An Examination of Light Intensity Physical Activity and Health in Older Adults Whitney A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Laser Beer (3Ncoeaaora to Lewero at Dletaoaj Sunsets They Saw the Symbol of God
, t M ftlf 11 $M j i tax .4 .4 - RiUblUhed Jul a. 1856. VOIj. XIX., 1STO. 3G51. XKXNOIOXTJ, HAWAIIAN ISLANDS, MOTS DAY. APRIL 2, 1894. PRICE: 5 CENTS. Business ari)s. cUdriis. of earth enough to leave a cha-- G000 Business THE PALACE OF THE SUN. feet deep and thirty miles in circum- ference; but such are the facts, and it is well worth the journey to see just C. BREWER CO., LIMITED M. E. D.D.S. HAWAIIAN HARDWARE CO., how a big mouutaiu looks after it has k Grossman, The New Jewelry Store belched forth so much valuable terri- 13 A 1 K , tory. HA W The Scene of Grandeur Beheld from Queen Street, Honolulu, H. S03 Street, The pilgrim fiually reaches the edge I Port Cutlery and Glassware its Summit. of Haleakala before daylight if he is ARE PREPARED TO MANUFACTURE ANY sensible! To his left is a cave beneath 307 AGENTS FOR THING IN Til KIR LINK. Fort strt. a pinnacle of raged rocks, and before 3575-l- v him the crater. The entire circum- Hawaiian Aerricnlfcnral Co.. Onomea I3JFD3STTISTY ference of the silent pit is surrounded Souvenir Spoons! bowlders and cathedral-shape- d 8ugar Co., Honomu 8ug&r Co , Wailuku J. U. DAVIDSON. BEAUTY, SILENCE AND DESOLATION. by mountain Rncar . Wit.ihfft Suerar Co.. Makee a specialty. Also, on band a fine stock cliffs, with here aud there a 8ugar Co., Haleakala Ranch Co., Kapa- - 93 HOTIL STRUT. of imported gap into which people can walk, and pala Kanch. from which they can look upon tho Line San Francisco Packets . -

Injustice Runs Deep Christopher Gordon Nicole Hayes the Goals of a Higher Education Usually Entail the Creation, Testing, and Implementation of New Ideas
Winner of Nine Collegiate Excellence in Journalism Awards fromo Our college. Our news. Our voice. Naugatuck Valley Community College November 1, 2016 Waterbury, Connecticut Vol. 60, Iss. 7 Embracing Ideas Injustice Runs Deep Christopher Gordon Nicole Hayes The goals of a higher education usually entail the creation, testing, and implementation of new ideas. In some colleges across America, Illinois, it could also affect those who rely on though, this concept is undergoing a radical the Mississippi River as a viable resource. shift. Students are being denied the ability to In direct violation of the National explore the wide world of free thought with Preservation Act of 1966, the Bakken Pipeline the execution of “safe spaces.” has already damaged burial sites belonging The creation of places of refuge comes to the Standing Rock Sioux. On September 3, from a position of caring. Sometimes, ideas construction workers began bulldozing along- are perceived as dangerous or dismissed as side the reservation, near historical burial sites. too ridiculous to be taken seriously. These As protesters attempted to peacefully block reactions may come in response to bigotry, the bulldozers, several people were bitten by sexism, and mockery. To give people a sanc- security dogs, and as many as thirty protes- tuary in which to develop an idea without tors were doused with pepper-spray. Several fear is laudable. However, a problem arises were arrested. A tribal chairman stated, “In when such refuges become havens of the one day, our sacred land has been turned into same sorts of bigotry, sexism, and mock- hollow ground.” Although the pipeline is not ery. -

Volume 65, Number 08 (August 1947) James Francis Cooke
Gardner-Webb University Digital Commons @ Gardner-Webb University The tudeE Magazine: 1883-1957 John R. Dover Memorial Library 8-1-1947 Volume 65, Number 08 (August 1947) James Francis Cooke Follow this and additional works at: https://digitalcommons.gardner-webb.edu/etude Part of the Composition Commons, Music Pedagogy Commons, and the Music Performance Commons Recommended Citation Cooke, James Francis. "Volume 65, Number 08 (August 1947)." , (1947). https://digitalcommons.gardner-webb.edu/etude/181 This Book is brought to you for free and open access by the John R. Dover Memorial Library at Digital Commons @ Gardner-Webb University. It has been accepted for inclusion in The tudeE Magazine: 1883-1957 by an authorized administrator of Digital Commons @ Gardner-Webb University. For more information, please contact [email protected]. XUQfr JNftr o 10 I s vation Army Band, has retired, after an AARON COPLAND’S Third Symphony unbroken record of sixty-four years’ serv- and Ernest Bloch’s Second Quartet have ice as Bandmaster in the Salvation Army. won the Award of the Music Critics Cir- cle of New York as the outstanding music American orchestral and chamber THE SALZBURG FESTI- BEGINNERS heard for the first time in New York VAL, which opened on PIANO during the past season. YOUNG July 31, witnessed an im- FOB portant break with tra- JOHN ALDEN CARPEN- dition when on August TER, widely known con- 6 the world premiere of KEYBOARD TOWN temporary American Gottfried von Einem’s composer, has been opera, “Danton’s Tod,” By Louise Robyn awarded the 1947 Gold was produced. -

Transgender Movement
New Trump Administration Memo on Obama Order Alarms LGBT Advocates Community Bonds Over Scoring Goals in the Detroit Drive Soccer League TRANS SINGER MOVED FELLOW MICHIGAN INMATES. NOW? AN ALBUM. WWW.PRIDESOURCE.COM AUGUST 23, 2018 | VOL. 2634 | FREE Join The Conversation @ Pridesource.com SAVE THE DATE PROFILE WAYNE’S WORLD A Local Designer’s Breathable, Butt- Hugging Underwear Line for Men Who Want to Feel COVER Comfortable While 16 Trans Singer Moved Fellow Michigan Inmates. Feeling Sexy Now? An Album. CONFERENCE NEWS Queering Racial Justice Heads to Detroit 6 Sue Carter Runs for WSU Board of Governors 6 Wade Rakes Runs for U of M Board of Regents See Page 22 See Page 14 7 Trump Administration Memo on Obama Order Alarms LGBT Advocates 12 Promoting Pride 12 Team-WERK HAPPENINGS NATIONAL NEWS ELECTION 2018 OPINION 8 Parting Glances 8 Viewpoint 9 Creep of the Week LIFE 14 Wayne’s World 18 Happenings 21 Puzzle and Crossword 20 The Frivolist: 7 Gay Tips for Throwing the Perfect Labor Day Party 26 Deep Inside Hollywood COMMUNITY CONNECTIONS 22 Detroit Repertory Theatre Hosts Second Arts & IN CONCERT JOE BIDEN VERMONT Culture Festival Sarah Shook & the Disarmers at OTUS Foundation Launches Campaign In First, Trans Candidate Wins Major Party 22 Affirmations Hosts Golden Girls Trivia Party Supply in Ferndale Promoting LGBTQ Acceptance Nomination for Governor’s Race 22 Queering Racial Justice Heads to Detroit See Page 18 24 Third Annual Strand with Trans Family Picnic See Page 11 See Page 10 Draws Record Crowd 22 Mom to Mom Sale in Ferndale on Aug. -

March 15, 2020
5376 State Street Saginaw, MI 48603 989-799-2460 www.stasaginaw.org March 15, 2020 Eucharistic Liturgies Saturday 4:00 PM Sunday 8:30 & 11:00 AM Tuesday - Thursday 8:30 AM First Friday 8:30 AM In the event of a funeral on Tuesday, Wednesday, Thursday or First Friday, morning Mass will be cancelled. Sacrament of Reconciliation 2nd & 4th Saturday 9:00-10:00 AM or by appointment Parish Staff Fr. Richard Bokinskie Pastor [email protected] Sr. Ann deGuise, OSF Pastoral Associate [email protected] Dawn Drago Parish Secretary [email protected] Pat Messing Bookkeeper [email protected] Deborah Kraklow Director of Liturgy and Music [email protected] Karen Bartels RCIA Director Baptism & Funeral Coordinator Welcome to our Parish: If you are a visitor to St. Thomas Aquinas, we want you to know how welcome you are. If you wish to become a member of our parish, please call the parish office. Parishioner Info: If you are moving, changing phone numbers or need to update family status, kindly notify the parish office. Rite of Christian Initiation of Adults (R.C.I.A.): Anyone seeking information about the Catholic Faith should contact the parish office for more information. Sessions meet from September through Spring. Baptisms: Held on the first weekend of the month after the required Baptism Preparation Class. Parents are required to be practicing Catholics and attending Mass regularly. Call the parish office to register. Marriage: Individuals must be registered in the parish at least six months before scheduling a wedding. A wedding date can only be set after meeting with the parish priest. -

December 2010 New
FOR YOUTH OF THE CHURCH OF JESUS CHRIST OF LATTER-DAY SAINTS THE DECEMBER 2010 COVER STORY: THE SEASON OF CARING, P. 2 SINGING PRAISE IN SOUTH AFRICA, P. 16 BOOK OF MORMON CHRISTMAS, P. 24 GIFTS TO SAMOA, P. 28 HOW MUCH IS ENOUGH? P. 34 In Tune: The First Presidency: Thomas S. Monson, Christmas Comes Again 8 Henry B. Eyring, Don Staheli and Jim Kasen Dieter F. Uchtdorf The Quorum of the Twelve Apostles: The Gift I Didn’t Want 10 Boyd K. Packer, L. Tom Perry, Chad Morris Russell M. Nelson, Dallin H. Oaks, M. Russell Ballard, I didn’t much like my Christmas present, but Richard G. Scott, Robert D. Hales, Jeffrey R. Holland, it eventually became precious to me. David A. Bednar, Quentin L. Cook, D. Todd Christofferson, Neil L. Andersen Line upon Line: Editor: Paul B. Pieper Luke 2:8–14 13 Advisers: Stanley G. Ellis, Christoffel Golden Jr., Yoshihiko Kikuchi Questions and Answers 14 “I have a hard time motivating myself to read Managing Director: David L. Frischknecht the scriptures. How can I find the motiva- Evaluation, Planning, and Editorial Director: tion?” Vincent A. Vaughn Graphics Director: THE SPIRIT WE FEEL AT Allan R. Loyborg CHRISTMASTIME p. 2 Sing Praise to Him 16 Managing Editor: Richard M. Romney Richard M. Romney South African youth worship the Lord Assistant Managing Editor: Janet Thomas The Message: through song. Associate Editors: David A. Edwards, The Spirit We Feel at Christmastime 2 Paul VanDenBerghe President Thomas S. Monson The Best Present 22 Publications Assistant: Sally J. Odekirk The Savior gave freely to all. -

Sound Connections Unity’S New Thought Music Resource
Sound Connections Unity’s New Thought Music Resource Issue #87 December 2012 Produced by Music Ministry Team and the Sacred Music Resources Department. Richard Mekdeci, Editor Sue Riley, Team Chair Blair Tabor, David Ezell, Carole Tomhave, Melinda Wood-Allen, Todd Lowry, Sheryl Meyers, Megon McDonough This Month’s Highlights─page 2 Another year of amazing service from your Music Ministry Team 2012 Sound Connections Music Conference at Unity Village─page 3 Announcing next year’s keynotes. Make plans now to attend. Feature Article─page 4 Christmas Carols and New Thought Theology: Have we finally found our “Sacred Cow?” From the Road – Traveling Artist Review─page 6 Kathy Zavada – Music and Ministry CD Review─page 7 Chants to Awaken by Kathy Zavada The Mailbox – Your Questions and Comments─page 8 Resources for your theater ministry / Music licensing in your church New Releases, Resources & Events─page 10 See what’s new and what’s coming up New Thought’s First Online Choral Library!─page 12 Find your holiday music here! Job Openings for Music Directors─page 13 New! Unity Church of Bay Area, League, TX.; Unity of Murfreesboro, Tenn.; Unity of Davis, Calif.; Unity Center for Creative Living, St. Johns, Fla. This Month’s Free Sheet Music Offering─page 14 “May You Know God” ─a beautiful, prayerful blessing song for the holiday New Thought’s First Music Director Listing: Online Only Currently over 180 music directors in 41 states and Canada. Help us make this a complete listing for all of New Thought. Update/add your name to this valuable resource. www.unity.org/music [email protected] 1 ThThhiis Month’s Highlights Greetings Sound Connections Family! Well, by the time you are reading this, you’ve probably already begun hearing those old familiar Christmas tunes playing on the radio. -

December 2003
Building a world class foster care system while serving our neighborhood youth DECEMBER 2003 Foster Care and Homeless Youth Speak out Across the Nation VOLUME III, ISSUE 11 VISIT US ONLINE AT WWW.MOCKINGBIRDSOCIETY.ORG Youth, Police Learn how to Talk Together Shay Deney My Day with the SPD Darius Reynolds FOR YEARS there has been a growing tension in Seattle between homeless youth and the Seattle Police Department (SPD). A lot of this tension is caused by pre-conceived notions and misconceptions, such as homeless youth thinking that all cops are out to get them and police thinking that every homeless kid does COPS AND ROBBERS; that’s supposed to drugs, steals, etc. Over the past couple years, the be the game, right? However, on the afternoon problems have been getting worse. The community Cop and youth on a smoke break. of Oct 15th in Seattle’s University District, a decided to take matters into their own hands and Photo by Darius Reynolds. time out was called in the game as police create something called the Donut Dialogues. This is Next up on the agenda was the actual dialogue. The officers and homeless youth set aside their where street youth and the SPD get together and talk room separated into five different groups: two officers differences to get a better understanding of about issues that each are having with the other. There and about six youth included in every group. The energy each other. have been four previous Donut Dialogues sessions held within the room felt calm, even light-hearted at times. -

Rock Album Discography Last Up-Date: September 27Th, 2021
Rock Album Discography Last up-date: September 27th, 2021 Rock Album Discography “Music was my first love, and it will be my last” was the first line of the virteous song “Music” on the album “Rebel”, which was produced by Alan Parson, sung by John Miles, and released I n 1976. From my point of view, there is no other citation, which more properly expresses the emotional impact of music to human beings. People come and go, but music remains forever, since acoustic waves are not bound to matter like monuments, paintings, or sculptures. In contrast, music as sound in general is transmitted by matter vibrations and can be reproduced independent of space and time. In this way, music is able to connect humans from the earliest high cultures to people of our present societies all over the world. Music is indeed a universal language and likely not restricted to our planetary society. The importance of music to the human society is also underlined by the Voyager mission: Both Voyager spacecrafts, which were launched at August 20th and September 05th, 1977, are bound for the stars, now, after their visits to the outer planets of our solar system (mission status: https://voyager.jpl.nasa.gov/mission/status/). They carry a gold- plated copper phonograph record, which comprises 90 minutes of music selected from all cultures next to sounds, spoken messages, and images from our planet Earth. There is rather little hope that any extraterrestrial form of life will ever come along the Voyager spacecrafts. But if this is yet going to happen they are likely able to understand the sound of music from these records at least. -
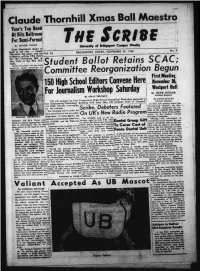
The Scribe by DDLCII PONON U Id V W D Ly « 1 a H W * C a M Fm T W E E U Y Look Maguiitt'a Choice As Band of the Year — Claude BRIDGEPORT
Year’s Tap Band M Rita Ballroom For Semi-Formal The Scribe By DDLCII PONON U id v w d ly « 1 a H W * C a m fm t W e e U y Look Maguiitt'a choice as band of the year — Claude BRIDGEPORT. CONN.. NOVEMBER 29. 1950 Thornhill, his piano and his Vol. 2 i orchestra, will be UB’s choice! for the Christmas Ball on Dec. 15th at the Hit* Ball room. Student Ballot Retains SCAC; Claude Thornhill, who has made piimprnus smash recordings lor Committee Reorganization Begun iSOffighSchool Editors Convene Here November S, Westport Hall For Journalism Workshop Saturday By RUTH ZUCKER > Political Reporter By o n n n r t e n n b n t By RUTH ZUCKER Political Reporter In their last meeting before the Thanksgiving vacation, the Stu Zl i K . “ c0'"'m \Scribe, Debaters Featured dent Council recognised the re sults of the recently held student referendum in favor of the contin | joint sponsorship o f the journalism O n UB's New Radio Program uation of the Student Council department Pi Delta Epsilon, the , .___________________ ________ _____ Advisory Committee. national undergraduate fraternity;! The SCRIBE took to thenur Officially, '-the referendum is Columbia and RCA. Victor will considered invalid because the nee- the SCRIBE; and the Wutori.n ¡“ ■¡ygJJ R ^ ^ .lL c i.te Dental Group Gift bring hi* musical aggregation with essary two-thirds vote of the stu yearbook. 1 . ■ ■—* him to demonstrate why he has •n vJi editor w w . __Dulcie__ | ______Ponon,. and business To Cover Cost off dent body, as stated in the Consti been picked as the band to watch Featured on the» program "J“wi'l.)l,|Bim ** Laaager ller Stahstah Josephson were In- tution, was not obtained. -

RECORD SHOP Gesamtkatalog Gültig Bis 31.12.2019 Record Shop Holger Schneider Flurstr
RECORD SHOP GESamtkatalOG gültig bis 31.12.2019 Record Shop Holger Schneider Flurstr. 7, 66989 Höheinöd, Germany Tel.: (0049) 06333-993214 Fax: (0049) 06333-993215 @Mail: [email protected] Homepage: www.recordshop-online.de Gruppe / Titel Artikelbeschreibung B.-Nr.Preis Gruppe / Titel Artikelbeschreibung B.-Nr. Preis 10 CC ROCK OR BUSTCD Lim. Edition im Digipack !!! EX/M 96501 6,99 € GREATEST HITS 1972 - 1978CD M-/M 90675 4,99 € ROCK OR BUSTCD Lim. Edition im Digipack !!! ORIGINALVERPACKT 93937 9,99 € STIFF UPPER LIPCD M/M 53656 6,99 € 12 STONES STIFF UPPER LIPCD Maxi EX-/M- 61532 4,99 € 12 STONESCD M-/M 97005 6,99 € STIFF UPPER LIP LIVEDVD 2001 M-/M 02085 9,99 € POTTERS FIELDCD M/M 97004 6,99 € THE RAZORS EDGECD D/1990/ACTO M/M 83231 6,99 € 18 SUMMERS AC/DC - BON SCOTT VIRGIN MARYCD EX-/M- 93108 6,99 € THE YEARS BEFORE AC/DCDVD M/M 01870 4,99 € 23RD GRADE OF EVIL AC/DC - VARIOUS ARTITS WHAT WILL REMAIN WHEN WE ARE GCD M-/M 98249 9,99 € BACK IN BLACKCD A TRIBUTE TO AC/DC M/M 85519 5,99 € 24 K THE MANY FACES OFCD 3 CD BOX Lim. Edition im Digipack !!! EX-/EX/EX/EX 96776 6,99 € BULLETPROOFCD EX-/M 82303 4,99 € ACCEPT PURECD EX-/M- 72083 4,99 € ACCEPTCD D/2005/Steamhammer M/M 99871 19,99 € 24-7 SPYZ ACCEPTLP Spain/79/Victoria Lady Lou.... M/M 20437 14,99 € 6CD EX/M 85408 2,99 € ALL AREAS - WORLDWIDECD-DO Doppel-CD M/M/M 59067 9,99 € 3 DOORS DOWN BEST OFCD M/M- 77627 4,99 € THE BETTER LIFECD M/M 84233 2,99 € BEST OFLP D/83/Braun EX/EX 20345 7,99 € 30.000 Kollegen BLOOD OF NATIONSCD Lim. -

HISTORY of the SABBATH and FIRST DAY of the WEEK by J
HISTORY OF THE SABBATH and FIRST DAY OF THE WEEK By J. N. Andrews PREFACE THE history of the Sabbath embraces the period of 6000 years. The seventh day is the Sabbath of the Lord. The acts which constituted it such were, first, the example of the Creator; secondly, his placing his blessing upon the day; and thirdly, the sanctification or divine appointment of the day to a holy use. The Sabbath, therefore, dates from the beginning of our world's history. The first who Sabbatized on the seventh day is God the Creator; and the first seventh day of time is the day which he thus honored. The highest of all possible honors does, therefore, pertain to the seventh day. Nor is this honor confined to the first seventh day of time; for so soon as God had rested upon that day, he appointed the seventh day to a holy use, that man might hallow it in memory of his Creator. This divine appointment grows out of the nature and fitness of things, and must have been made directly to Adam, for himself and wife were then the only beings who had the days of the week to use. As it was addressed to Adam while yet in his uprightness, it must have been given to him as the head of the human family. The fourth commandment bases all its authority upon this original mandate of the Creator, and must, therefore, be in substance what God commanded to Adam and Eve as the representatives of mankind. The patriarchs could not possibly have been ignorant of the facts and the obligation which the fourth commandment shows to have originated in the beginning, for Adam was present with them for a period equal to more than half the Christian dispensation.