2012 BRC BW Day One Cover Page
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
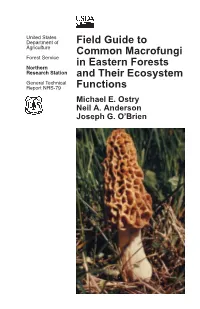
Field Guide to Common Macrofungi in Eastern Forests and Their Ecosystem Functions
United States Department of Field Guide to Agriculture Common Macrofungi Forest Service in Eastern Forests Northern Research Station and Their Ecosystem General Technical Report NRS-79 Functions Michael E. Ostry Neil A. Anderson Joseph G. O’Brien Cover Photos Front: Morel, Morchella esculenta. Photo by Neil A. Anderson, University of Minnesota. Back: Bear’s Head Tooth, Hericium coralloides. Photo by Michael E. Ostry, U.S. Forest Service. The Authors MICHAEL E. OSTRY, research plant pathologist, U.S. Forest Service, Northern Research Station, St. Paul, MN NEIL A. ANDERSON, professor emeritus, University of Minnesota, Department of Plant Pathology, St. Paul, MN JOSEPH G. O’BRIEN, plant pathologist, U.S. Forest Service, Forest Health Protection, St. Paul, MN Manuscript received for publication 23 April 2010 Published by: For additional copies: U.S. FOREST SERVICE U.S. Forest Service 11 CAMPUS BLVD SUITE 200 Publications Distribution NEWTOWN SQUARE PA 19073 359 Main Road Delaware, OH 43015-8640 April 2011 Fax: (740)368-0152 Visit our homepage at: http://www.nrs.fs.fed.us/ CONTENTS Introduction: About this Guide 1 Mushroom Basics 2 Aspen-Birch Ecosystem Mycorrhizal On the ground associated with tree roots Fly Agaric Amanita muscaria 8 Destroying Angel Amanita virosa, A. verna, A. bisporigera 9 The Omnipresent Laccaria Laccaria bicolor 10 Aspen Bolete Leccinum aurantiacum, L. insigne 11 Birch Bolete Leccinum scabrum 12 Saprophytic Litter and Wood Decay On wood Oyster Mushroom Pleurotus populinus (P. ostreatus) 13 Artist’s Conk Ganoderma applanatum -

XXXV International Congress of the European Association of Poisons Centres and Clinical Toxicologists (EAPCCT) 26–29 May 2015, St Julian's, Malta
Clinical Toxicology ISSN: 1556-3650 (Print) 1556-9519 (Online) Journal homepage: http://www.tandfonline.com/loi/ictx20 XXXV International Congress of the European Association of Poisons Centres and Clinical Toxicologists (EAPCCT) 26–29 May 2015, St Julian's, Malta To cite this article: (2015) XXXV International Congress of the European Association of Poisons Centres and Clinical Toxicologists (EAPCCT) 26–29 May 2015, St Julian's, Malta, Clinical Toxicology, 53:4, 233-403, DOI: 10.3109/15563650.2015.1024953 To link to this article: http://dx.doi.org/10.3109/15563650.2015.1024953 Published online: 26 Mar 2015. Submit your article to this journal Article views: 3422 View related articles View Crossmark data Citing articles: 2 View citing articles Full Terms & Conditions of access and use can be found at http://www.tandfonline.com/action/journalInformation?journalCode=ictx20 Download by: [UPSTATE Medical University Health Sciences Library] Date: 28 December 2016, At: 10:31 Clinical Toxicology (2015), 53, 233–403 Copyright © 2015 Informa Healthcare USA, Inc. ISSN: 1556-3650 print / 1556-9519 online DOI: 10.3109/15563650.2015.1024953 ABSTRACTS XXXV International Congress of the European Association of Poisons Centres and Clinical Toxicologists (EAPCCT) 26–29 May 2015, St Julian ’ s, Malta 1. Modelling dose-concentration-response Introduction: The American Association of Poison Control Cen- ters (AAPCC) published its fi rst annual report in 1983. Call data Ursula Gundert-Remy from sixteen US poison centers was chronicled in that report. Seven submitted data for the entire year. By July 2000, 63 centers Institute for Clinical Pharmacology and Toxicology, Charit é were part of the national poison center system, but only 59 submit- Medical School, Berlin, Germany ted data for the full year. -
Theoretical Problem Icho 2018
19th – 29th July 2018 Bratislava, SLOVAKIA Prague, CZECH REPUBLIC www.50icho.eu THEORETICAL PROBLEMS Country: Name as in passport: Student code: Language: 50th IChO 2018 International Chemistry Olympiad SLOVAKIA & CZECH REPUBLIC BACK TO WHERE IT ALL BEGAN XXX-X INTERNATIONAL CHEMISTRY OLYMPIAD / SLOVAKIA & CZECH REPUBLIC, 2018 Table of Contents Instructions ...................................................................................................................................... 2 Physical constants and equations ................................................................................................... 3 Problem 1. DNA .............................................................................................................................. 5 Problem 2. Repatriation of remains in the middle ages .................................................................. 14 Problem 3. Emerging electro-mobility ............................................................................................ 22 Problem 4. Column chromatography of radioactive copper ........................................................... 30 Problem 5. Bohemian garnet ......................................................................................................... 34 Problem 6. Let’s go mushrooming ................................................................................................. 41 Problem 7. Cidofovir ...................................................................................................................... 47 -

Medical Management of Biological Casualties Handbook
USAMRIID’s MEDICAL MANAGEMENT OF BIOLOGICAL CASUALTIES HANDBOOK Sixth Edition April 2005 U.S. ARMY MEDICAL RESEARCH INSTITUTE OF INFECTIOUS DISEASES FORT DETRICK FREDERICK, MARYLAND Emergency Response Numbers National Response Center: 1-800-424-8802 or (for chem/bio hazards & terrorist events) 1-202-267-2675 National Domestic Preparedness Office: 1-202-324-9025 (for civilian use) Domestic Preparedness Chem/Bio Helpline: 1-410-436-4484 or (Edgewood Ops Center – for military use) DSN 584-4484 USAMRIID’s Emergency Response Line: 1-888-872-7443 CDC'S Emergency Response Line: 1-770-488-7100 Handbook Download Site An Adobe Acrobat Reader (pdf file) version of this handbook can be downloaded from the internet at the following url: http://www.usamriid.army.mil USAMRIID’s MEDICAL MANAGEMENT OF BIOLOGICAL CASUALTIES HANDBOOK Sixth Edition April 2005 Lead Editor Lt Col Jon B. Woods, MC, USAF Contributing Editors CAPT Robert G. Darling, MC, USN LTC Zygmunt F. Dembek, MS, USAR Lt Col Bridget K. Carr, MSC, USAF COL Ted J. Cieslak, MC, USA LCDR James V. Lawler, MC, USN MAJ Anthony C. Littrell, MC, USA LTC Mark G. Kortepeter, MC, USA LTC Nelson W. Rebert, MS, USA LTC Scott A. Stanek, MC, USA COL James W. Martin, MC, USA Comments and suggestions are appreciated and should be addressed to: Operational Medicine Department Attn: MCMR-UIM-O U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID) Fort Detrick, Maryland 21702-5011 PREFACE TO THE SIXTH EDITION The Medical Management of Biological Casualties Handbook, which has become affectionately known as the "Blue Book," has been enormously successful - far beyond our expectations. -

Treatment of Social Phobia with Antidepressants
Antidepressants for Social Phobia Treatment of Social Phobia With Antidepressants Franklin R. Schneier, M.D. This article reviews evidence for the utility of antidepressant medications in the treatment of social phobia. Monoamine oxidase inhibitors (MAOIs) were the first antidepressants shown to be effective © Copyrightfor social phobia, but 2001dietary restrictions Physicians and a relatively Postgraduate high rate of adverse effects Press, often relegate Inc. MAOIs to use after other treatments have been found ineffective. Reversible inhibitors of monoamine oxidase (RIMAs) hold promise as safer alternatives to MAOIs, but RIMAs may be less effective and are currently unavailable in the United States. Selective serotonin reuptake inhibitors (SSRIs), of which paroxetine has been the best studied in social phobia to date, have recently emerged as a first- line treatment for the generalized subtype of social phobia. The SSRIs are well tolerated and consis- tently have been shown to be efficacious in controlled trials. (J Clin Psychiatry 2001;62[suppl 1]:43–48) arly evidence that antidepressantsOne might personal have utility copy maypressant be printed treatment of other anxiety disorders, such as panic E in the treatment of social phobia emerged in the disorder and obsessive-compulsive disorder. In particular, 1970s when studies found efficacy for monoamine oxidase the high rate of comorbidity of anxiety disorders with de- inhibitors (MAOIs) in patient samples that included both pression3 makes treatment with antidepressants an efficient -

Batrachotoxin Time-Resolved Absorption And
Dental, Oral and Maxillofacial Research Mini Review ISSN: 2633-4291 Batrachotoxin time-resolved absorption and resonance FT-IR and raman biospectroscopy and density functional theory (DFT) investigation of vibronic-mode coupling structure in vibrational spectra analysis: A spectroscopic study on an anti-gum cancer drug Alireza Heidari1,2*, Jennifer Esposito1 and Angela Caissutti1 1Faculty of Chemistry, California South University, 14731 Comet St. Irvine, CA 92604, USA 2American International Standards Institute, Irvine, CA 3800, USA Abstract Gum cancers are cancers that arise from the gum. They are due to the development of abnormal cells that have the ability to invade or spread to other parts of the body. There are three main types of gum cancers: basal-cell gum cancer (BCC), squamous-cell gum cancer (SCC) and melanoma. Batrachotoxin (BTX) is an anti- gum cancer extremely potent cardiotoxic and neurotoxic steroidal alkaloid found in certain species of beetles, birds, and frogs. Batrachotoxin was derived from the Greek word βάτραχος bátrachos "frog". Structurally-related chemical compounds are often referred to collectively as batrachotoxins. It is an extremely poisonous alkaloid. In certain frogs this alkaloid is present mostly on the gum. Such frogs are among those used for poisoning darts. Batrachotoxin binds to and irreversibly opens the sodium channels of nerve cells and prevents them from closing, resulting in paralysis-no antidote is known. Parameters such as FT -IR and Raman vibrational wavelengths and intensities for single crystal Batrachotoxin are calculated using density functional theory and were compared with empirical results. The investigation about vibrational spectrum of cycle dimers in crystal with carboxyl groups from each molecule of acid was shown that it leads to create Hydrogen bonds for adjacent molecules. -
![Lithium Carbonate; [2] Lithium Chloride; [3] Lithium Hydroxide](https://docslib.b-cdn.net/cover/7768/lithium-carbonate-2-lithium-chloride-3-lithium-hydroxide-617768.webp)
Lithium Carbonate; [2] Lithium Chloride; [3] Lithium Hydroxide
CLH REPORT FOR LITHIUM SALTS CLH report Proposal for Harmonised Classification and Labelling Based on Regulation (EC) No 1272/2008 (CLP Regulation), Annex VI, Part 2 International Chemical Identification: [1] Lithium carbonate; [2] lithium chloride; [3] lithium hydroxide EC Number: [1] 209-062-5; [2] 231-212-3; [3] 215-183-4 CAS Number: [1] 554-13-2; [2] 7447-41-8; [3] 1310-65-2 Index Number: - Contact details for dossier submitter: ANSES (on behalf of the French MSCA) 14 rue Pierre Marie Curie F-94701 Maisons-Alfort Cedex [email protected] Version number: 02 Date: June 2020 CLH REPORT FOR LITHIUM SALTS CONTENTS 1 IDENTITY OF THE SUBSTANCE........................................................................................................................1 1.1 NAME AND OTHER IDENTIFIERS OF THE SUBSTANCES .............................................................................................1 1.1.1 Lithium carbonate ........................................................................................................................................1 1.1.2 Lithium chloride ...........................................................................................................................................2 1.1.3 Lithium hydroxide.........................................................................................................................................3 1.2 COMPOSITION OF THE SUBSTANCE..........................................................................................................................3 -

Oleandrin-Mediated Inhibition of Human Tumor Cell Proliferation: Importance of Na,K-Atpase Α Subunits As Drug Targets
Published OnlineFirst August 11, 2009; DOI: 10.1158/1535-7163.MCT-08-1085 2319 Oleandrin-mediated inhibition of human tumor cell proliferation: Importance of Na,K-ATPase α subunits as drug targets Peiying Yang,1 David G. Menter,2 relatively higher expression of α3 with the limited expres- Carrie Cartwright,1 Diana Chan,1 Susan Dixon,1 sion of α1 may help predict which human tumors are likely Milind Suraokar,2 Gabriela Mendoza,2 to be responsive to treatment with potent lipid-soluble car- Norma Llansa,2 and Robert A. Newman1 diac glycosides such as oleandrin. [Mol Cancer Ther 2009;8(8):2319–28] Departments of 1Experimental Therapeutics and 2Thoracic/Head and Neck Medical Oncology and Clinical Cancer Prevention, The University of Texas, M. D. Anderson Cancer, Houston, Texas Introduction Cardiac glycosides are a class of compounds used to treat Abstract congestive heart failure by increasing myocardial contractile Cardiac glycosides such as oleandrin are known to inhibit force (1). Oleandrin is a cardiac glycoside derived from the Na,K-ATPase pump, resulting in a consequent increase Nerium oleander, which has been used for many years in in calcium influx in heart muscle. Here, we investigated Russia and China for this purpose. In contrast to its use the effect of oleandrin on the growth of human and mouse for the treatment of heart failure, preclinical and retrospec- cancer cells in relation to Na,K-ATPase subunits. Olean- tive patient data suggest that cardiac glycosides (e.g., digox- drin treatment resulted in selective inhibition of human in, digitoxin, ouabain, and oleandrin), may reduce the cancer cell growth but not rodent cell proliferation, which growth of various cancers including breast, lung, prostate, corresponded to the relative level of Na,K-ATPase α3 sub- and leukemia (2–7). -

Insights Into the Mechanisms of Action Ofthe MAO Inhibitors Phenelzine and Tranylcypromine
Insights into the Mechanisms of Action of the MAO Inhibitors Phenelzine and Tranylcypromine: A Review Glen B. Baker, Ph.D., Ronald T. Coutts, Ph.D., D.Sc., Kevin F. McKenna, M.D., and Rhonda L. Sherry-McKenna, B.Sc. Neurochemical Research Unit, Department of Psychiatry and Faculty of Pharmacy and Pharmaceutical Sciences, University of Alberta, Edmonton, Alberta Submitted: July 10, 1992 Accepted: October 7, 1992 Although the non-selective monoamine oxidase inhibitors phenelzine and tranylcypromine have been used for many years, much still remains to be understood about their mechanisms of action. Other factors, in addition to the inhibition of monoamine oxidase and the subsequent elevation of brain levels of the catecholamines and 5-hydroxytryptamine, may contribute to the overall pharma- cological profiles ofthese drugs. This review also considers the effects on brain levels of amino acids and trace amines, uptake and release of neurotransmitter amines at nerve terminals, receptors for amino acids and amines, and enzymes other than monoamine oxidase, including enzymes involved in metabolism of other drugs. The possible contributions of metabolism and stereochemistry to the actions of these monoamine oxidase inhibitors are discussed. Key Words: amino acids, monoamine oxidase, neurotransmitter amines, phenelzine, tranylcypromine, uptake Despite the fact that the non-selective monoamine oxidase nerve endings (Baker et al 1977; Raiteri et al 1977) and/or (MAO) inhibitors phenelzine (PLZ) and tranylcypromine may act as neuromodulators through direct actions on recep- (TCP) (see Fig. 1) have been used clinically for many years, tors for the catecholamines and/or 5-HT (Jones 1983; much remains to be learned about theirmechanisms ofaction. -
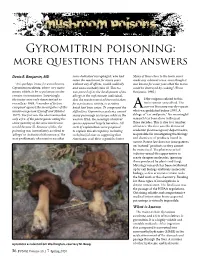
Gyromitrin Poisoning: More Questions Than Answers
Gyromitrin poisoning: more questions than answers Denis R. Benjamin, MD some dedicated mycophagist, who had Many of these clues to the toxin never eaten the mushroom for many years made any coherent sense, even though it “It is perhaps ironic for a mushroom, without any ill effects, would suddenly was known for some years that the toxins Gyromitra esculenta, whose very name and unaccountably take ill. This too could be destroyed by cooking.” (From means edible, to be so poisonous under was passed off as the development of an Benjamin, 1995.) certain circumstances. Surprisingly, allergy in the unfortunate individual, the toxins were only characterized as that the mushrooms had been mistaken ll the enigmas related to this recently as 1968. A number of factors for a poisonous variety, or a rotten toxin remain unresolved. The conspired against the investigators of this batch had been eaten. To compound the current literature merely repeats mushroom poison (Lincoff and Mitchel, difficulties, Gyromitra esculenta caused Awhat was published before 1990. A 1977). The first was the observation that many poisonings in Europe, while in the deluge of “cut and paste.” No meaningful only a few of the participants eating the western USA, the seemingly identical research has been done in the past same quantity of the same mushroom species appeared largely harmless. All three decades. This is due to a number would become ill. Because of this, the sorts of explanations were proposed of factors. The first was the demise of poisoning was immediately ascribed to to explain this discrepancy, including academic pharmacognosy departments, ‘allergy’ or ‘individual idiosyncrasy.’ The such fanciful ones as suggesting that responsible for investigating the biology next problematic observation was that Americans cook their vegetables better. -

Grayanotoxin Poisoning in Humans from Honey Consumption HELENA COLOMA DÍEZ AUTONOMOUS UNIVERSITY of BARCELONA
Grayanotoxin Poisoning in Humans from Honey Consumption HELENA COLOMA DÍEZ AUTONOMOUS UNIVERSITY OF BARCELONA Objectives Structure, Types and Isolation of GTX The main objective of this bibliographic research is compiling and announcing information Grayanotoxins are non-volatile diterpenes, a about grayanotoxin-containing honey and the toxic effects derived from its ingestion. This polyhidroxylated cyclic hydrocarbon with a 5/7/6/5 ring substance is believed to have medicinal properties, and the current increment of use of structure that does not contain nitrogen, as seen on figure 2. There are 25 known isoforms of grayanotoxins, natural products as dietetic complements with this finality may cause a rising in the number GTX-I and GTX-III being the most common and of intoxication cases. So it is important learning to recognise the clinical signs it causes and abundant ones, followed by GTX-II. their treatment, apart from finding out if it may have medicinal applications. TheGTXcanbeisolatedbytypicalextraction procedures for naturally occurring terpenes, such as paper electrophoresis, thin-layer chromatography (TLC), and gas chromatography (GC). They require derivatization before GC analysis due to the Introduction compound’s instability on heating and having low vapor pressure. Other identification techniques are based on The poisoning caused by grayanotoxin-containing honey, called “mad honey”, is known from infrared (IR), nuclear magnetic resonance (NMR), and antiquity. This toxic honey has been used for different purposes, such as biological weapon mass spectrometry (MS). or therapeutical product. Figure 2. Structure formulas (left pannel) and 3D The origin of this toxin relays in some plants of the Rhododendron genus, widespread all representations (right pannel) of GTX-I, II and III. -

083 Toxicity of Ibotenic Acid and Muscimol Containing Mushrooms Reported to a Regional Poison Control Center from 2002-2016 Mich
083 Toxicity of ibotenic acid and muscimol containing mushrooms reported to a regional poison control center from 2002-2016 Michael Moss 1,2 , Robert Hendrickson 1,2 1Oregon Health and Science University, Portland, OR, USA, 2Oregon Poison Center, Portland, OR, USA Background: Amanita muscaria (AM) and Amanita pantherina (AP) contain ibotenic acid and muscimol and may cause both excitatory and sedating symptoms. A "typical" syndrome of accidental ingestion with CNS depression in adults and CNS excitation in children and a paucity of GI symptoms or respiratory depression are based on relatively few reported cases with these mushrooms in North America. Research Question: What are the clinical effects of ibotenic acid/muscimol containing mushroom toxicity? Methods: Retrospective review of ingestions of ibotenic acid/muscimol containing mushrooms reported to a regional poison center from 2002-2016. Cases were included if identification was made by a mycologist or if AM was described as a red/orange mushroom with white spots. Results: Thirty-five cases met inclusion criteria. There were 24 cases of AM, 10 AP, and 1 A. aprica. Reason for ingestion included foraging (12), recreational (5), accidental (12), therapeutic (1), and self- harm (1). Of the accidental pediatric ingestions 4 (25%) were symptomatic. None of the children with a symptomatic ingestion of AM required admission. A 3-year old male who ingested AP developed vomiting, agitation, and lethargy. He was intubated and had a 3-day ICU stay. There were 25 symptomatic patients in total. All but one developed symptoms within 6 hours. Duration of symptoms was: <6 hours (6, 24%), 6-24 hours (15, 60%), >24 hours (1, 4%), and unreported (3, 12%).