Dystrophin Diagnosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Multiomic Approaches to Uncover the Complexities of Dystrophin-Associated Cardiomyopathy
International Journal of Molecular Sciences Review Multiomic Approaches to Uncover the Complexities of Dystrophin-Associated Cardiomyopathy Aoife Gowran 1,*, Maura Brioschi 2, Davide Rovina 1 , Mattia Chiesa 3,4 , Luca Piacentini 3,* , Sara Mallia 1, Cristina Banfi 2,* , Giulio Pompilio 1,5,6,* and Rosaria Santoro 1,4 1 Unit of Vascular Biology and Regenerative Medicine, Centro Cardiologico Monzino-IRCCS, 20138 Milan, Italy; [email protected] (D.R.); [email protected] (S.M.); [email protected] (R.S.) 2 Unit of Cardiovascular Proteomics, Centro Cardiologico Monzino-IRCCS, 20138 Milan, Italy; [email protected] 3 Bioinformatics and Artificial Intelligence Facility, Centro Cardiologico Monzino-IRCCS, 20138 Milan, Italy; [email protected] 4 Department of Electronics, Information and Biomedical Engineering, Politecnico di Milano, 20133 Milan, Italy 5 Department of Cardiac Surgery, Centro Cardiologico Monzino-IRCCS, 20138 Milan, Italy 6 Department of Biomedical, Surgical and Dental Sciences, University of Milan, 20122 Milan, Italy * Correspondence: [email protected] (A.G.); [email protected] (L.P.); cristina.banfi@cardiologicomonzino.it (C.B.); [email protected] (G.P.) Abstract: Despite major progress in treating skeletal muscle disease associated with dystrophinopathies, cardiomyopathy is emerging as a major cause of death in people carrying dystrophin gene mutations that remain without a targeted cure even with new treatment directions and advances in modelling Citation: Gowran, A.; Brioschi, M.; abilities. The reasons for the stunted progress in ameliorating dystrophin-associated cardiomyopathy Rovina, D.; Chiesa, M.; Piacentini, L.; (DAC) can be explained by the difficulties in detecting pathophysiological mechanisms which can also Mallia, S.; Banfi, C.; Pompilio, G.; Santoro, R. -

Molecular Genetic Analysis of the Adenomatous Polyposis Coli (APC)
Molecular Genetic Analysis of the Adenomatous Polyposis Coli(APC) gene region by Garret Malcolm Hampton A thesis submitted in requirement for the degree of Doctor of Philosophy at the University of London May, 1992 Cancer Genetics Laboratory (formerly Director's Laboratory) Imperial Cancer Research Fund London and Department of Genetics and Biometry University College London London University Page -1- ProQuest Number: 10609182 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a com plete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. uest ProQuest 10609182 Published by ProQuest LLC(2017). Copyright of the Dissertation is held by the Author. All rights reserved. This work is protected against unauthorized copying under Title 17, United States C ode Microform Edition © ProQuest LLC. ProQuest LLC. 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106- 1346 To my parents and my wife, Kate Page -2- Abstract Familial Adenomatous Polyposis (FAP) is a rare, autosomal dominant predisposition to colorectal cancer, affecting about one in ten thousand individuals in all populations studied. The gene responsible for this syndrome, designated APC (for Adenomatous Polyposis Coli) was mapped to 5q21-q22 by linkage analysis following a cytogenetic report of a male patient with polyposis and an interstitial deletion on 5q. The high incidence of allele loss at 5q21-q22 in carcinomas of sporadic patients suggests that mutation of the APC gene is a very frequent step in the tumorigenic pathway to nonfamilial colorectal carcinomas and emphasises the importance of isolating the gene and identifying its function. -

Gene Therapy Rescues Cardiac Dysfunction in Duchenne Muscular
JACC: BASIC TO TRANSLATIONAL SCIENCE VOL.4,NO.7,2019 ª 2019 THE AUTHORS. PUBLISHED BY ELSEVIER ON BEHALF OF THE AMERICAN COLLEGE OF CARDIOLOGY FOUNDATION. THIS IS AN OPEN ACCESS ARTICLE UNDER THE CC BY-NC-ND LICENSE (http://creativecommons.org/licenses/by-nc-nd/4.0/). PRECLINICAL RESEARCH Gene Therapy Rescues Cardiac DysfunctioninDuchenneMuscular Dystrophy Mice by Elevating Cardiomyocyte Deoxy-Adenosine Triphosphate a b c d,e Stephen C. Kolwicz, JR,PHD, John K. Hall, PHD, Farid Moussavi-Harami, MD, Xiolan Chen, PHD, d,e b,d,e e,f,g, b,e,g, Stephen D. Hauschka, PHD, Jeffrey S. Chamberlain, PHD, Michael Regnier, PHD, * Guy L. Odom, PHD * VISUAL ABSTRACT Kolwicz, S.C. Jr. et al. J Am Coll Cardiol Basic Trans Science. 2019;4(7):778–91. HIGHLIGHTS rAAV vectors increase cardiac-specific expression of RNR and elevate cardiomyocyte 2-dATP levels. Elevated myocardial RNR and subsequent increase in 2-dATP rescues the performance of failing myocardium, an effect that persists long term. ISSN 2452-302X https://doi.org/10.1016/j.jacbts.2019.06.006 JACC: BASIC TO TRANSLATIONAL SCIENCE VOL. 4, NO. 7, 2019 Kolwicz, Jr., et al. 779 NOVEMBER 2019:778– 91 Nucleotide-Based Cardiac Gene Therapy Restores Function in dmd Mice We show the ability to increase both cardiac baseline function and high workload contractile performance in ABBREVIATIONS aged (22- to 24-month old) mdx4cv mice, by high-level muscle-specific expression of either microdystrophin AND ACRONYMS or RNR. mDys = microdystrophin Five months post-treatment, mice systemically injected with rAAV6 vector carrying a striated muscle-specific CK8 regulatory cassette driving expression of microdystrophin in both skeletal and cardiac muscle, exhibited the = miniaturized murine creatine kinase regulatory greatest effect on systolic function. -
Impacts of Dystrophin and Utrophin Domains on Actin Structural Dynamics: Implications for Therapeutic Design
doi:10.1016/j.jmb.2012.04.005 J. Mol. Biol. (2012) 420,87–98 Contents lists available at www.sciencedirect.com Journal of Molecular Biology journal homepage: http://ees.elsevier.com.jmb Impacts of Dystrophin and Utrophin Domains on Actin Structural Dynamics: Implications for Therapeutic Design Ava Yun Lin, Ewa Prochniewicz, Davin M. Henderson, Bin Li, James M. Ervasti and David D. Thomas⁎ Department of Biochemistry, Molecular Biology, and Biophysics, University of Minnesota, 6-155 Jackson Hall, 321 Church Street SE, Minneapolis, MN 55455, USA Received 27 January 2012; We have used time-resolved phosphorescence anisotropy (TPA) of actin received in revised form to evaluate domains of dystrophin and utrophin, with implications for 26 March 2012; gene therapy in muscular dystrophy. Dystrophin and its homolog accepted 2 April 2012 utrophin bind to cytoskeletal actin to form mechanical linkages that Available online prevent muscular damage. Because these proteins are too large for most 11 April 2012 gene therapy vectors, much effort is currently devoted to smaller constructs. We previously used TPA to show that both dystrophin and Edited by R. Craig utrophin have a paradoxical effect on actin rotational dynamics— restricting amplitude while increasing rate, thus increasing resilience, Keywords: with utrophin more effective than dystrophin. Here, we have evaluated time-resolved individual domains of these proteins. We found that a “mini-dystrophin,” phosphorescence anisotropy; lacking one of the two actin-binding domains, is less effective than TPA; dystrophin in regulating actin dynamics, correlating with its moderate muscular dystrophy; effectiveness in rescuing the dystrophic phenotype in mice. In contrast, gene therapy we found that a “micro-utrophin,” with more extensive internal deletions, is as effective as full-length dystrophin in the regulation of actin dynamics. -

Diagnosis and Cell-Based Therapy for Duchenne Muscular Dystrophy in Humans, Mice, and Zebrafish
J Hum Genet (2006) 51:397–406 DOI 10.1007/s10038-006-0374-9 MINIREVIEW Louis M. Kunkel Æ Estanislao Bachrach Richard R. Bennett Æ Jeffrey Guyon Æ Leta Steffen Diagnosis and cell-based therapy for Duchenne muscular dystrophy in humans, mice, and zebrafish Received: 3 January 2006 / Accepted: 4 January 2006 / Published online: 1 April 2006 Ó The Japan Society of Human Genetics and Springer-Verlag 2006 Abstract The muscular dystrophies are a heterogeneous mutants carries a stop codon mutation in dystrophin, group of genetically caused muscle degenerative disor- and we have recently identified another carrying a ders. The Kunkel laboratory has had a longstanding mutation in titin. We are currently positionally cloning research program into the pathogenesis and treatment of the disease-causative mutation in the remaining 12 mu- these diseases. Starting with our identification of dys- tant strains. We hope that one of these new mutant trophin as the defective protein in Duchenne muscular strains of fish will have a mutation in a gene not previ- dystrophy (DMD), we have continued our work on ously implicated in human muscular dystrophy. This normal dystrophin function and how it is altered in gene would become a candidate gene to be analyzed in muscular dystrophy. Our work has led to the identifi- patients which do not carry a mutation in any of the cation of the defective genes in three forms of limb girdle known dystrophy-associated genes. By studying both muscular dystrophy (LGMD) and a better understand- disease pathology and investigating potential therapies, ing of how muscle degenerates in many of the different we hope to make a positive difference in the lives of dystrophies. -

Review Increasing Complexity of the Dystrophin-Associated Protein Complex Jonathon M
Proc. Nadl. Acad. Sci. USA Vol. 91, pp. 8307-8313, August 1994 Review Increasing complexity of the dystrophin-associated protein complex Jonathon M. Tinsley, Derek J. Blake, Richard A. Zuellig, and Kay E. Davies Molecular Genetics Group, Institute of Molecular Medicine, John Radcliffe Hospital, Headington, Oxford OX3 9DU, United Kingdom ABSTRACT Duchenne muscular dys- Purkinje neurons. Alternatively spliced dystrophin-1 (Dp7l) and apo-dystro- trophy is a severe X chromosome-linked, isoforms originating from the carboxyl- phin-3 are regulated by a promoter situ- muscle-wasting disease caused by lack of terminal coding region ofdystrophin have ated between exons 62 and 63 of the the protein dystrophin. The exact function also been described. The significance of dystrophin gene and are expressed in of dystrophin rem to be determined. these isoforms at the RNA and protein nonmuscle tissues, including brain, lung, However, analysis of its interaction with a level has not been elucidated. liver, and kidney. Apo-dystrophin-1 tran- large oligomeric protein complex at the Dystrophin is a 427-kDa protein local- scripts are only detectable in fetal and sarcolemma and the identicaton of a ized to the cytoplasmic face of the sar- newborn muscle. Muscle samples taken structurally related protein, utrophin, is colemma, enriched at myotendinous after 15 days postnatally have no apo- leading to the characterization ofcandidate junctions and the postsynaptic mem- dystrophin-1 transcript as determined by genes for other neuromusular disorders. brane of the neuromuscular junction reverse transcription-PCR. In rat brain, (NMJ). Dystrophin colocalizes with apo-dystrophin-1 transcripts continue in- Duchenne muscular dystrophy (DMD) is f3-spectrin and vinculin in three distinct creasing until they reach a maximum the most common muscular dystrophy, domains at the sarcolemma (overlaying after -1 mo. -

Disease-Proportional Proteasomal Degradation of Missense Dystrophins
Disease-proportional proteasomal degradation of missense dystrophins Dana M. Talsness, Joseph J. Belanto, and James M. Ervasti1 Department of Biochemistry, Molecular Biology, and Biophysics, University of Minnesota–Twin Cities, Minneapolis, MN 55455 Edited by Louis M. Kunkel, Children’s Hospital Boston, Harvard Medical School, Boston, MA, and approved September 1, 2015 (received for review May 5, 2015) The 427-kDa protein dystrophin is expressed in striated muscle insertions or deletions (indels) represent ∼7% of the total DMD/ where it physically links the interior of muscle fibers to the BMD population (13). When indel mutations cause a frameshift, they extracellular matrix. A range of mutations in the DMD gene encod- can specifically be targeted by current exon-skipping strategies (15). ing dystrophin lead to a severe muscular dystrophy known as Du- Patients with missense mutations account for only a small percentage chenne (DMD) or a typically milder form known as Becker (BMD). of dystrophinopathies (<1%) (13), yet they represent an orphaned Patients with nonsense mutations in dystrophin are specifically tar- subpopulation with an undetermined pathomechanism and no cur- geted by stop codon read-through drugs, whereas out-of-frame de- rent personalized therapies. letions and insertions are targeted by exon-skipping therapies. Both The first missense mutation reported to cause DMD was L54R treatment strategies are currently in clinical trials. Dystrophin mis- in ABD1 of an 8-y-old patient (16). Another group later reported sense mutations, however, cause a wide range of phenotypic se- L172H, a missense mutation in a structurally analogous location of verity in patients. The molecular and cellular consequences of such ABD1 (17), yet this patient presented with mild symptoms at 42 mutations are not well understood, and there are no therapies spe- years of age. -

Current Understanding of the Role of Cytoskeletal Cross-Linkers in the Onset and Development of Cardiomyopathies
International Journal of Molecular Sciences Review Current Understanding of the Role of Cytoskeletal Cross-Linkers in the Onset and Development of Cardiomyopathies Ilaria Pecorari 1, Luisa Mestroni 2 and Orfeo Sbaizero 1,* 1 Department of Engineering and Architecture, University of Trieste, 34127 Trieste, Italy; [email protected] 2 University of Colorado Cardiovascular Institute, University of Colorado Anschutz Medical Campus, Aurora, CO 80045, USA; [email protected] * Correspondence: [email protected]; Tel.: +39-040-5583770 Received: 15 July 2020; Accepted: 10 August 2020; Published: 15 August 2020 Abstract: Cardiomyopathies affect individuals worldwide, without regard to age, sex and ethnicity and are associated with significant morbidity and mortality. Inherited cardiomyopathies account for a relevant part of these conditions. Although progresses have been made over the years, early diagnosis and curative therapies are still challenging. Understanding the events occurring in normal and diseased cardiac cells is crucial, as they are important determinants of overall heart function. Besides chemical and molecular events, there are also structural and mechanical phenomena that require to be investigated. Cell structure and mechanics largely depend from the cytoskeleton, which is composed by filamentous proteins that can be cross-linked via accessory proteins. Alpha-actinin 2 (ACTN2), filamin C (FLNC) and dystrophin are three major actin cross-linkers that extensively contribute to the regulation of cell structure and mechanics. Hereby, we review the current understanding of the roles played by ACTN2, FLNC and dystrophin in the onset and progress of inherited cardiomyopathies. With our work, we aim to set the stage for new approaches to study the cardiomyopathies, which might reveal new therapeutic targets and broaden the panel of genes to be screened. -

1F800d5ff86e1b07fb02737a631e
ONCOLOGY LETTERS 12: 421-428, 2016 Investigating polymorphisms by bioinformatics is a potential cost‑effective method to screen for germline mutations in Chinese familial adenomatous polyposis patients JUN YANG1, WEI QING LIU2, WEN LIANG LI1, CHENG CHEN1, ZHU ZHU1, MIN HONG2, ZHI QIANG WANG1 and JIAN DONG2,3 Departments of 1Oncology and 2Internal Medicine‑Oncology, First Affiliated Hospital of Kunming Medical University, Kunming, Yunnan 650032; 3Department of Internal Medicine‑Oncology, Third Affiliated Hospital of Kunming Medical University, Kunming, Yunnan 650106, P.R. China Received January 22, 2015; Accepted April 12, 2016 DOI: 10.3892/ol.2016.4646 Abstract. The aim of this study was to investigate germline was observed in the AXIN2 gene. Comprehensive screening mutations of the APC, MUTYH and AXIN2 genes in Chinese for germline mutations in APC, MUTYH and AXIN2 genes patients with familial adenomatous polyposis (FAP), and further followed by prediction of pathogenicity using bioinformatic assess the value of bioinformatics in screening the pathogenic tools contributes to a cost-effective way of screening germline changes predisposing to FAP. APC genes from 11 unrelated FAP mutations in Chinese familial adenomatous polyposis patients. patients in Yunnan province in China were firstly examined by exon‑specific DNA sequencing. For samples without already Introduction known pathogenic changes predisposing to FAP in the APC gene, whole‑gene sequencing of MUTYH and AXIN2 was Familial adenomatous polyposis (FAP) is an autosomal performed. Mutational analysis of each gene was performed by dominantly inherited disease (1), which is characterized by bioinformatics. Eleven different types of APC polymorphisms the development of hundreds to thousands of adenomatous were observed in the cohort of families analyzed. -

Functional Correction of Dystrophin Actin Binding Domain Mutations by Genome Editing
Functional correction of dystrophin actin binding domain mutations by genome editing Viktoriia Kyrychenko, … , Rhonda Bassel-Duby, Eric N. Olson JCI Insight. 2017;2(18):e95918. https://doi.org/10.1172/jci.insight.95918. Research Article Muscle biology Dystrophin maintains the integrity of striated muscles by linking the actin cytoskeleton with the cell membrane. Duchenne muscular dystrophy (DMD) is caused by mutations in the dystrophin gene (DMD) that result in progressive, debilitating muscle weakness, cardiomyopathy, and a shortened lifespan. Mutations of dystrophin that disrupt the amino-terminal actin-binding domain 1 (ABD-1), encoded by exons 2–8, represent the second-most common cause of DMD. In the present study, we compared three different strategies for CRISPR/Cas9 genome editing to correct mutations in the ABD- 1 region of the DMD gene by deleting exons 3–9, 6–9, or 7–11 in human induced pluripotent stem cells (iPSCs) and by assessing the function of iPSC-derived cardiomyocytes. All three exon deletion strategies enabled the expression of truncated dystrophin protein and restoration of cardiomyocyte contractility and calcium transients to varying degrees. We show that deletion of exons 3–9 by genomic editing provides an especially effective means of correcting disease-causing ABD-1 mutations. These findings represent an important step toward eventual correction of common DMD mutations and provide a means of rapidly assessing the expression and function of internally truncated forms of dystrophin-lacking portions of ABD-1. Find the latest version: https://jci.me/95918/pdf RESEARCH ARTICLE Functional correction of dystrophin actin binding domain mutations by genome editing Viktoriia Kyrychenko,1,2,3 Sergii Kyrychenko,1,2,3 Malte Tiburcy,4,5 John M. -
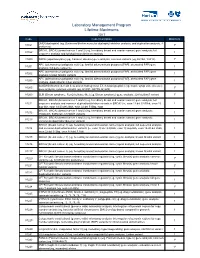
Laboratory Management Program Lifetime Maximums
Laboratory Management Program Lifetime Maximums 2017 Code Code Description Maximum DMD (dystrophin) (eg, Duchenne/Becker muscular dystrophy) deletion analysis, and duplication analysis, if 81161 1* performed BRCA1, BRCA2 (breast cancer 1 and 2) (eg, hereditary breast and ovarian cancer) gene analysis; full 81162 1 sequence analysis and full duplication/deletion analysis 81200 ASPA (aspartoacylase) (eg, Canavan disease) gene analysis, common variants (eg, E285A, Y231X) 1* APC (adenomatous polyposis coli) (eg, familial adenomatosis polyposis [FAP], attenuated FAP) gene 81201 1 analysis; full gene sequence APC (adenomatous polyposis coli) (eg, familial adenomatosis polyposis [FAP], attenuated FAP) gene 81202 1 analysis; known familial variants APC (adenomatous polyposis coli) (eg, familial adenomatosis polyposis [FAP], attenuated FAP) gene 81203 1 analysis; duplication/deletion variants BCKDHB (branched-chain keto acid dehydrogenase E1, beta polypeptide) (eg, maple syrup urine disease) 81205 1* gene analysis, common variants (eg, R183P, G278S, E422X) 81209 BLM (Bloom syndrome, RecQ helicase-like) (eg, Bloom syndrome) gene analysis, 2281del6ins7 variant 1* BRCA1, BRCA2 (breast cancer 1 and 2) (eg, hereditary breast and ovarian cancer) gene analysis; full 81211 sequence analysis and common duplication/deletion variants in BRCA1 (ie, exon 13 del 3.835kb, exon 13 1 dup 6kb, exon 14-20 del 26kb, exon 22 del 510bp, exon BRCA1, BRCA2 (breast cancer 1 and 2) (eg, hereditary breast and ovarian cancer) gene analysis; 81212 1 185delAG, 5385insC, 6174delT -

Elevation of Fast but Not Slow Troponin I in the Circulation of Patients With
Russell Alan (Orcid ID: 0000-0001-7545-5008) Elevation of fast but not slow troponin I in the circulation of patients with Becker and Duchenne muscular dystrophy Benjamin L Barthel PhD1, Dan Cox BSc2, Marissa Barbieri BA3, Michael Ziemba3, Volker Straub MD, PhD2, Eric P. Hoffman PhD3, Alan J Russell PhD1 1Edgewise Therapeutics, BioFrontiers Institute, University of Colorado, Boulder, CO 80303, USA. 2The John Walton Muscular Dystrophy Research Centre, Translational and Clinical Research Institute, Newcastle University and Newcastle Hospitals NHS Foundation Trust, Newcastle upon Tyne, NE1 3BZ, UK 3Department of Pharmaceutical Sciences, School of Pharmacy and Pharmaceutical Sciences, Binghamton University – State University of New York, Binghamton, NY 13902 USA Acknowledgements: Source of funding, private industry Number of words in abstract: 220 Number of words in manuscript: 2490 Corresponding author: Alan J Russell, 1Edgewise Therapeutics, BioFrontiers Institute, University of Colorado, Boulder, CO 80303, USA. [email protected]. ORCID ID https://orcid.org/0000-0001-7545-5008 Ethical publication statement: We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent This article has been accepted for publication and undergone full peer review but has not been through the copyediting, typesetting, pagination and proofreading process which may lead to differences between this version and the Version of Record. Please cite this article as doi: 10.1002/mus.27222 This article is protected by copyright. All rights reserved. with those guidelines. Key words: Muscular dystrophy, biomarker, muscle injury, creatine kinase, troponin Conflicts of interest: Benjamin Barthel and Alan Russell are paid employees of Edgewise Therapeutics, Inc.