Alcohol and Substance Use in Pregnancy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Alcohol and Pregnancy 'One Drink' Community Toolkit Campaign Assets and Resources for You to Use in Your Community and Workplace
Alcohol and Pregnancy 'One Drink' Community toolkit Campaign assets and resources for you to use in your community and workplace. Contents 03 ALCOHOL AND PREGNANCY 'ONE DRINK' CAMPAIGN 04 EVIDENCE TO SUPPORT THE CAMPAIGN AND KEY MESSAGES 05 STATEWIDE CAMPAIGN SCHEDULE 06 CAMPAIGN MATERIALS AND RESOURCES TO USE LOCALLY 14 EXTENDING THE CAMPAIGN IN YOUR LOCAL COMMUNITY 15 USEFUL CONTACTS ALCOHOL.THINK AGAIN | COMMUNITY KIT 2 Alcohol and Pregnancy 'One Drink' campaign ABOUT THIS TOOLKIT ABOUT THIS CAMPAIGN This toolkit provides information, campaign materials and The Alcohol.Think Again public education program aims Key messages strategies for professional and community groups to assist in to reduce alcohol-related harm in the Western Australian • The placenta does not protect a baby from alcohol. decreasing risky drinking and related harm in Western Australia. community by using a mass reach social marketing strategy to • Any amount of alcohol a mother drinks, the baby drinks. provide information about health risks from drinking alcohol, These resources have been developed to assist you to extend consistent with the National Health and Medical Research Council • There is no safe amount or time to drink alcohol during the reach of the campaign in your community using materials (NHMRC). pregnancy. consistent with the statewide Alcohol.Think Again, • Women who are pregnant or planning pregnancy should Alcohol and Pregnancy campaign titled 'One Drink’. The 'One Drink' campaign aims to increase the proportion of the not drink alcohol. Western Australian community who are aware that there is no As a local stakeholder, you may wish to use one or all of the safe amount or time to drink alcohol when pregnant, and that supplied materials and strategies in this toolkit. -

Childbirth Education Booklet
Childbirth Education Contents Normal Discomforts of Pregnancy 2 Call Your Doctor 4 Late Pregnancy 5 Labor: Stage 1 6 Labor: Stages 2 & 3 8 Breastfeeding in the Hospital 9 Breathing Techniques 10 Birth Plans 10 Labor Positions 11 How Your Partner and Doula Can Help 13 Packing for the Hospital 15 Normal Discomforts of Pregnancy Fatigue Backache • Listen to your body, take naps, get extra rest • Maintain correct posture • Do pelvic tilt exercises while standing and on hands Stuffy Nose and knees • Warm compresses to nose • While on all fours, crawl forwards and backwards, • Cool mist humidifier in your home or rock, and do pelvic tilts bedroom at night • When picking up something lift with your legs to protect your back Shortness of Breath • Don’t stay that way, slow down and catch your breath • For prolonged standing, elevate 1 foot on a step stool • Sleep propped up with pillows or in recliner • Receive back massages • Maintain correct posture Dribble Urine • Moderate intensity exercising (walking, stationary • Do Kegel exercises – at least 50 a day bike, swim, flexibility moves) (do 10 every time you wash your hands) • How can you tell if you are dribbling urine or your Heartburn/Nausea water broke? Call your OB or midwife, and remember • Don’t eat 3 big meals a day, eat 5-6 smaller meals this acronym: • Drink 8 cups of water a day COAT. C=color, O=odor, A=amount, T=time. • Have dry crackers/cereal to nibble on–keep in purse and at bedside • Don’t let stomach become empty • Eat well balanced diet–vitamin B may help to decrease • Avoid -

The Effects of Alcohol in Newborns Efeitos Do Álcool No Recém-Nascido
REVIEW The effects of alcohol in newborns Efeitos do álcool no recém-nascido Maria dos Anjos Mesquita* ABSTRACT alcoólicas leva a prejuízos individuais, para a sua família e para The purpose of this article was to present a review of the effects toda a sociedade. Apesar disso, a dificuldade do seu diagnóstico e of alcohol consumption by pregnant mothers on their newborn. a inexperiência dos profissionais de saúde faz com que o espectro Definitions, prevalence, pathophysiology, clinical features, diagnostic dessas lesões seja pouco lembrado e até desconhecido. As lesões criteria, follow-up, treatment and prevention were discussed. A causadas pela ação do álcool no concepto são totalmente prevenidas search was performed in Medline, LILACS, and SciELO databases se a gestante não consumir bebidas alcoólicas durante a gestação. using the following terms: “fetus”, “newborn”, “pregnant woman”, Assim, é fundamental a detecção das mulheres consumidoras “alcohol”, “alcoholism”, “fetal alcohol syndrome”, and “alcohol- de álcool durante a gravidez e o desenvolvimento de programas related disorders”. Portuguese and English articles published from específicos de alerta sobre as consequências do álcool durante a 2000 to 2009 were reviewed. The effects of alcohol consumed by gestação e amamentação. pregnant women on newborns are extremely serious and occur frequently; it is a major issue in Public Health worldwide. Fetal alcohol Descritores: Bebidas alcoólicas/efeitos adversos; Feto; Recém-nascido; spectrum disorders cause harm to individuals, their families, and the Síndrome alcoólica fetal; Transtornos relacionados ao uso de álcool entire society. Nevertheless, diagnostic difficulties and inexperience of healthcare professionals result in such damage, being remembered rarely or even remaining uncovered. -

Care During Pregnancy and Delivery ACCESSIBLE, QUALITY HEALTH CARE DURING PREGNANCY and DELIVERY
Care during Pregnancy and Delivery ACCESSIBLE, QUALITY HEALTH CARE DURING PREGNANCY AND DELIVERY Why It’s Important Having a healthy pregnancy and access to quality birth facilities are the best ways to promote a healthy birth and have a thriving newborn. Getting early and regular prenatal care is vital. Prenatal care is the health care that women receive during their entire pregnancy. Prenatal care is more than doctor’s visits and ultrasounds; it is an opportunity to improve the overall well-being and health of the mom which directly affects the health of her baby. Prenatal visits give parents a chance to ask questions, discuss concerns, treat complications in a timely manner, and ensure that mom and baby are safe during pregnancy and delivery. Receiving quality prenatal care can have positive effects long after birth for both the mother and baby. When it is time for the mother to give birth, having access to safe, high quality birth facilities is critical. Early prenatal care, starting in the 1st trimester, is crucial to the health of mothers and babies. But more important than just initiating early prenatal care is receiving adequate prenatal care, having the appropriate number of prenatal care visits at the appropriate intervals throughout the pregnancy. Babies of mothers who do not get prenatal care are three times more likely to be born low birth weight and five times more likely to die than those born to mothers who do get care.1 In 2017 in Minnesota, only 77.1 percent of women received prenatal care within their first trimester of pregnancy. -

18 Percent of Pregnant Women Drink Alcohol During Early
National Survey on Drug Use and Health The NSDUH Report Data Spotlight September 9, 2013 18 Percent of Pregnant VA60 Women Drink Alcohol during Early Pregnancy Women who drink alcohol while pregnant increase the risk that their infants will have physical, learning, and/or behavior problems, including Fetal Alcohol Spectrum Disorder (FASD).1 These problems are caused by alcohol and can be lifelong. Combined 2011 to 2012 data from the National Survey on Drug Use and Health (NSDUH) show that 8.5 percent of pregnant women aged 15 to 44 drank alcohol in the past month (Figure). Also, 2.7 percent binge drank.2 Among women aged 15 to 44 who were not pregnant, 55.5 percent drank alcohol in the past month, and 24.7 percent binge drank. Most alcohol use by pregnant women occurred during the first trimester. Alcohol use was lower during the second and third trimesters than during the first (4.2 and 3.7 percent vs. 17.9 percent). These findings suggest that many pregnant women are getting the message and not drinking alcohol. Alcohol can disrupt fetal development at Past Month Alcohol Use and Binge Alcohol Use among Pregnant Women Aged any stage during a pregnancy, even before a 15 to 44, Overall and by Trimester*: 2011 and 2012 woman knows she is pregnant.3 If a woman is pregnant, there is no known amount 20 Any Alcohol Use 17.9 or type of alcohol that is safe for her to Binge Alcohol Use drink.4 To prevent problems like FASD, a woman who is pregnant or likely to become 15 pregnant should not drink alcohol. -

Massive Subchorionic Haemorrhage: a Rare Case Report Associated with Secondary PPH Due to Uterine Artery Pseudoaneurysm
International Journal of Reproduction, Contraception, Obstetrics and Gynecology Arumaikannu J et al. Int J Reprod Contracept Obstet Gynecol. 2017 Oct;6(10):4723-4726 www.ijrcog.org pISSN 2320-1770 | eISSN 2320-1789 DOI: http://dx.doi.org/10.18203/2320-1770.ijrcog20174475 Case Report Massive subchorionic haemorrhage: a rare case report associated with secondary PPH due to uterine artery pseudoaneurysm J. Arumaikannu*, S. Usha Rani, T. S. Aarifa Thasleem Institute of Obstetrics and Gynecology, Egmore, Chennai, Tamil Nadu, India Received: 08 August 2017 Accepted: 04 September 2017 *Correspondence: Dr. J. Arumaikannu, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Massive subchorionic hemorrhage is a rare but serious condition in pregnancy in which a large amount of blood, mainly maternal collects between the uterine wall and the chorionic membrane and may leak through the cervical canal. Although many associations have been reported, an underlying etiology has not been elucidated. Association of massive subchorionic hemorrhage with thrombophilias have been reported in few articles. We are reporting a case of massive subchorionic hemorrhage presented at 13 weeks of gestation associated with secondary post-partum hemorrhage due to uterine artery pseudoaneurysm. Keywords: Massive subchorionic haemorrhage, Secondary PPH, Uterine artery pseudoaneurysm INTRODUCTION hemorrhage in the second trimester may also compromise maternal health.2,3 During pregnancy, minor degrees of haemorrhage on the chorionic plate surface of the placenta are commonly A subchorionic hemorrhage can be considered large or identified on ultrasound assessment. -

A Guide to Obstetrical Coding Production of This Document Is Made Possible by Financial Contributions from Health Canada and Provincial and Territorial Governments
ICD-10-CA | CCI A Guide to Obstetrical Coding Production of this document is made possible by financial contributions from Health Canada and provincial and territorial governments. The views expressed herein do not necessarily represent the views of Health Canada or any provincial or territorial government. Unless otherwise indicated, this product uses data provided by Canada’s provinces and territories. All rights reserved. The contents of this publication may be reproduced unaltered, in whole or in part and by any means, solely for non-commercial purposes, provided that the Canadian Institute for Health Information is properly and fully acknowledged as the copyright owner. Any reproduction or use of this publication or its contents for any commercial purpose requires the prior written authorization of the Canadian Institute for Health Information. Reproduction or use that suggests endorsement by, or affiliation with, the Canadian Institute for Health Information is prohibited. For permission or information, please contact CIHI: Canadian Institute for Health Information 495 Richmond Road, Suite 600 Ottawa, Ontario K2A 4H6 Phone: 613-241-7860 Fax: 613-241-8120 www.cihi.ca [email protected] © 2018 Canadian Institute for Health Information Cette publication est aussi disponible en français sous le titre Guide de codification des données en obstétrique. Table of contents About CIHI ................................................................................................................................. 6 Chapter 1: Introduction .............................................................................................................. -
Turning Your Breech Baby to a Head-Down Position (External Cephalic Version)
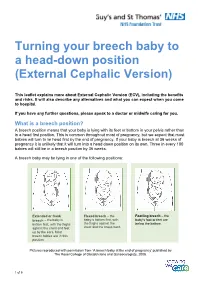
Turning your breech baby to a head-down position (External Cephalic Version) This leaflet explains more about External Cephalic Version (ECV), including the benefits and risks. It will also describe any alternatives and what you can expect when you come to hospital. If you have any further questions, please speak to a doctor or midwife caring for you. What is a breech position? A breech position means that your baby is lying with its feet or bottom in your pelvis rather than in a head first position. This is common throughout most of pregnancy, but we expect that most babies will turn to lie head first by the end of pregnancy. If your baby is breech at 36 weeks of pregnancy it is unlikely that it will turn into a head down position on its own. Three in every 100 babies will still be in a breech position by 36 weeks. A breech baby may be lying in one of the following positions: Extended or frank Flexed breech – the Footling breech – the breech – the baby is baby is bottom first, with baby’s foot or feet are bottom first, with the thighs the thighs against the below the bottom. against the chest and feet chest and the knees bent. up by the ears. Most breech babies are in this position. Pictures reproduced with permission from ‘A breech baby at the end of pregnancy’ published by The Royal College of Obstetricians and Gynaecologists, 2008. 1 of 5 What causes breech? Breech is more common in women who are expecting twins, or in women who have a differently-shaped womb (uterus). -

Drug Use and Pregnancy
Rochester Institute of Technology RIT Scholar Works Theses 7-28-1999 Drug use and pregnancy Kimberly Klapmust Follow this and additional works at: https://scholarworks.rit.edu/theses Recommended Citation Klapmust, Kimberly, "Drug use and pregnancy" (1999). Thesis. Rochester Institute of Technology. Accessed from This Thesis is brought to you for free and open access by RIT Scholar Works. It has been accepted for inclusion in Theses by an authorized administrator of RIT Scholar Works. For more information, please contact [email protected]. ROCHESTER INSTITUTE OF TECHNOLOGY A Thesis Submitted to the Faculty of The College of Imaging Arts and Sciences In Candidacy for the Degree of MASTER OF FINE ARTS Drug Use and Pregnancy by Kimberly A. Klapmust July 28, 1999 Approvals Adviser: Robert Wabnitz Date: Associate Adviser. Dr. Nancy Wanek ~)14 Date: \\.\,, c Associate Advisor: Glen Hintz Date ]I-I, zJ Cf9 I 7 Department ChaiIWrson: _ Dale: 1//17._/c; '1 I, , hereby deny permission to the Wallace Memorial library of RIT to reproduce my thesis in whole or in part. Any reproduction will not be for commercial use or profit. INTRODUCTION Human development is a remarkably complex process whereby the union of two small cells can after a period of time give rise to a new human being, complete with vital organs, bones, muscles, nerves, blood vessels, and much more. Considering the intricacy of the developmental process, it is indeed miraculous that most babies are born healthy. Some children, however, are born with abnormalities. Environmental agents, such as drugs, are responsible for some of these abnormalities. -

The Law of Placenta
The Law of Placenta Mathilde Cohent ABSTRACT: Of the forms of reproductive labor in which legal scholars have been interested, placenta, the organ developed during pregnancy, has been overlooked. As placenta becomes an object of value for a growing number of individuals, researchers, clinicians, biobanks, and biotech companies, among others, its cultural meaning is changing. At the same time, these various constituencies may be at odds. Some postpartum parents and their families want to repossess their placenta for personal use, while third parties use placentas for a variety of research, medical, and commercial purposes. This Article contributes to the scholarship on reproductive justice and agency by asking who should have access to placentas and under what conditions. The Article emphasizes the insufficient protection the law affords pregnant people wishing to decide what happens to their placenta. Generally considered clinical waste under federal and state law, placental tissue is sometimes made inaccessible to its producers on the ground that it is infectious at the same time as it is made available to third parties on the ground that placenta is discarded and de-identified tissue. Less privileged people who lack the ability to shop for obstetric and other pregnancy-related services that allow them to keep their placentas are at a disadvantage in this chain of supply and demand. While calling for further research on the modus operandi of placenta markets and how pregnant people think about them, this Article concludes that lawmakers should take steps to protect decision-making autonomy over placental labor and offers a range of proposals to operationalize this idea. -

14. Management of Diabetes in Pregnancy: Standards of Medical
Diabetes Care Volume 42, Supplement 1, January 2019 S165 14. Management of Diabetes in American Diabetes Association Pregnancy: Standards of Medical Care in Diabetesd2019 Diabetes Care 2019;42(Suppl. 1):S165–S172 | https://doi.org/10.2337/dc19-S014 14. MANAGEMENT OF DIABETES IN PREGNANCY The American Diabetes Association (ADA) “Standards of Medical Care in Diabetes” includes ADA’s current clinical practice recommendations and is intended to provide the components of diabetes care, general treatment goals and guidelines, and tools to evaluate quality of care. Members of the ADA Professional Practice Committee, a multidisciplinary expert committee, are responsible for updating the Standards of Care annually, or more frequently as warranted. For a detailed description of ADA standards, statements, and reports, as well as the evidence-grading system for ADA’s clinical practice recommendations, please refer to the Standards of Care Introduction. Readers who wish to comment on the Standards of Care are invited to do so at professional.diabetes.org/SOC. DIABETES IN PREGNANCY The prevalence of diabetes in pregnancy has been increasing in the U.S. The majority is gestational diabetes mellitus (GDM) with the remainder primarily preexisting type 1 diabetes and type 2 diabetes. The rise in GDM and type 2 diabetes in parallel with obesity both in the U.S. and worldwide is of particular concern. Both type 1 diabetes and type 2 diabetes in pregnancy confer significantly greater maternal and fetal risk than GDM, with some differences according to type of diabetes. In general, specific risks of uncontrolled diabetes in pregnancy include spontaneous abortion, fetal anomalies, preeclampsia, fetal demise, macrosomia, neonatal hypoglycemia, and neonatal hyperbilirubinemia, among others. -

If You Are Pregnant: INFORMATION on FETAL DEVELOPMENT, ABORTION and ALTERNATIVES August 2019
If You Are Pregnant: INFORMATION ON FETAL DEVELOPMENT, ABORTION AND ALTERNATIVES August 2019 IF YOU ARE PREGNANT: INFORMATION ON FETAL DEVELOPMENT, ABORTION AND ALTERNATIVES If You Are Pregnant: Information on Fetal Development, Abortion and Alternatives Resources used by the Minnesota Department of Health for this publication are Human Embryology and Developmental Biology, Fifth Edition, 2014; Larsen’s Human Embryology, Fifth Edition, 2014; The Developing Human, 10th Edition, 2016; and In the Womb, 2006. The photographs in this booklet are credited to Lennart Nilsson/TT Images and are used by permission; except for week 38 copyright Minnesota Department of Health. The illustrations found throughout this booklet were created by Peg Gerrity, Houston, Texas. Copyright: http://www.peggerrity.com. Minnesota Department of Health Division of Child and Family Health PO Box 64882 St. Paul, MN 55164-0882 651-201-3580 Women's Right to Know (https://www.health.state.mn.us/people/wrtk/index.html) Upon request, this material will be made available in an alternative format such as large print, Braille or audio recording. Printed on recycled paper. 2 IF YOU ARE PREGNANT: INFORMATION ON FETAL DEVELOPMENT, ABORTION AND ALTERNATIVES Contents If You Are Pregnant: INFORMATION ON FETAL DEVELOPMENT, ABORTION AND ALTERNATIVES............................................................................................................................. 1 Introduction ...............................................................................................................................