Characterization of the Pathophysiological Determinants of Diarrheagenic Escherichia Coli Infection Using a Challenge Model in H
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Peptic Ulcer Disease
Peptic Ulcer Disease orking with you as a partner in health care, your gastroenterologist Wat GI Associates will determine the best diagnostic and treatment measures for your unique needs. Albert F. Chiemprabha, M.D. Pierce D. Dotherow, M.D. Reed B. Hogan, M.D. James H. Johnston, III, M.D. Ronald P. Kotfila, M.D. Billy W. Long, M.D. Paul B. Milner, M.D. Michelle A. Petro, M.D. Vonda Reeves-Darby, M.D. Matt Runnels, M.D. James Q. Sones, II, M.D. April Ulmer, M.D., Pediatric GI James A. Underwood, Jr., M.D. Chad Wigington, D.O. Mark E. Wilson, M.D. Cindy Haden Wright, M.D. Keith Brown, M.D., Pathologist Samuel Hensley, M.D., Pathologist Jackson Madison Vicksburg 1421 N. State Street, Ste 203 104 Highland Way 1815 Mission 66 Jackson, MS 39202 Madison, MS 39110 Vicksburg, MS 39180 Telephone 601/355-1234 • Fax 601/352-4882 • 800/880-1231 www.msgastrodocs.com ©2010 GI Associates & Endoscopy Center. All rights reserved. A discovery that Table of contents brought relief to millions of ulcer What Is Peptic Ulcer Disease............... 2 patients...... Three Major Types Of Peptic Ulcer Disease .. 6 The bacterium now implicated as a cause of some ulcers How Are Ulcers Treated................... 9 was not noticed in the stomach until 1981. Before that, it was thought that bacteria couldn’t survive in the stomach because Questions & Answers About Peptic Ulcers .. 11 of the presence of acid. Australian pathologists, Drs. Warren and Marshall found differently when they noticed bacteria Ulcers Can Be Stubborn................... 13 while microscopically inspecting biopsies from stomach tissue. -

Indeling Van Nederland in 40 COROP-Gebieden Gemeentelijke Indeling Van Nederland Op 1 Januari 2019
Indeling van Nederland in 40 COROP-gebieden Gemeentelijke indeling van Nederland op 1 januari 2019 Legenda COROP-grens Het Hogeland Schiermonnikoog Gemeentegrens Ameland Woonkern Terschelling Het Hogeland 02 Noardeast-Fryslân Loppersum Appingedam Delfzijl Dantumadiel 03 Achtkarspelen Vlieland Waadhoeke 04 Westerkwartier GRONINGEN Midden-Groningen Oldambt Tytsjerksteradiel Harlingen LEEUWARDEN Smallingerland Veendam Westerwolde Noordenveld Tynaarlo Pekela Texel Opsterland Súdwest-Fryslân 01 06 Assen Aa en Hunze Stadskanaal Ooststellingwerf 05 07 Heerenveen Den Helder Borger-Odoorn De Fryske Marren Weststellingwerf Midden-Drenthe Hollands Westerveld Kroon Schagen 08 18 Steenwijkerland EMMEN 09 Coevorden Hoogeveen Medemblik Enkhuizen Opmeer Noordoostpolder Langedijk Stede Broec Meppel Heerhugowaard Bergen Drechterland Urk De Wolden Hoorn Koggenland 19 Staphorst Heiloo ALKMAAR Zwartewaterland Hardenberg Castricum Beemster Kampen 10 Edam- Volendam Uitgeest 40 ZWOLLE Ommen Heemskerk Dalfsen Wormerland Purmerend Dronten Beverwijk Lelystad 22 Hattem ZAANSTAD Twenterand 20 Oostzaan Waterland Oldebroek Velsen Landsmeer Tubbergen Bloemendaal Elburg Heerde Dinkelland Raalte 21 HAARLEM AMSTERDAM Zandvoort ALMERE Hellendoorn Almelo Heemstede Zeewolde Wierden 23 Diemen Harderwijk Nunspeet Olst- Wijhe 11 Losser Epe Borne HAARLEMMERMEER Gooise Oldenzaal Weesp Hillegom Meren Rijssen-Holten Ouder- Amstel Huizen Ermelo Amstelveen Blaricum Noordwijk Deventer 12 Hengelo Lisse Aalsmeer 24 Eemnes Laren Putten 25 Uithoorn Wijdemeren Bunschoten Hof van Voorst Teylingen -

Active Peptic Ulcer Disease in Patients with Hepatitis C Virus-Related Cirrhosis: the Role of Helicobacter Pylori Infection and Portal Hypertensive Gastropathy
dore.qxd 7/19/2004 11:24 AM Page 521 View metadata, citation and similar papers at core.ac.uk ORIGINAL ARTICLE brought to you by CORE provided by Crossref Active peptic ulcer disease in patients with hepatitis C virus-related cirrhosis: The role of Helicobacter pylori infection and portal hypertensive gastropathy Maria Pina Dore MD PhD, Daniela Mura MD, Stefania Deledda MD, Emmanouil Maragkoudakis MD, Antonella Pironti MD, Giuseppe Realdi MD MP Dore, D Mura, S Deledda, E Maragkoudakis, Ulcère gastroduodénal évolutif chez les A Pironti, G Realdi. Active peptic ulcer disease in patients patients atteints de cirrhose liée au HCV : Le with hepatitis C virus-related cirrhosis: The role of Helicobacter pylori infection and portal hypertensive rôle de l’infection à Helicobacter pylori et de la gastropathy. Can J Gastroenterol 2004;18(8):521-524. gastropathie liée à l’hypertension portale BACKGROUND & AIM: The relationship between Helicobacter HISTORIQUE ET BUT : Le lien entre l’infection à Helicobacter pylori pylori infection and peptic ulcer disease in cirrhosis remains contro- et l’ulcère gastroduodénal dans la cirrhose reste controversé. Le but de la versial. The purpose of the present study was to investigate the role of présente étude est de vérifier le rôle de l’infection à H. pylori et de la gas- H pylori infection and portal hypertension gastropathy in the preva- tropathie liée à l’hypertension portale dans la prévalence de l’ulcère gas- lence of active peptic ulcer among dyspeptic patients with compen- troduodénal évolutif chez les patients dyspeptiques souffrant d’une sated hepatitis C virus (HCV)-related cirrhosis. -
Challenges in the Management of Acute Peptic Ulcer Bleeding
Review Challenges in the management of acute peptic ulcer bleeding James Y W Lau, Alan Barkun, Dai-ming Fan, Ernst J Kuipers, Yun-sheng Yang, Francis K L Chan Acute upper gastrointestinal bleeding is a common medical emergency worldwide, a major cause of which are bleeding Lancet 2013; 381: 2033–43 peptic ulcers. Endoscopic treatment and acid suppression with proton-pump inhibitors are cornerstones in the Institute of Digestive Diseases, management of the disease, and both treatments have been shown to reduce mortality. The role of emergency surgery The Chinese University of Hong continues to diminish. In specialised centres, radiological intervention is increasingly used in patients with severe and Kong, Hong Kong, China (Prof J Y W Lau MD, recurrent bleeding who do not respond to endoscopic treatment. Despite these advances, mortality from the disorder Prof F K L Chan MD); Division of has remained at around 10%. The disease often occurs in elderly patients with frequent comorbidities who use Gastroenterology, McGill antiplatelet agents, non-steroidal anti-infl ammatory drugs, and anticoagulants. The management of such patients, University and the McGill especially those at high cardiothrombotic risk who are on anticoagulants, is a challenge for clinicians. We summarise University Health Centre, Quebec, Canada the published scientifi c literature about the management of patients with bleeding peptic ulcers, identify directions for (Prof A Barkun MD); Institute of future clinical research, and suggest how mortality can be reduced. Digestive Diseases, Xijing Hospital, Fourth Military Introduction by how participants were sampled, their inclusion Medical University, Xian, China (Prof D Fan MD); Department of Acute upper gastrointestinal bleeding is characterised by criteria, and defi nitions of case ascertainment. -

An Overview: Current Clinical Guidelines for the Evaluation, Diagnosis, Treatment, and Management of Dyspepsia$
Osteopathic Family Physician (2013) 5, 79–85 An overview: Current clinical guidelines for the evaluation, diagnosis, treatment, and management of dyspepsia$ Peter Zajac, DO, FACOFP, Abigail Holbrook, OMS IV, Maria E. Super, OMS IV, Manuel Vogt, OMS IV From University of Pikeville-Kentucky College of Osteopathic Medicine (UP-KYCOM), Pikeville, KY. KEYWORDS: Dyspeptic symptoms are very common in the general population. Expert consensus has proposed to Dyspepsia; define dyspepsia as pain or discomfort centered in the upper abdomen. The more common causes of Functional dyspepsia dyspepsia include peptic ulcer disease, gastritis, and gastroesophageal reflux disease.4 At some point in (FD); life most individuals will experience some sort of transient epigastric pain. This paper will provide an Gastritis; overview of the current guidelines for the evaluation, diagnosis, treatment, and management of Gastroesophageal dyspepsia in a clinical setting. reflux disease (GERD); r 2013 Elsevier Ltd All rights reserved. Nonulcer dyspepsia (NUD); Osteopathic manipulative medicine (OMM); Peptic ulcer disease (PUD); Somatic dysfunction Dyspeptic symptoms are very common in the general common causes of dyspepsia include peptic ulcer disease population, affecting an estimated 20% of persons in the (PUD), gastritis, and gastroesophageal reflux disease United States.1 While a good number of these individuals (GERD).4 However, it is not unusual for a complete may never seek medical care, a significant proportion will investigation to fail to reveal significant organic findings, eventually proceed to see their family physician. Several and the patient is then considered to have “functional reports exist on the prevalence and impact of dyspepsia in the dyspepsia.”5,6 The term “functional” is usually applied to general population.2,3 However, the results of these studies disorders or syndromes where the body’s normal activities in are strongly influenced by criteria used to define dyspepsia. -

Systeembeschrijving Beheersgebied Oude Ijssel Juli 2016
Systeembeschrijving Beheersgebied Oude IJssel juli 2016 Systeembeschrijving beheersgebied Oude IJssel Inhoud Introductie in de systeembeschrijvingen ................................................................................................ 3 1 Samenvatting Beheersgebied Oude IJssel ....................................................................................... 4 2 Algemene informatie ....................................................................................................................... 9 2.1 Gebiedsbegrenzing en indeling ............................................................................................... 9 2.2 Bodem en ondergrond .......................................................................................................... 10 2.3 Historie .................................................................................................................................. 15 2.4 Landschap en landgebruik ..................................................................................................... 19 2.5 Natuur.................................................................................................................................... 21 3 Watersysteem ............................................................................................................................... 24 3.1 Algemeen: Beheersgebied Oude IJssel .................................................................................. 24 3.2 Oude IJssel en Aastrang ........................................................................................................ -

Leading Article Vaccines Against Gut Pathogens
Gut 1999;45:633–635 633 Gut: first published as 10.1136/gut.45.5.633 on 1 November 1999. Downloaded from Leading article Vaccines against gut pathogens Many infectious agents enter the body using the oral route development.15 Salmonella strains harbouring mutations and are able to establish infections in or through the gut. in genes of the shikimate pathway (aro genes) have For protection against most pathogens we rely on impaired ability to grow in mammalian tissues (they are immunity to prevent or limit infection. The expression of starved in vivo for the aromatic ring).6 Salmonella strains protective immunity in the gut is normally dependent both harbouring mutations in one or two aro genes (i.e., aroA, on local (mucosal) and systemic mechanisms. In order to aroC ) are eVective vaccines in several animal models after obtain full protection against some pathogens, particularly single dose oral administration and induce strong Th1 type non-invasive micro-organisms such as Vibrio cholerae, and mucosal responses.7 An aroC/aroD mutant of S typhi mucosal immunity may be particularly important. There is was well tolerated clinically in human volunteers; mild a need to take these factors into account when designing transient bacteraemia in a minority of the subjects was the vaccines targeting gut pathogens. Conventional parenteral only drawback.8 Th1 responses, cytotoxic T lymphocyte vaccines (injected vaccines) can induce a degree of responses, and IgG, IgA secreting gut derived lymphocytes systemic immunity but are generally poor stimulators of appeared in the majority of vaccinees.89 In an attempt to mucosal responses. -

Oude Ijssel R6 - Langzaam Stromend Riviertje Op Zand/Klei
Factsheet visstand en sportvisserij, bijlage bij het Visplan Rijn en IJssel Situatie per januari 2011 Oude IJssel R6 - Langzaam stromend riviertje op zand/klei Visrecht Verhuurder visrecht: Waterschap Rijn en IJssel Visrechthebbende: Federatie Midden Nederland (volledig) Schriftelijke toestemming: VISpas, landelijke lijst van viswateren Algemene beschrijving Ligging: De Oude IJssel loopt vanaf de Duitse grens naar Doesburg. Vanuit Duitsland en enkele zijwateren (zoals de Aa-strang) wordt water aangevoerd. Via een stuw met scheepvaartsluis bij Doesburg wordt het water afgevoerd naar de Geldersche IJssel. Totaal 3 stuwen, waarvan een met vispassage. Gelegen in de gemeenten Aalten, Bronckhorst, Doesburg, Doetinchem, Montferland, Oude IJsselstreek, Zevenaar Grootte: Lengte 36,8 km / Breedte: 35 meter Diepte: 2 tot 5 meter Watertype: Langzaam stromend gekanaliseerd riviertje Functie: Scheepvaart, waterafvoer, EVZ Oever: Steenstort Beheer: Er wordt niet gemaaid Baggeren bij Gendringen en Ulft (2013) Milieu: KRW-vismaatlat Waterplantenbedekking zomer Doorzicht: 0,8 m Huidige score: 0,418 (goed) Bovenwaterplanten: 2 % Baggerlaag: 10 cm Doel score: 0,4 (goed) Drijfbladplanten: 2 % Stroming: beperkt Ambitieniveau: laag Onderwaterplanten: 2 % Substraat: zand KRW-visstandbemonstering 2007 Totaal: 6 % Visbarriere: 2 stuwen Per hectare: Kg aantal Visstand: Blankvoorn-brasem viswatertype Meest Blankvoorn en voorkomend: baars Grootste Brasem, aal biomassa: Roofvis: Snoek en snoekbaars Vissterfte: Aalscholver- predatie Trend in visdichtheid (HVR) Factsheet -

Peptic Ulcer Disease
\ Lecture Two Peptic ulcer disease 432 Pathology Team Done By: Zaina Alsawah Reviewed By: Mohammed Adel GIT Block Color Index: female notes are in purple. Male notes are in Blue. Red is important. Orange is explanation. 432PathologyTeam LECTURE TWO: Peptic Ulcer Peptic Ulcer Disease Mind Map: Peptic Ulcer Disease Acute Chronic Pathophysiology Morphology Prognosis Locations Pathophysiology Imbalance Acute severe Extreme Gastric Duodenal gastritis stress hyperacidity between agrresive and defensive Musocal Due to factors increased Defenses Morphology acidity + H. Pylori infection Mucus Surface bicarbonate epithelium barrier P a g e | 1 432PathologyTeam LECTURE TWO: Peptic Ulcer Peptic Ulcer Definitions: Ulcer is breach in the mucosa of the alimentary tract extending through muscularis mucosa into submucosa or deeper. erosi on ulcer Chronic ulcers heal by Fibrosis. Erosion is a breach in the epithelium of the mucosa only. They heal by regeneration of mucosal epithelium unless erosion was very deep then it will heal by fibrosis. Types of Ulcer: 1- Acute Peptic Ulcers ( Stress ulcers ): Acutely developing gastric mucosal defects that may appear after severe stress. Pathophysiology: All new terms mentioned in the diagram are explained next page Pathophysiology of acute peptic ulcer Complication of a As a reult of Due to acute severe stress extreme gastritis response hyperacidity Mucosal e.g. Zollinger- inflammation as a Curling's ulcer Stress ulcer Cushing ulcer Ellison response to an syndrome irritant e.g. NSAID or alcohol P a g e | 2 432PathologyTeam -
Why Did the Netherlands Develop So Early? the Legacy of the Brethren of the Common Life
CPB Discussion Paper | 228 Why Did the Netherlands Develop so Early? The Legacy of the Brethren of the Common Life İ. Semih Akçomak Dinand Webbink Bas ter Weel Why Did the Netherlands Develop so Early? The Legacy of the Brethren of the Common Life* İ. Semih Akçomak Middle East Technical University [email protected] Dinand Webbink Erasmus University Rotterdam and CPB [email protected] Bas ter Weel CPB and Maastricht University [email protected] Abstract This research provides an explanation for high literacy, economic growth and societal developments in the Netherlands in the period before the Dutch Republic. We establish a link between the Brethren of the Common Life (BCL), a religious community founded by Geert Groote in the city of Deventer in the late fourteenth century, and the early development of the Netherlands. The BCL stimulated human capital accumulation by educating Dutch citizens without inducing animosity from the dominant Roman Catholic Church or other political rulers. Human capital had an impact on the structure of economic development in the period immediately after 1400. The educated workforce put pressure on the Habsburg monarchy leading to economic and religious resentment and eventually to the Revolt in 1572. The analyses show that the BCL contributed to the high rates of literacy in the Netherlands. In addition, there are positive effects of the BCL on book production and on city growth in the fifteenth and sixteenth century. Finally, we find that cities with BCL-roots were more likely to join the Dutch Revolt. These findings are supported by regressions that use distance to Deventer as an instrument for the presence of BCL. -

Ecologische Beoordeling Van Maatregelen Voor Beter Beleefbare Linies Te Doesburg
Ecologische beoordeling van maatregelen voor beter beleefbare Linies te Doesburg Eindconcept Culemborg, december 2013 Ecologische beoordeling van maatregelen voor beter beleefbare linies te Doesburg Rapport 201316 december 2013 Onderzoek en rapportage: G. Mostert M.Sc. Bureau LandLeven Parklaan 103 4102 EC Culemborg 0345-533300 [email protected] ECOLOGISCHE BEOORDELING VAN MAATREGELEN VOOR BETER BELEEFBARE LINIES TE DOESBURG Inhoud 1_ INLEIDING 3 2_ BELEID EN REGELGEVING 5 2.1 Algemeen _________________________________________________________ 5 2.2 Flora- en faunawet _________________________________________________ 5 2.3 Gelders Natuur Netwerk (GNN) _______________________________________ 8 2.4 Natuurbeschermingswet____________________________________________ 11 2.5 Boswet __________________________________________________________ 11 3_ RUIMTELIJKE INGREPEN OP DE HOGE LINIE 15 3.1 Overall-beschrijving _______________________________________________ 15 3.2 Verwijderen houtige begroeiing (struweel. opschot, bomen) met uitzondering van de eiken en de haag op één lunet____________________________________ 15 3.3 herprofileren taluds van vestingwerken, mede gericht op herstel en uitbreiding van de graslandvegetaties. _________________________________________ 18 3.4 paden op één lunet (eventueel verhoogd en geconditioneerd) 20 3.5 Aanbrengen afrasteringen langs toegankelijke deel van de Hoge Linie_____ 21 3.6 Beter zichtbaar maken Hoge Linie bij N317, b.v. door het realiseren van een “doorsnijding” langs de N317 _______________________________________ -
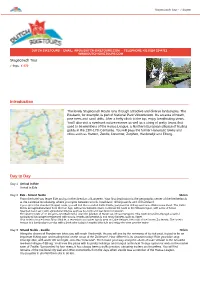
Introduction Day To
Stagecoach Tour - 7 dagen DUTCH BIKETOURS - EMAIL: [email protected] - TELEPHONE +31 (0)24 3244712 - WWW.DUTCH-BIKETOURS.COM Stagecoach Tour 7 days, € 570 Introduction The lovely Stagecoach Route runs through attractive and diverse landscapes. The Posbank, for example, is part of National Park Veluwezoom. It’s an area of heath, pine trees and sand drifts. After a hefty climb to the top, enjoy breathtaking views. You’ll also visit a riverbank nature reserve as well as a string of pretty towns that used to be members of the Hansa League, a Northern European alliance of trading guilds in the 13th-17th Centuries. You will pass the former Hanseatic towns and cities such as Hattem, Zwolle, Deventer, Zutphen, Harderwijk and Elburg. Day to Day Day 1 Arrival in Ede Arrival in Ede Day 2 Ede - Strand Nulde 56 km From the hotel you leave Ede and go in the direction of Lunteren. Your first destination is the geographic center of the Netherlands at the Lunterse Goudsberg, where you cycle between woods, heathland, drifting sands and old farmland. If you opt for the standard (longer) route, you will find the so-called Celtic Fields, just past the drifting sand area Wek eromse Zand. The Celtic Fields are agricultural land from the Iron Age, with a reconstructed farm. Continue the route to the Veluwe region, with a mix of forest, heathland and sand with agricultural villages such as Kootwijk and Garderen in between. The shorter route of 47 km goes over Barneveld, once the junction of Hanze and Hessen weggen. This route meanders through a varied agricultural landscape interspersed with woods, heaths and peatlands and many hamlets such as Appel.