 2nd (Prague 2004) and 3rd (Zurich 2008) concussion and management issues raised in the 092313). International Consensus Conferences on Concussion previous Vienna 2001, Prague 2004 and Zurich For numbered affiliations see in Sport and is based on the deliberations at the 4th 2008 documents and applies the consensus ques- 1–3 end of article. -

Incidence, Awareness, and Reporting of Sport-Related Concussions in Manitoba High Schools
ORIGINAL ARTICLE COPYRIGHT © 2019 THE CANADIAN JOURNAL OF NEUROLOGICAL SCIENCES INC. Incidence, Awareness, and Reporting of Sport-Related Concussions in Manitoba High Schools Glen L. Bergeron ABSTRACT: Background and Objectives: Federal and provincial governments in Canada are promoting provincial legislation to prevent and manage sport-related concussions (SRCs). The objective of this research was to determine the incidence of concussions in high school sport, the knowledge of the signs, symptoms, and consequences of SRC, and how likely student athletes are to report a concussion. Methods: A cross-sectional survey of athletes (N = 225) from multiple sports in five high schools in one Manitoba school division was conducted. Results: Participants in this study were well aware of the signs, symptoms, and consequences of SRC. Cognitive and emotional symptoms were the least recognized consequences. SRC is prevalent in high schools in both males and females across all sports. Of the 225 respondents, 35.3% reported having sustained an SRC. Less than half (45.5%) reported their concussion. Athletes purposely chose not to report a concussion in games (38.4%) and practices (33.8%). Two major barriers to reporting were feeling embarrassed (3.4/7) and finding it difficult (3.5/7) to report. There was, however, strong agreement (Mean 5.91/7, SD 0.09) when asked if they intend to report a concussion should they experience one in the future. Conclusions: The results suggest that high school athletes would benefit from more SRC education. Coaches and team medical staff must be trained to be vigilant for the mechanism, signs, and symptoms of injury in both game and practice situations. -
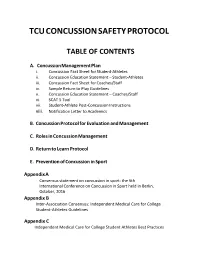
Tcu Concussion Safety Protocol
TCU CONCUSSION SAFETY PROTOCOL TABLE OF CONTENTS A. Concussion Management Plan i. Concussion Fact Sheet for Student-Athletes ii. Concussion Education Statement – Student-Athletes iii. Concussion Fact Sheet for Coaches/Staff iv. Sample Return to Play Guidelines v. Concussion Education Statement – Coaches/Staff vi. SCAT 5 Tool vii. Student-Athlete Post-Concussion Instructions viii. Notification Letter to Academics B. Concussion Protocol for Evaluation and Management C. Roles in Concussion Management D. Return to Learn Protocol E. Prevention of Concussion in Sport Appendix A Consensus statement on concussion in sport: the 5th International Conference on Concussion in Sport held in Berlin, October, 2016 Appendix B Inter-Association Consensus: Independent Medical Care for College Student-Athletes Guidelines Appendix C Independent Medical Care for College Student Athletes Best Practices Concussion Management Plan: This plan is based on the most current evidence on concussions available as well as the recommended best practices for concussion management distributed by the NCAA Committee on Competitive Safeguards in Sport. As such, modifications may follow as the science of concussion diagnosis, education, and treatment advances. All incoming student-athletes, including transfer students and anyone new to the program, will be subject to this plan. PRE-PRACTICE EDUCATION: 1) Student athletes will undergo a formal education program on concussion in sport. Topics covered will include mechanism of injury, recognition of signs and symptoms of concussion, and strategies to avoid injury/prevent further sequelae. The ‘Concussion Fact Sheet for Student-Athletes’ provided by the NCAA will also be distributed at this time. This will be completed before participating in the first official practice session and will be directed by a staff athletic trainer and/or team physician. -

Football Facts and Figures Activity Guide 2017-2018 Pro Football Hall of Fame 2017-2018 Educational Outreach Program Football Facts and Figures Table of Contents
Pro Football Hall of Fame Youth & Education Football Facts and Figures Activity Guide 2017-2018 Pro Football Hall of Fame 2017-2018 Educational Outreach Program Football Facts and Figures Table of Contents Lesson Page(s) Canton, Ohio and the National Football League FF 1 Who Was Jim Thorpe? FF 2 Gridiron Terminology FF 3 National Football League FF 4-5 2017 Team Colors FF 6 Football Facts FF 7 2017 NFL Schedule FF 8-9 Football Bingo FF 10-11 Touchdown Trivia FF 12 Answer Key FF 13 Football Facts and Figures Canton, Ohio and the National Football League ach year, approximately 250,000 fans from all over the world visit the Pro Football Hall of Fame in Canton, Ohio. The museum’s guest register reveals that in a year’s time, visitors come from all fifty Estates and from sixty to seventy foreign countries. Many wonder why the Hall of Fame is located in this small northeast Ohio city. Often, museums are built in locations that have historical significance to their subject matter. The Pro Football Hall of Fame is no exception. Canton’s ties to pro football began long before the Hall of Fame was built in 1963. On September 17, 1920, a meeting was held in an automobile showroom in downtown Canton. It was at this time that the American Professional Football Association was formed. Two years later, the league changed its name to the National Football League. Today, fans follow teams like the Dallas Cowboys, San Francisco 49ers, and the Miami Dolphins. But, in 1920, none of those teams existed. -

Canadian Guideline on Concussion in Sport Canadian Guideline on Concussion in Sport
Canadian Guideline on Concussion in Sport Canadian Guideline on Concussion in Sport July 2017 Funding provided by: Public Health Agency of Canada The views expressed herein do not necessarily represent the views of the Public Health Agency of Canada. Suggested citation: Parachute. (2017). Canadian Guideline on Concussion in Sport. Toronto: Parachute. © Parachute – Leaders in Injury Prevention, 2017 Contents EXPERT ADVISORY COMMITTEE ON CONCUSSIONS 5 ADDITIONAL REVIEW AND FEEDBACK 6 PARACHUTE PROJECT TEAM 6 OVERVIEW 7 PURPOSE 7 APPLICATION TO NON-SPORT RELATED CONCUSSION 7 WHO SHOULD USE THIS GUIDELINE? 7 HOW TO READ THIS GUIDELINE 8 ROLE OF CLINICAL JUDGMENT 8 KEY TERM DEFINITIONS 8 GUIDELINE RECOMMENDATIONS 11 1. PRE-SEASON EDUCATION 12 2. HEAD INJURY RECOGNITION 13 3. ONSITE MEDICAL ASSESSMENT 14 4. MEDICAL ASSESSMENT 16 5. CONCUSSION MANAGEMENT 17 6. MULTIDISCIPLINARY CONCUSSION CARE 20 7. RETURN TO SPORT 21 CANADIAN SPORT CONCUSSION PATHWAY 23 GUIDELINE DEVELOPMENT PROCESS 25 EVIDENCE 25 STAKEHOLDER CONSULTATION 25 UPDATES TO THIS GUIDELINE 26 APPENDIX: DOCUMENTS & TOOLS 27 PRE-SEASON CONCUSSION EDUCATION SHEET 29 MEDICAL ASSESSMENT LETTER 31 MEDICAL CLEARANCE LETTER 33 CONCUSSION RECOGNITION TOOL – 5TH EDITION (CRT5) 35 SPORT CONCUSSION ASSESSMENT TOOL – 5TH EDITION (SCAT5) 37 CHILD SPORT CONCUSSION ASSESSMENT TOOL – 5TH EDITION (CHILD SCAT5) 45 Contributors Expert Advisory Committee on Concussions Dr. Charles Tator, Co-Chair, MD, PhD, FRCSC, FACS Professor of Neurosurgery, University of Toronto Division of Neurosurgery and Canadian Concussion Centre, Toronto Western Hospital Dr. Michael Ellis, Co-Chair, BSc, MD, FRCSC Medical Director, Pan Am Concussion Program Dept. of Surgery and Pediatrics and Section of Neurosurgery, University of Manitoba Scientist, Children’s Hospital Research Institute of Manitoba Co-director, Canada North Concussion Network Dr. -

Bioenergetics and Time-Motion Analysis of Competitive Basketball
University of Nebraska at Omaha DigitalCommons@UNO Student Work 6-1-2005 Bioenergetics and time-motion analysis of competitive basketball Kenji Narazaki University of Nebraska at Omaha Follow this and additional works at: https://digitalcommons.unomaha.edu/studentwork Recommended Citation Narazaki, Kenji, "Bioenergetics and time-motion analysis of competitive basketball" (2005). Student Work. 758. https://digitalcommons.unomaha.edu/studentwork/758 This Thesis is brought to you for free and open access by DigitalCommons@UNO. It has been accepted for inclusion in Student Work by an authorized administrator of DigitalCommons@UNO. For more information, please contact [email protected]. BIOENERGETICS AND TIME-MOTION ANALYSIS OF COMPETITIVE BASKETBALL A Thesis Presented to the School of Health, Physical Education, and Recreation and the Faculty of the Graduate College University of Nebraska In Partial Fulfillment of the Requirements for the Degree Master of Science University of Nebraska at Omaha by Kenji Narazaki June 2005 UMI Number: EP73298 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. Dissertation Publishing UMI EP73298 Published by ProQuest LLC (2015). Copyright in the Dissertation held by the Author. Microform Edition © ProQuest LLC. All rights reserved. This work is protected against unauthorized copying under Title 17, United States Code ProQuest LLC. 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106-1346 1 THESIS ACCEPTANCE Acceptance for the faculty of the Graduate College, University of Nebraska, in partial fulfillment of the requirements for the degree Master of Science in Exercise Science, University of Nebraska at Omaha. -

CYO West Contra Costa – WCC/Northern League 2019-2020 Basketball Rules
CYO West Contra Costa – WCC/Northern League 2019-2020 Basketball Rules Rule Book Play shall be governed in order of priority, First by WCC/Northern rules listed below, Second by Diocese of Oakland CYO basketball rules and Third by the current edition of the National Federation of State High School Association Rule Book for boy’s and girl’s competitions. Team Rosters Original team rosters complete with coach, athletic director and principal or pastor signatures are due at a scheduled Roster Review Meeting. The League Executive Board (the Board) will set a date for such a meeting prior to league play for both the boys’ and girls’ seasons. When necessary, rosters must be accompanied by copies of birth certificates, CCD letters signed by the religious director or coordinator, and/or proof of residency (current utility bill). All new non-school players must show proof of residency. Rosters must consist of 7 or more players to constitute a valid team. The Board may grant approval for teams of 6 after reviewing the roster. AD’s will be given the day before the first league game to correct rosters. AD’s must notify all members of the Board of any added players for final roster approval. After the first played game, only verified, eligible players will be allowed to play. Any games played with illegal players or players not listed on the official roster will become forfeits. Teams who do not submit rosters by the specified deadline will forfeit all games played until approved rosters are turned in. Player Eligibility The Board will allow any player to play in the league who meets the player eligibility as described in the Diocese of Oakland CYO Athletic Manual with the additional restriction: Any team consisting of more boundary players than school and CCD players will require approval from the Board. -

Nysphsaa Rules & Regulations
Education Through Interscholastic Athletics 2017 HANDBOOK MEMBER NYSPHSAA TABLE OF CONTENTS CLICK ON TOPIC BELOW RECENT REVISIONS TO NYSPHSAA HANDBOOK ...................................................................................................... 5 ADMINISTRATION .................................................................................................................................................................. 7 HISTORY OF NYSPHSAA, INC. ........................................................................................................................................ 8 NYSED COMMISSIONER’S REGULATIONS .................................................................................................................. 11 NYSED TOOLKIT ............................................................................................................................................................... 11 ATHLETIC PLACEMENT PROCESS ............................................................................................................................ 11 COACHING CERTIFICATION ......................................................................................................................................... 11 MIXED COMPETITION .................................................................................................................................................... 11 REGULATION 135.4 ........................................................................................................................................................ -
Rationale for Collaborative Action
Zero Tolerance for Concussions and other Neurotrauma in Ice Hockey: Rationale for Collaborative Action Aynsley M. Smith, RN, PhD, Michael J. Stuart, MD, David Dodick, MD, Matthew C Sorenson, JD, MA Jonathon T Finnoff, DO, David Krause, PT, DSc The Mayo Clinic Sports Medicine Center Hockey Research Team This document provides an overview of some research across sectors that might segue to an empirical basis for discussion by Summit attendees who seek a collaborative, multi sector solution to addressing the concussion challenge in hockey. 1 Preface We would like to state at the outset that Aynsley, Michael and our ice hockey research team has been humbled by the fantastic support of the faculty, steering and planning committees. Many of you have been addressing concussions your entire careers, are extremely well known and are well published in concussions in hockey and in related neurotrauma. The purpose of the Ice Hockey Summit: Action on Concussion is to provide background information to attendees so they can make informed decisions on the action plan needed to address the concussion epidemic. This pre-reading has been written to help ensure that we all have a basic understanding of the many dimensions of concussion. Hopefully, the six sectors identified and discussed in the pre-reading will serve as the studs in a framework for a collaborative action plan toward a solution. This document is not an exhaustive review of the influences on concussion. Our paradigm is influenced and simultaneously limited by our knowledge and professional experience. In many cases we are aware we have only cited only one or two publications written by our steering committee members. -

WYA Basketball Playing Rules
WYA Basketball Playing Rules Divisions: Kids: (K4, K5, 1st) Coed Pee Wee: (2nd, 3rd)(Also 4th for girls league) Midget Boys: (4th, 5th) Minor Boys: (Junior High 6th -8th) Minor Girls: (5th grade-8th Grade) A. Players will be placed in a division as of their age and grade on 01AUGxx. Children will play in their age division, unless approved by the Basketball Director. Exceptions will be made and age groups are subject to change due to signup numbers. B. Unless otherwise specified, games shall be played under the official S.C. High School basketball rules. C. Kids/ Pee Wees-27.5” ball, 8’ goal, 7’ free throw Midget Boys/ Minor Girls—28.5” ball, regulation goal, regulation free throw (may cross line on follow through) Minor/ Junior Boys—29.5” ball, regulation goal, regulation free throw D. Conduct of coaches: Each coach’s role is to be a positive role model to his/her team, set a proper example, and understand the score comes second to the safety and wellbeing of the players. Verbal or physical abuse against the opposing team, referees, or spectators will not be tolerated. Teaching of fundamentals and the spirit of the game are our goals over winning. Coaches set the tone. E. Conduct of fans: Each coach will be responsible for the conduct of his or her team’s fans. Coaches may be asked by referees, Coordinators, Board Members, or the Basketball Director to speak to one of their team’s fans about their conduct. This will be done first to prevent a conflict between fans and WYA.