District Health Action Plan Darbhanga 2009-2010
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Professor Anil Kumar Date of Birth: 20
Curriculum Vitae Name: Professor Anil Kumar Date of Birth: 20. 09. 1967. Designation: Professor and Head Department: Ancient Indian History Culture & Archaeology, Visva Bharati, Santiniketan, West Bengal, India. Pin 731235. Email: [email protected] , [email protected] ACADEMIC PROFILE Year Degree Board/College/University Division 1983 High School Bihar School Examination 1st. Board 1985 Intermediate Bihar Intermediate Council 1st. 1988 Graduation Allahabad University 2nd./ 1st class marks in Ancient History 1990 Masters Allahabad University 1st. Session Delayed and Result Published in 1992. 2000 Ph.D. Patna University Trade in Early Medieval Eastern India. 1991 NET/JRF ( UGC) University Grants Commission, Delhi. 1993 A Course on K.P.Jaiswal Research Research Institute, Patna. Methodology in History and Indology 2001 Appointed Lecturer in AIHC&A, at Visva Bharati, Santiniketan 2002 Refresher Course Centre for Research And Grade A Training in History, Archaeology And Palaeo- environment, New Delhi 2005 Orientation Course Patna University Grade A 2010 Refresher Course Ranchi University, Ranchi Grade A 2013 Refresher Course Allahabad University, Grade A Allahabad Area of Specialization: Early Medieval Arachaeology and Socio Economic History of Early Medieval India. Books; 1. Trade in Early Medieval Eastern India, Janaki Prakashan, Patna, Delhi, 2001. (Review published in Indian Historical Review, ICHR, New Delhi, Vol. XXXIV, No. I, pp. 301-305., The Quarterly Review of Historical Studies, Vol. XLIII, Nos. 3&4, Institute of Historical Studies Kolkata, and Journal of Dept. of History, Burdwan University, Vol.VI, No.I ) Second Edition of the Book Published in 2009. 2. Bihar Sthaniya Itihas Evam Parampara, ( Ed.) ( Hindi), Janaki Prakashan, Patna, Delhi, 1998. -

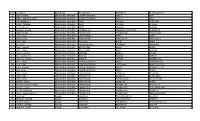
Detail of Existing Unit As on 28.02.2018 Industrial Area/Estate- Bela Region- Darbhanga SL
Detail of Existing Unit as on 28.02.2018 Industrial Area/Estate- Bela Region- Darbhanga SL. Date of Area in Present Name of Units Name Product Plot No. Remark No. allotment Sq.ft. Status 1 2 3 4 5 6 7 8 M/s Balaji Disposable & Packaging Pvt. Ltd. Part.- Sri Bharat Kumar Bagaria, Disposiable Glass Transfer in 1 1P 10890 Working - S/o- Pawan Kumar Bagaria, & Cup 08-07-2009 Gullowara, Darbhanga. Mob.- 9431219810 M/s Wood Crafts Bihar Prop.- Sri Late narendra Nath Jha, Saw Mill, S/o- Sri Girendra Mohan Jha, 2 Wooden, 25.04.84 3,4 10890 Working - Vill+PO- Bhawanipur, Ps.- Sakari, furniture Madhubani. Mob.- 9431086374 M/s Kishan Rice & Dal Mill, Prop.- Sri Bhola Sah, At- 3 ratnopatti, P.O.- Subhankarpur, Rice & Dal Mill 14.02.79 5,6 16988 Working - Distt.- Darbhanga. Mobile- 9835432755 M/s Sanjivani Ind. Prop.- Sri ram Babu, Ratnopatti, Transfer in 4 Rice & Dal mill , 9 6534 Working - PO.- subhankarpur, Darbhanga. 23-06-2009 Mob.- 9334360040 M/s Bimla Ice Factory Prop.- Smt. Vimla Devi W/o- Late Raghunath Thakur, At. Ice Slab & Ice 5 17.10.95 10 4356 Working - Nayatola, P.O.- Lalbagh, P.S.- Candy LNMU Darbhanga, Sunderpur, Bela, Darbhanga. M.ob- 8102505049 M/s Balajee Ice Candy Ind. Prop.- Sri Pramod Kumar, S/o- Ice Slab & Ice Transfer in 6 raghunath Thakur, Naya Tola, 11 4356 Working - Candy 13-07-11 sunderpur, Bela, Darbhanga. Mob.- 8102505049 M/s wood craft Mithila Prop.- Sri Narendra Mohan Jha, Vill+PO- Wooden 7 16.03.78 13, 34 25274 Working - Bhawanipur, Madhubani Furniture Mob.- 9461642569 M/s Maa Gayatri Ind Prop.- Sri Umesh Kumar yadav, S/o- Sri Puran Lal Yadav, Moh.- Edibal Oil & Oil 8 09.03.79 15 4356 Working - Balughat, Loharsari, Lalbagh, Naka Cack No.-02, Darbhanga Mob.- 9570861534 SL. -

State Dist GP Village CSP Name Contact Number Model Punjab FARIDKOT Dhiman Wali Dhiman Wali AMRITPAL SINGH 9915004096 PMJDY Punj
State Dist GP Village CSP Name Contact number Model Punjab FARIDKOT Dhiman wali Dhiman wali AMRITPAL SINGH 9915004096 PMJDY Punjab FARIDKOT Pakhi Kalan Pakhi Kalan Amandeep kaur 9803287500 PMJDY Punjab FATEHGARH SAHIB RAILON RAILON MOHANVEER SINGH 9781448504 PMJDY Punjab FAZILKA Mamu Joya Mamu Joya SARBJEET KAUR 7347511711 PMJDY Punjab MOGA Chotian Kalan Chotian Kalan Paramjeet kumari 9781610459 PMJDY Punjab KAPURTHALA Khagura Khagura AJIT SINGH M1 8968229045 PMJDY Punjab FAZILKA Moran Wala Moran Wala MAMTA RANI 9780974040 PMJDY Punjab FAZILKA Chak Jamalgarh Chak Jamalgarh PARVEEN KAUR 9465906424 PMJDY Punjab FEROZEPUR Chak Tahli Wala Chak Tahli Wala AMANDEEP SINGH 9988700440 PMJDY Punjab FEROZEPUR Chuhar Khilchi Chuhar Khilchi Hazoor Singh 9781138479 PMJDY Punjab FEROZEPUR Ferozepur City Ferozepur City Tersem Singh 9501930503 PMJDY Punjab FEROZEPUR Mehma Mehma GURDEEP SINGH 9781628193 PMJDY Punjab AMRITSAR Chak Aul Chak Aul KULDEEP SINGH 9888387466 PMJDY Punjab AMRITSAR Fathewal Fathewal RAMANPREET SINGH 9914110712 PMJDY Punjab GURDASPUR Babehali Babehali Gagandeep singh 9888860636 PMJDY Punjab GURDASPUR Jagowal Bet Jagowal Bet Raman Ohri 9814073389 PMJDY Punjab KAPURTHALA Chuharhwal Chuharhwal Sandeep Singh 9646864661 PMJDY Punjab LUDHIANA PABBIAN PABBIAN SONY KAUR 9888967594 PMJDY Punjab MOGA Chotta Ghar Chotta Ghar Gurjent Singh 9814913151 PMJDY Punjab TARN TARAN Asal Asal Gurwinder Singh 9501272812 PMJDY Punjab TARN TARAN Jaur singh Wala Jaur singh Wala Rajbir singh 9915674442 PMJDY Punjab TARN TARAN Deo Deo Ramandeep Singh 9779320303 -
Sr.No VLE Name Statename Districtname Blockname
Sr.No VLE Name StateName DistrictName BlockName PanchayatName 1 GEM TAYAM ARUNACHAL PRADESH LOWER SUBANSIRI ZIRO II JATH 2 RINKU PRASAD GUPTA ARUNACHAL PRADESH LOWER SUBANSIRI ZIRO II ZIRO 3 OSI WANGHA ARUNACHAL PRADESH TIRAP KHONSA BORDURIA 4 DAWA TSERING ARUNACHAL PRADESH TIRAP KHONSA KHONSA 5 Emlal Sharma ARUNACHAL PRADESH TIRAP KHONSA KHONSA 6 Chandan Prasad ARUNACHAL PRADESH CHANGLANG MANMAO-JAIRAMPUR JAIRAMPUR 7 SONU THAPA ARUNACHAL PRADESH CHANGLANG CHANGLANG CHANGLANG 8 Dena Dada ARUNACHAL PRADESH EAST KAMENG SEPPA SEPPA 9 Hillang Kapa ARUNACHAL PRADESH PAPUM PARE PAPU NALLA PAPU NALLA 10 Toku Take ARUNACHAL PRADESH Kra Daadi PALIN PANIA 11 Biri Asha ARUNACHAL PRADESH KURUNG KUMEY SANGRAM SANGRAM 12 Ranjit Jaiswal ARUNACHAL PRADESH WEST SIANG BASAR BASAR 13 Dobli Pakam ARUNACHAL PRADESH WEST SIANG AALO RAGLAM 14 Thutan Gombu ARUNACHAL PRADESH TAWANG LUMLA JANGDA 15 Arun Kumar Rai ARUNACHAL PRADESH NAMSAI NAMSAI DEOBEEL 16 Hemanto Phukan ARUNACHAL PRADESH NAMSAI LEKANG LEKANG (HQ) 17 Kime Tangu ARUNACHAL PRADESH LOWER SUBANSIRI ZIRO II PYAGANG LEYU 18 Gyati Kani ARUNACHAL PRADESH LOWER SUBANSIRI GYATI URU MUDO GYATI III 19 Vivek biswass ARUNACHAL PRADESH LOWER SUBANSIRI HAPOLI BAKHANG TULU 20 Padi Obing ARUNACHAL PRADESH LOWER SUBANSIRI ZIRO II YAZALI 21 Tana Simon ARUNACHAL PRADESH PAPUM PARE DOIMUKH DOIMUKH 22 KIME TARA ARUNACHAL PRADESH PAPUM PARE DOIMUKH RONO (NEW) 23 DANI TADO ARUNACHAL PRADESH PAPUM PARE NAHARLAGUN POLO COLONY 24 BISHNU SONAR ARUNACHAL PRADESH PAPUM PARE DOIMUKH MIDPU 25 Konchok Rinzin Khamba ARUNACHAL PRADESH UPPER SIANG PEKONG LALI PEKONG LALI 26 Shankar Thapa ARUNACHAL PRADESH CHANGLANG CHANGLANG OLD CHANGLANG 27 KECHA CHANGMI ARUNACHAL PRADESH CHANGLANG CHANGLANG PHANGTIP 28 Usham Bidhan Singha ARUNACHAL PRADESH CHANGLANG CHANGLANG NEW CHANGLANG 29 ELIAS ALI ASSAM DARRANG PUB MANGALDOI SHERPUR 30 EMAMUL HOQUE ASSAM DARRANG KALAIGAON (PT) PANBARI 31 Prakash Dubey ASSAM SONITPUR BAGHMARA KHORASIMOLU G.P. -
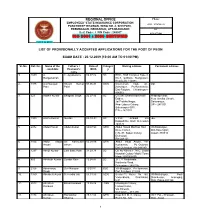
List of Provisionally Accepted Applications for the Post of Peon
REGIONAL OFFICE Phone: EMPLOYEES’ STATE INSURANCE CORPORATION 0135 – 2774762 / 63 PANCHDEEP BHAWAN, WING NO. 4, SHIVPURI, PREMNAGAR, DEHRADUN, UTTARAKHAND Fax Beat Code : I PIN Code : 248007 0135-2771542 ISO 9001 : 2000 CERTIFIED CHINTA SE MUKTI LIST OF PROVISIONALLY ACCEPTED APPLICATIONS FOR THE POST OF PEON EXAM DATE : 20.12.2009 (10:00 AM TO 01:00 PM) Sl. No. Ref. No. Name of the Father’s / Date of Categor Mailing address Permanent address candidate Husband’s Birth y name 1. 1859 A. C. Ayyaswamy 06.07.82 SC ESIC, Staff Complex Type-3, Ranganathan No-7, O-Block, Mangolpuri, New Delhi-110083 2. 1375 A.D.Narayan Shyam Kumar 01.06.83 GEN. C/o-Hetram Naik, AT- DO Patel Patel jhanakpur, Po-Baramkela, Dist-Raigarh, Chhattisgarh- 496551 3. 323 Aadhin Kumar Bhagwat Singh 20.07.86 SC C/o Shri Dharmendra Nath Pradeep Vihar, Dubey, Near Gavlira Chowk, Jai Prabha Nagar, Saharanpur, Near Labour Colony, UP – 247 001 Saharanpur (UP), PIN – 247 001 4. 1995 Aashu Kumar Gurdas 08-10-84 SC V.P.O. Ambadi Via -do- Dakpaththa Distt Dehradun 248125 5. 2072 Abdul Hamid Abdul shukur 08/07/90 GEN Abdul Hamid Marfhan Havi Vill-Barkanpur, Deve Camuli, Dist-Karemganj H.N.-97, Saken Colony, Assam-788810 Dehradun Pin-248121 6. 1104 Abdul Majid Sri Kalimullah 05.08.89 GEN Abdul Majid Ansari, Vill- Ansari Ansari Kurkawala, Po.-Doiwala, Dist-Dehradun, Pin-248140 7. 1297 Abhijit Kumar Late Babu Ram 31.03.78 SC Qtr.No-Reena F 7N.C, Jindal Hospital Colony Model Town Hisar-125005(H.R) 8. -
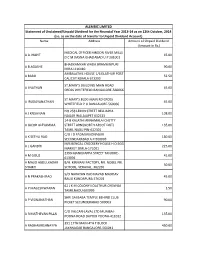
Name Address Amount of Unpaid Dividend
ALEMBIC LIMITED Statement of Unclaimed/Unpaid Dividend for the Financial Year 2013-14 as on 12th October, 2014 (i.e. as on the date of transfer to Unpaid Dividend Account) Name Address Amount of Unpaid Dividend (Amount in Rs.) MEDICAL OFFICER HINDON RIVER MILLS A A JHAPIT 45.00 D C M DASNA GHAZIABAD U P 201001 BHADKAMKAR WADA BRAMHINPURI A B AGASHE 90.00 MIRAJ 416410 AMBALATHIL HOUSE 1/6 ELATHUR POST A BABU 52.50 CALICUT KERALA 673303 ST.MARY'S BUILDING MAIN ROAD A I NATHAN 45.00 CROSS WHITEFIELD BANGALORE-560066 ST MARY'S BLDG MAIN RD CROSS A IRUDAYANATHAN 45.00 WHITEFIELD P O BANGALORE-560066 NO 258 LEMIN STREET BELLIAPPA A J KRISHNAN 108.00 NAGAR WALAJAPET 632513 14-B KALATHI ANNAMALAI CHETTY A JACOB ALEYAMMA STREET ARNI(NORTH ARCOT DIST) 135.00 TAMIL NADU PIN-632301 C/O I D PADMARAONAGAR A K SETHU RAO 180.00 SECUNDARABAD A P-500003 M/S BENGAL CROCKERY HOUSE H O EGG A L GANDHI 225.00 MARKET SIMLA-171001 2399 MANOJIAPPA STREET TANJORE- A M GOUZ 45.00 613001 A MAJID ABDULKADAR B/H. KIRMANI FACTORY, NR. NOBEL PRI. 30.00 SHAIKH SCHOOL, VERAVAL. 362265 S/O NARAYAN RAO NAVAD MADHAV A N PRAKASH RAO 45.00 BAUG KUNDAPURA 576201 62 J K M COLONY KOLATHUR CHENNAI A P MAGESHWARAN 1.50 TAMILNADU 600099 SHRI SAI BABA TEMPLE BEHIND CLUB A P VISWANATHAN 90.00 PICKET SECUNDERABAD 500003 C/O VALCAN-LAVAL LTD MUMBAI- A R MATHEVAN PILLAI 135.00 POONA ROAD DAPODI POONA-411012 391 17TH MAIN 4TH T BLOCK A RADHAKRISHNAYYA 450.00 JAYANAGAR BANGALORE-560041 ALEMBIC LIMITED Statement of Unclaimed/Unpaid Dividend for the Financial Year 2013-14 as on 12th October, 2014 (i.e. -
![Iz[ Kam F'k{Kd Fu;Kstu Bdkbz] Rkjmhga](https://docslib.b-cdn.net/cover/3810/iz-kam-fk-kd-fu-kstu-bdkbz-rkjmhga-3643810.webp)
Iz[ Kam F'k{Kd Fu;Kstu Bdkbz] Rkjmhga
iz[kaM f'k{kd fu;kstu bdkbZ] rkjMhgA PROVISIONAL MERIT LIST - ---------------- BLOCK - TARDIH SUBJECT- MATH (TRAINED) DISTRICT- DARBHANGA NAME OF PASSING YEAR CATEGORY REMARKS GENDER MATRIC INTER GRADUATION TRAINED T.E.T SIN0. R.NO APPLICANT NAME FATHER'S NAME D.O.B. ADDRESS TRAINING SESSION MERIT F.M. M.O. PER F.M. M.O PER F.M M.O PER F.M. M.O PER ROL.NO. F.M M.O PERCEN WEIGHTA COLLEGE GE 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 KANHAIYA JI JHA DEOKI RAMAN JHA AT-GANGAULI KANKPUR,PO- D.D.E. 2018 1 1 10.01.1981 EWS M GANGAULI,PS-SAKATPUR,DBG 700 341 48.71 900 472 52.44 1500 751 50.07 1300 852 65.53 6102175538 144 87 60.42 2 56.19 NARESH KUMAR THAKUR MAHENDRA THAKUR AT+PO-RAGHOPUR,PS- D.D.E.(LNMU)DBG 0 2017 2 2 12.06.1986 EBC M 700 433 61.86 900 451 50.11 1500 806 53.73 1300 892 68.62 6104175449 146 98 67.12 2 60.58 MANIGACHHI,DBG AVINASH KUMAR VIDIYA NAND VIMAL AT-BHARI,PO-BATHNAHA,PS- KIRAN 0 2019 3 3 12.01.1995 BC M 500 353 70.60 500 368 73.60 1500 883 58.87 1300 959 73.77 0202016754 150 92 61.33 2 71.21 PHULPRAS,MADHUBANI T.T.C.PANDAUL BALRAM SHRMA RAM SUNDAR SHRMA AT+PO-RAJAKHARWAR,PS- KSHATRIYA,COLLEG 0 2018 4 4 09.03.1989 EBC M 700 475 67.86 900 513 57.00 1500 911 60.73 1400 912 65.14 0202013336 150 84 56.00 2 64.68 SAKATPUR,DBG E OF EDUCATION SAMARJIT KUMAR RAJENDRA PRASAD AT+PO-KABIRCHAK,PS- D.C.E.SHISHO DBG 0 2015 5 5 05.02.1987 BC M 700 517 73.86 900 483 53.67 1500 884 58.93 1000 851 85.10 6107175150 146 94 64.38 2 69.89 YADAV SADAR,DBG CHANDAN KUMAR VIDIYA NAND SINGH AT+PO-POKHARBHINDA,PS- -

Directorate of Distance Education L.N
DIRECTORATE OF DISTANCE EDUCATION L.N. Mithila University, Kameshwaranagar, Darbhanga-846008 (BIHAR) Phone & Fax : 06272-246506 Website : ddelnmu.ac.in, E-mail : [email protected] S.N. Class Name of Father's Name Mother's Name Gender Category D.O.B. Aadhar Mobile No. Email Address Address Roll No. Student 1 19001 Avinash Prahlad Sahni Hira Devi M EBC 03.03.1996 277512757960 9534867511 [email protected] Vill- Brahmotra, PO- Ratanpura, PS- Ashok Kumar om Paper Mill, Darbhanga 846002 2 19002 Chandan Shila Kant Jha Mamta Devi M GEN 10.03.1996 761477060724 7488212064 [email protected] Vill+PO- Kathra, PS- Manigachhi, Kumar Jha Darbhanga 847423 3 19003 Nisha Bharti Shrish Kumar Neena F GEN 02.02.1997 818674129646 9709904490 [email protected] Laxmipur, Ward No.-2, PO- Basudeopur, PS- Lal Das Priyadarshi LNMU Campus, Darbhanga 846005 4 19004 Ankit Kumar Rishi Alok Reena Singh M GEN 24.09.1995 490089418382 7654753737 [email protected] New Market, Commercial Chowk, Laheriasarai, Darbhanga 846001 5 19005 Madan Kumar Raj Kumar Rampari Devi M BC 03.02.1996 697577136924 8676993976 madankumarmk3976@gmail. At-Ghuski Patti, PO- Gehumabairiya, PS- Mahto com Phulparas, Madhubani 847402 6 19006 Manu Rani Arbendra Anamika Kumari F GEN 15.01.1994 921359951759 9472355552 [email protected] Saraswati Bihar, Bank Colony, Laxmisagar, Kumar Jha Darbhanga 846009 7 19007 Arfa Mohsin Md. Mohsin Bibi Noor Jahan F EBC 01.01.1996 452402969067 7903292627 [email protected] Abdullah Ganj, Laheriasarai, Darbhanga 846001 8 19008 Raju Kumar Shreeprasad Rampari Devi M SC 01.12.1994 350163963614 9006478261 [email protected] At & PO- Mansapur, PS- Laukahi, Ram Ram Madhubani 847108 9 19009 Kumari Shikha Amrendra Indra Mishra M GEN 15.01.1996 990546626952 8240162719 [email protected] Teacher's Colony, Azamnagar, Darbhanga Kumar Mishra 846004 10 19010 Prawin Kumar Ram Ratan Shanti Devi M EBC 25.07.1997 342103191061 8340762178 prawinkumarmandal3@gmail. -

DISTRICT : Munger
District District District District District Sl. No. Name of Husband's/Father,s AddressDate of Catego Full Marks Percent Choice-1 Choice-2 Choice-3 Choice-4 Choice-5 Candidate Name Birth ry Marks Obtained age (With Rank) (With Rank) (With Rank) (With Rank) (With Rank) DISTRICT : Munger 1BABITA SHRI- SICHANAND vill- karhariya 10-May-69 BC 900 857 95.22 Bhagalpur (1) Banka (1) Munger (1) Jamui (1) Purnia (1) SINGH thana- bath dist- bhagalpur 2 KUMARI PUNAM SRI BALESHWAR c/o- sri baleshwar 01-Jan-85 BC 700 631 90.14 Banka (2) Bhagalpur (2) Munger (2) Khagaria (1) Katihar (1) BHARTIA MANDAL mandal vill - babudih post -bhurna via- bausi, banka. bihar pin code - 813119 3 RENU KUMARIASHOK KUMAR vill-maharna (talab par) 04-May-69 BC 700 617 88.14 Munger (3) Lakhisarai (1) Bhagalpur (3) Jamui (2) Sheikhpura (1) po-dharara dis-mungar 4 KUMARI SARITA AJYA KUMAR vill-pahra 10-Aug-68 BC 700 609 87 Arwal (2) Jahanabad (2) Munger (4) Patna (1) Aurangabad (1) GUPTH GUPTA po-akbarpur dis-arwal pin-804401 5 KABITA KUMARILET NIVIN PRASAD villi+po-khria 31-Dec-69 GEN 700 609 87 Munger (5) Banka (3) Bhagalpur (4) Lakhisarai (2) SINGH ps-habali kharakpur dis-munger 6SARITA KUMARISRI ARVIND RAM c/o- sri arvind ram das 05-Feb-86 BC 700 607 86.71 Banka (4) Bhagalpur (5) Munger (6) Khagaria (2) Katihar (2) DAS vill- babudih post- bhurna via- basi, banka, bihar- 813119 7 CHANDRAKALA SRI RAMAKANT mohalla- gandhi 04-May-73 MBC 700 600 85.71 Khagaria (3) Begusarai (1) Saharsa (1) Bhagalpur (6) Munger (7) DEVI PODDAR nagar,ward no-3, distt- khagaria 8 SUSHILA DEVI -

Name Address Amount of Unpaid Dividend
ALEMBIC LIMITED Statement of Unpaid / Unclaimed Dividend for the year 2017-18 as on 6th September, 2018 (i.e. as on the date of transfer to Unpaid Dividend Account Name Address Amount of Unpaid Dividend (in Rs.) SANJAY SHIVSHANKAR MATTE QTR NO 101 SHASTRI NAGAR, GHUGUS, CHANDRAPUR, 40.00 CHANDRAPUR, 0 MUKESH SHUKLA LIC CBO-3 KA SAMNE, DR. MAJAM GALI, BHAGAT COLONEY, 8.00 JABALPUR, 0 HAMEED A P . ALUMPARAMBIL HOUSE, P O KURANHIYOOR, VIA CHAVAKKAD, 36.00 TRICHUR, 0 KACHWALA ABBASALI HAJIMULLA MOHMMADALI PLOT NO. 8 CHAROTAR CO OP SOC, GROUP B, OLD PADRA RD, 72.00 VADODARA, 0 KERIATBHAI RAMBHAI PATEL VASAD NEAR APPROCH ROAD, P O VASAD TA ANAND, DIST KAIRA 60.00 PIN-391830, , 0 JITENDRABHAI RANCHHODBHAI PATEL GREEN BUNGLOW RLY CROSSING, P O VASAD TA ANAND, DT 60.00 KAIRA PIN-391830, , 0 MANOHAR LAL CHAUHAN STATION ROAD PO GHATSILA, DT EAST SINGBHUM, JHARKHAND, , 180.00 0 PURSHOTTAM CHHOTABHAI PATEL JAY HIND KHADKI, VASAD, DIST KAIRA (GUJARAT) PIN-391830, , 0 120.00 AMBALAL TRIBHOVANBHAI PATEL VASAD NEAR RAMJI MANDIR, P O VASAD TA ANAND, DIST KAIRA 60.00 PIN-391830, , 0 RAMESHBHAI RANCHHODBHAI PATEL GREEN BUNGLOW RLY CROSSING, POST VASAD TAL ANAND, DIST 30.00 KAIRA 391830, , 0 SHURESHBHAI RAMBHAI PATEL NEAR APPROCH ROAD, PO VASAD TA ANAND, DIST KAIRA PIN- 60.00 391830, , 0 VIJAYKUMAR VIRAPPA NAKATE SANGAMNAGAR, TALUKA-SATARA PIN-422065, , , 0 120.00 CHIMANBHAI RAIJIBHAI KACHHIA PATEL NEAR PARABDI VASAD, TA ANAND, DIST KAIRA PIN-391830, , 0 30.00 VIJAYKUMAR VIRAPPA NAKATE SANGAMNAGAR, TALUKA-SATARA PIN-422065, , , 0 420.00 ATUL AMBAVIDAS DOSHI SECTOR 6/C/1/202 NEELKAMAL, SHANTI NAGAR SOCIETY, 72.00 MIRAROAD EAST, THANE, 0 NATUBHAI MAGANBHAI PATEL VASAD SHAKKAR FALIYA, P O VASAD TA ANAND, DIST KAIRA PIN- 60.00 391830, , 0 GAJANAND JANGIR GAJANAND S\O KISTOOR CHAND, JANGIR VILLAGE- MITHARI, TEH. -

Village & Townwise Primary Census Abstract, Series-4, Bihar
CEN-SUS OF lNDIA PARTS XIU-A_ & B 198f VILLAGE. & TOWN DIRECTORY SERIES 4-SIHAR VILLAGE & TOWNWISE PRIMARY' CENSUS ABSTRACT DISTRICT CENSUS DAR·BHANGA HANDBOOK DISTRICT B. B. LAL . OF THE INDIAN ADMINISTRATIVE SERVICE Director of Census Operations, Bihar 1981 CENSUS PUBLICATIONS OF BIHAR (All the Census Publications of this State will bear series 4) Part I-A Administration Report-Enumeration \ Offi ;rl use only. Part f-B Administration Report-Tabulation 1 C.ii Part II-A General Population Tab,les {A-series-, Tables A-l to 4--P) ..Part IJ-B Primary Census Abstrac~ : ., , ," Part III-A General Economic Tables (B-series Tables B-1 to B-I0) Part fII-B General Economic Tables, (D-series Tables B-ll to B-22) Part IV-A Social and Cultura;t Tables (C-series Tables C-l to C-6) Part IV-B Social and Cultural Tables (C-series Tables C-7 to C-9) !tart IV-e •• ~ Household by composition and size (C-Series Table C-IO) Part V-A Migration Tables (D-series Tables D-l to D-4) Part V-B Migration Tables (D-series Tables D-5 to D-13) Part VI-A }tertility Tables (F-series Tables F-l to F-19) Part VI-B F'ertility Tables (F-series Tables F-20 to F-28) Part vn 'rabIes on Houses and Disabled Population (H-series Tables H-l and H-2) Part VIII-A Household Tables (HH-series Tables HH-l to HH-16) Part Vln-B Household Tables (HH-series Table HH-17) ''Part IX Special Tables on Scheduled Castes andt:S~£_q~~ Trjb~ (SC 'and ST-series Tables) Part X-A Town Directory Part X-B Survey Reports on selected towns Part X-C Survey Reports on selected villages Part XI Ethnographic notes and special studies on Scheduled Castes and Scheduled Tribes Part XII Census Atlas Part XITI-A District Census Handbook-Village and Town Directory Part XIII-B District Census Handbook-General Population Tables (C. -

28Th January 2011 Union Bank of India Alternat
Request For Proposal For Selection of Enrollment Agency for Aadhaar Project Date: 28th January 2011 Union Bank of India Alternate Channels and New Initiative Dept. 12th Floor, Union Bank Bhavan, 239, Vidhan Bhawan Marg, Nariman Point, Mumbai - 400092 1 Contents INVITATION FOR PROPOSAL ......................................................................................................................... 4 INTRODUCTION ............................................................................................................................................. 6 INSTRUCTION TO BIDDERS - STANDARD ....................................................................................................... 7 INSTRUCTION TO BIDDERS – DATA SHEET .................................................................................................. 16 SCOPE OF WORK ......................................................................................................................................... 22 Functional scope ..................................................................................................................................... 22 Procure Biometric Devices as per UIDAI Specifications ...................................................................... 22 Setting up of Enrolment Stations and Enrolment Centers .................................................................. 22 Hire & Train Manpower for Enrolment ................................................................................................... 25 Hiring Manpower: