Randomized Clinical Trial of Torsional Versus Linear Mode Ultrasonically Activated Devices for Laparoscopic Cholecystectomy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
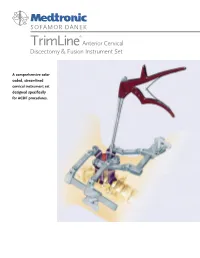
TRIMLINE® ACDF INSTRUMENT SET Cat
SOFAMOR DANEK ® TrimLine Anterior Cervical Discectomy & Fusion Instrument Set A comprehensive color coded, streamlined cervical instrument set designed specifically for ACDF procedures. Anterior Cervical Discectomy and Graft Curettes Fusion Instrument Set Placement Instruments Color coded handles to differentiate sizes The TrimLine ACDF Instrument Set has been designed Can be used with autograft or allograft Hand polished cutting specifically for standard cervical anterior approaches, Holder/Introducer will not leave a hole in surfaces to help discectomies, and fusions. It includes instruments necessary the graft maintain sharp edges to perform the cervical exposure, decompression, graft harvest, Ergonomically designed handles Fully machined and placement. Instruments are color coded to simplify components to enhance identification and this feature allows the procedure to product run more smoothly. Instruments can be purchased consistency separately or as part of the TrimLine Set. Kerrisons Color coded handles to differentiate sizes Hand polished cutting surfaces to help maintain sharp edges Fully machined components to enhance product consistency Pin Distraction Set Universally acceptable Self-Retaining instruments Retractors Improved pin strength Right and left options Generic blade for use with either fixed or rotating Hand-Held modular blade handles Retractors Modular blade handles can be removed after retractor frame is added Aluminum blades for better imaging Improved side-loading connection mechanism Ergonomically -

Miltex® Ophthalmic Instruments
OPHTHALmic INSTRUMENTS MILTEX ® OPHTHALMIC INSTRUMENTS The MILTEX® name is synonymous with unparalleled quality and service to our customers and surgical instrumentation produced with the utmost attention to consistent detail. The MILTEX® Ophthalmology product line includes both premium-grade German and American crafted stainless steel surgical instrumentation manufactured to exacting specifications. The surgical “feel” of our instruments, the outstanding cutting ability and the attention to delicate detail are just a few of the aspects that allow our products to outperform and stand out from the competition. This catalog presents our comprehensive offering of instruments necessary to support the innovative surgical techniques and advances in the field of Ophthalmology. In addition to our Ophthalmic offering, Miltex provides instruments to meet a variety of clinical needs for other specialties including: Plastic Surgery, Dermatology, Otolaryngology, Microsurgery, Gynecology, General Surgery as well as several other markets. General Information: Photographs in this catalog are close to actual size except where otherwise noted. Many illustrations are enlarged to show detail. Surgical instruments shown in this catalog are made of high quality surgical grade stainless steel, unless otherwise noted. Illustrations and content provide general description only and may be subject to change. Some products in this catalog may not be available for sale in the European Union. Miltex and Miltex Redefining Excellence are registered trademarks of Miltex, -

Surgery Instrumnts Khaled Khalilia Group 7
Surgery Instrumnts khaled khalilia Group 7 Scalpel handle blade +blade scalpel blade disposable fixed blade knife (Péan - Hand-grip : This grip is best for initial incisions and larger cuts. - Pen-grip : used for more precise cuts with smaller blades. - Changing Blade with Hemostat Liston Charrière Saw AmputationAmputati knife on knife Gigli Saw . a flexible wire saw used by surgeons for bone cutting .A gigli saw is used mainly for amputation surgeries. is the removal of a body extremity by trauma, prolonged constriction, or surgery. Scissors: here are two types of scissors used in surgeries.( zirconia/ ceramic,/ nitinol /titanium) . Ring scissors look much like standard utility scissors with two finger loops. Spring scissors are small scissors used mostly in eye surgery or microsurgery . Bandage scissors: Bandage scissors are angled tip scissors. helps in cutting bandages without gouging the skin. To size bandages and dressings. To cut through medical gauze. To cut through bandages already in place. Tenotomy Scissors: used to perform delicate surgery. used to cut small tissues They can be straight or curved, and blunt or sharp, depending upon necessity. operations in ophthalmic surgery or in neurosurgery. 10 c”m Metzenbaum scissors: designed for cutting delicate tissue come in variable lengths and have a relatively long shank-to-blade ratio blades can be curved or straight. the most commonly used scissors for cutting tissue. Use: ental, obstetrical, gynecological, dermatological, ophthalmological. Metzenbaum scissors Bandage scissors Tenotomy scissors Surgical scissors Forceps: Without teeth With teeth Dissecting forceps (Anatomical) With teeth: for tougher(hart) tissue: Fascia,Skin Without teeth: (atraumatic): for delicate tissues (empfindlich): Bowel Vessels. -

11 Cardiac Instruments
FEHLING AORTIC PUNCHES INS TRUMENTS AORTENSTANZEN 11/1 FEHLING... ... THE DIFFERENCE INSTRUMENTS FOR THORACIC, CARDIAC AND VASCULAR SURGERY INSTRUMENTE FÜR THORAX-, HERZ- UND GEFÄSSCHIRURGIE FEHLING Hanauer Landstraße 7A · 63791 Karlstein/Germany · www.fehling-instruments.de INSTRUMENTS +49(0) 6188 - 9574.40 +49(0) 6188 - 9574.45 [email protected] FEHLING STERNAL RETRACTORS INSTRUMENTS STERNUMSPREIZER 11/2 CALAFIORE STERNAL RETAINER STERNUMOFFENHALTER 1 1 ⁄2 ⁄4 1 1 1 ⁄16 ⁄2 ⁄2 STERNUM BLADE SCREW NUT STERNUMBLATT FLAT WRENCH STORAGE TRAY MUTTER GABELSCHLÜSSEL LAGERUNGS- LEFT RIGHT SINGLE USE BEHÄLTER LINKS RECHTS MPA-5 MPC-1L MPC-1R NEONATAL 7 x 30 mm** MPB-1 7 x 30 mm* 7 x 30 mm* Ø 8 MPC-0P MPB-7L MPB-7R 10 x 18 mm* 10 x 18 mm* MPA-6 “PEDIATRIC“ PEDIATRIC 45 x 65 mm** MPB-2 MPA-2L MPA-2R Ø 12 10 x 50 mm* 10 x 50 mm* MPA-3L MPA-3R ADULT 15 x 70 mm* 15 x 70 mm* MPA-9 45 x 65 mm** MPC-0A Ø 16 “ADULT“ MPA-4L MPA-4R ADIPOSIS 20 x 100 mm* 20 x 100 mm* MPA-7 70 x 90 mm** MPB-3 Ø 16 MPB-5L MPB-5R 15 x 30 mm* 15 x 30 mm* MPA-8 MPC-0C OSTEOPOROSIS 95 x 115 mm** “CURVED“ MPB-6L MPB-6R Ø 16 20 x 30 mm* 20 x 30 mm* *blade size / Blattgröße **opening width / Öffnungsweite exemplary configuration exemplary configuration Beispielkonfiguration Beispielkonfiguration ADULT - ADIPOSIS OSTEOPOROSIS FEHLING RETRACTORS INSTRUMENTS SPREIZER 11/3 TILTING KIPPBAR FOR PARTIAL STERNOTOMY FÜR PARTIELLE STERNOTOMIE BLADE SIZE BLATTGRÖSSE SPREADING WIDTH 160 mm a x b SPREIZWEITE 100 mm 35 x 50 mm MRM-5 45 x 50 mm MRM-6 215 mm 1 ⁄3 MARJAN 2 ⁄3 SUPERFLEX SOFT TISSUE RETRACTOR WEICHGEWEBERETRAKTOR 200 x 25 mm MTI-0 2 ⁄3 STERILISATION AND STORAGE TRAY FOR MTI-0 STERILISIER- UND LAGERSIEB FÜR MTI-0 220 x 51,2 x 19,5 mm MTK-0 FEHLING PROBES/SIZERS INSTRUMENTS SONDEN/LEHREN 11/6 SUPERPLAST A 45 mm A for mitral valve repair techniques without prosthetic ring SUPERPLAST instruments are construc- für Mitralklappenrekonstruktion ted of shape-memory metal. -

Surgical Products
Cervical & Endocervical Samplers Surgical Products Uterine Manipulation Devices Hysterectomy Instruments Laparoscopic Port-Site Closure Laparoscopic Instruments Laparoscopic Smoke Evacuation Laparoscopic Disposables Trocars Urology Instruments Retractors Delivering on the Promise to Help Clinicians Provide Better Health Care for Women Our mission is to enable physicians to provide increasingly more efficient and effective health care for women. We leverage our expertise in identifying and developing a steady stream of exceptional products that keep Ob/Gyns and others directly involved in caring for women, at the forefront of women’s health care. An Expansive Portfolio of Trusted Brands And Services Since our founding in 1990, CooperSurgical has researched, developed and manufactured a wide range of trusted brands that have advanced the standard of women’s health care. Our products are used by physicians and health care professionals in hospitals and their practices for a wide variety of procedures from basic annual gynecological exams to complex surgical procedures. As a full-service R&D and manufacturing company, we are committed to: • Improved patient outcomes and satisfaction • The highest quality and safety standards in the industry • Clinically proven technologies that provide ease of use • Technical support of our equipment – 20+ years of experience • Innovative solutions that reduce procedural costs • Annual support of medical professional educational organizations • Educational and in-service support of our products • Personalized service and a commitment to your satisfaction by educated professional representatives We appreciate the opportunity to partner with you to provide optimum health care for women. 2 To place an order, call us at: 800.243.2974 | Visit us online at: www.CooperSurgical.com About CooperSurgical Delivering on the Promise to Help Clinicians Provide Better Health Care for Women Industry-Leading Solutions for Laparoscopic and General Surgical Procedures CooperSurgical instruments are used every day in surgical procedures. -

Federal Chargemaster Price Transparency Edgewood (2).Xlsx
EDGEWOOD SURGICAL HOSPITAL CHARGES Federal reporting rules require hospitals to maintain a catalog of thousands of procedure codes, code descriptions and list prices in a complex accounting tool, known as the hospital chargemaster. The prices listed on the chargemaster do not reflect what patients will ultimately pay as insurance companies negotiate discounts on the list prices. In addition, co-pays, co-insurance and deductibles can also bring additional discounts before a final charge is determined. To get an accurate estimate of what your out of pocket expenses will be, contact us at (724) 646-0400, Monday through Friday, from 8 a.m. – 4:30 p.m. Chg Code Description Chg Amt 1 NF-HUMULIN R INJ SOLN 100U/1ML $61.61 99077 EXTENDED RECOVERY ROOM PER MINUTE $15.00 99078 OBSERVATION 1-4 HOURS $550.00 99079 OBSERVATION >5 HOURS **EACH** $15.00 99085 OR TIME PER MINUTE COMPLEX (>3 STAFF) $197.00 99086 OR TIME PER MINUTE MAJOR (3 STAFF) $136.00 99087 OR TIME PER MINUTE MINOR (1-2 STAFF) $93.00 99088 SURGICAL NEUROMONITORING $1,350.00 99089 SURGICAL EYE LASER $1,743.00 99090 PAIN MANAGEMENT PER MINUTE $187.00 99091 OR TIME PER MINUTE ADDITIONAL STAFF $1.00 99092 FORCE TRIAD RENTAL $350.00 99093 YAG LASER CHARGE $1,182.00 99094 PAIN MANAGEMENT PER MINUTE RF $326.00 99100 CONS SEDATION (SAME DOC) <5YR 30-MIN $302.00 99101 CONS SEDATION (SAME DOC) <5YR 30-MIN $302.00 99102 CONS SEDATION (SAME DOC) ADD'S 15-MIN $151.00 99103 CONS SEDATION (DIFF DOC) <5YR 30-MIN $302.00 99104 CONS SEDATION (DIFF DOC) >5 YR 30-MIN $302.00 99105 CONS SEDATION (DIFF -

Product Catalog
precision crafted quality PRODUCT CATALOG www.medicaldevicepurchase.com 1-916-663-4165 2 precision crafted quality A letter from our CEO: Medical Device Purchase is a company started by my father and me almost 10 years ago. We knew the road ahead for MDP would be challenging and that we would inevitably face giant corporations that had been established in the industry for decades. Many said we would not even last two years. However, our approach was different from our competitors. We wanted to create a friendlier environment for healthcare professionals searching for industry-leading surgical products. How? By providing more—and higher quality—options. Our mission was to provide a welcoming environment where customers could enjoy a uniquely approachable buying experience. We wanted to build a brand that focused on creating efficiency and reliability so that our clients could spend more time on the things that really matter. Dr. Ray, our co-founder, passed away earlier this year, but the legacy of Medical Device Purchase lives on as we continue to grow and expand as a cutting edge company blazing new trails in the world of surgical products. Sincerely, Orin Ray www.medicaldevicepurchase.com 3 About MDP WHO WE ARE AND WHAT WE DO Medical Device Purchase is a leading supplier of premium quality surgical products, committed to satisfying the ever-growing demands of the healthcare community. We provide a new level of reliability, efficiency, and value by using applications, performance products, and technology unlike any any other supplier in the the industry. OUR MISSION As the cost of healthcare continues to rise, MDP remain committed to reducing your overhead. -

Surgical Instruments
SURGICAL INSTRUMENTS I. CUTTING AND DISSECTING ~ Cutting and dissecting instruments are sharp and are used to cut body tissue or surgical supplies. deep knife Used to cut 7 handle with deep, delicate 15 blade tissue. inside knife 3 handle with Used to cut 10 blade superficial tissue. skin knife 4 handle with Used to cut skin. 20 blade A. KNIFE HANDLE Instruments Functions B. SCISSORS Straight Mayo Scissors Used to cut suture and supplies. Also known as: Suture scissors. Curved Mayo Scissors Used to cut heavy tissue (fascia, muscle, uterus, breast). Metzenbaum Scissors Used to cut delicate tissue. II. CLAMPING and OCCLUDING ~ Clamping and occluding instruments are used to compress blood vessels or hollow organs for hemostasis or to prevent spillage of contents. Instruments Functions Hemostat Other names: crile, snap or stat. A hemostat is used to clamp blood vessels or tag sutures. Its jaws may be straight or curved. Hemostat, Mosquito (left to right) A mosquito is used to clamp small blood vessels. Its jaws may be straight or curved. Kelly, Hemostat, Mosquito (left to right) Other names: Rochester Pean A Kelly is used to clamp larger vessels and tissue Burlisher Other names: Schnidt tonsil forcep, Adson forcep. A burlisher is used to clamp deep blood vessels. Burlishers have two closed finger rings. Burlishers with an open finger ring are called tonsil hemostats. Right Angle Other names: Mixter. A right angle is used to clamp hard-to-reach vessels and to place sutures behind or around a vessel. A right angle with a suture attached is called a "tie on a passer." Hemoclip applier with hemoclips A hemoclip applier with hemoclips applies metal clips onto blood vessels and ducts which will remain occluded. -

A Novel Right Ventricular Volume and Pressure Loaded Piglet Heart Model for the Study of Tricuspid Valve Function
Materials List for A Novel Right Ventricular Volume and Pressure Loaded Piglet Heart Model for the Study of Tricuspid Valve Function. Lily Q. Lin1, Sanaz Hatami2, James Yashu Coe1, Timothy M. Colen1, Consolato Sergi3, Richard Thompson4, Elena S. Di Martino5, Walter Herzog6, Ziad Abu Sara6, Darren H. Freed2, Nee Scze Khoo1 1Division of Pediatric Cardiology, Department of Pediatrics, University of Alberta 2Department of Surgery, University of Alberta 3Department of Laboratory Medicine and Pathology, University of Alberta 4Department of Biomedical Engineering, University of Alberta 5Department of Civil Engineering, University of Calgary 6Faculty of Kinesiology, University of Calgary Corresponding Author Citation Lily Q. Lin Lin, L.Q., Hatami, S., Coe, J.Y., Colen, T.M., Sergi, C., Thompson, R., Di Martino, E.S., [email protected] Herzog, W., Abu Sara, Z., Freed, D.H., Khoo, N.S. A Novel Right Ventricular Volume and Pressure Loaded Piglet Heart Model for the Study of Tricuspid Valve Function.. J. Vis. Exp. (), e61251, doi:10.3791/61251 (2020). Date Published DOI URL July 28, 2020 10.3791/61251 jove.com/video/61251 Materials Name Company Catalog Number Comments Drugs 1% lidocaine spray WDDC 103365 Lidodan 30 mL atropine sodium injection WDDC/Rafter 8 Products 0.5 mg/mL bupivacaine WDDC/Sterimax 5 mg/mL buprenorphine HCl slow release Chiron Compounding Pharmacy 1 mg/mL injection buprenorphine regular WDDC/Champion Alstoe 121378 Vetergesic 0.3 mg/mL cefazolin WDDC/Fresenius Kabi 102016 1 g/vial cephalexin capsule WDDC/Novopharm Novo-Lexin -

Fehling...The Difference
FEHLING AORTIC PUNCHES INS TRUMENTS AORTENSTANZEN 11/1 FEHLING... ... THE DIFFERENCE INSTRUMENTS FOR THORACIC, CARDIAC AND VASCULAR SURGERY INSTRUMENTE FÜR THORAX-, HERZ- UND GEFÄSSCHIRURGIE FEHLING Hanauer Landstraße 7A · 63791 Karlstein/Germany · www.fehling-instruments.de INSTRUMENTS +49(0) 6188 - 9574.40 +49(0) 6188 - 9574.45 [email protected] FEHLING STERNAL RETRACTORS INSTRUMENTS STERNUMSPREIZER 11/2 CALAFIORE STERNAL RETAINER STERNUMOFFENHALTER 1 1 ⁄2 ⁄4 1 1 1 ⁄16 ⁄2 ⁄2 STERNUM BLADE SCREW NUT STERNUMBLATT FLAT WRENCH STORAGE TRAY MUTTER GABELSCHLÜSSEL LAGERUNGS- LEFT RIGHT SINGLE USE BEHÄLTER LINKS RECHTS MPA-5 MPC-1L MPC-1R NEONATAL 7 x 30 mm** MPB-1 7 x 30 mm* 7 x 30 mm* Ø 8 MPC-0P MPB-7L MPB-7R 10 x 18 mm* 10 x 18 mm* MPA-6 “PEDIATRIC“ PEDIATRIC 45 x 65 mm** MPB-2 MPA-2L MPA-2R Ø 12 10 x 50 mm* 10 x 50 mm* MPA-3L MPA-3R ADULT 15 x 70 mm* 15 x 70 mm* MPA-9 45 x 65 mm** MPC-0A Ø 16 “ADULT“ MPA-4L MPA-4R ADIPOSIS 20 x 100 mm* 20 x 100 mm* MPA-7 70 x 90 mm** MPB-3 Ø 16 MPB-5L MPB-5R 15 x 30 mm* 15 x 30 mm* MPA-8 MPC-0C OSTEOPOROSIS 95 x 115 mm** “CURVED“ MPB-6L MPB-6R Ø 16 20 x 30 mm* 20 x 30 mm* *blade size / Blattgröße **opening width / Öffnungsweite exemplary configuration exemplary configuration Beispielkonfiguration Beispielkonfiguration ADULT - ADIPOSIS OSTEOPOROSIS FEHLING RETRACTORS INSTRUMENTS SPREIZER 11/3 TILTING KIPPBAR FOR PARTIAL STERNOTOMY FÜR PARTIELLE STERNOTOMIE BLADE SIZE BLATTGRÖSSE SPREADING WIDTH 160 mm a x b SPREIZWEITE 100 mm 35 x 50 mm MRM-5 45 x 50 mm MRM-6 215 mm 1 ⁄3 MARJAN 2 ⁄3 SUPERFLEX SOFT -
E-Mail : [email protected]
E-mail : [email protected] Web : www.medibiotek.com E-mail : [email protected] Web : www.medibiotek.com The company is managed by a team of experienced professionals who are well versed in operations with decades of experience in the health care field. The surgical equipment business of Medibiotek operates under the brand name of Pinaco and provides hospitals and surgeons with cutting edge equipment manufactured by the most advanced CNC machinery using the highest quality raw materials. The craftsmen who operate this equipment are renowned in the field with decades of experience and skills that have been passed down from one generation to the next. Skilled engineers also guide them and monitor the quality of the product at every step of the manufacturing process. At Health care institutions all across India, The Pinaco brand will continue to offer the most precise way for skilled surgeons to perform cutting edge surgeries with ease and precision. We will strive to build the same precision into our products just like surgeons who use precision on every surgery they perform. Our endeavour has always been and will continue to be to serve you with the most innovative products at the best value to you both in quality as well as affordability. E-mail : [email protected] Web : www.medibiotek.com Urology Instruments E-mail : [email protected] Web : www.medibiotek.com Bookwalter Retractor Ring Sizes Small 203mm x 311 URO1601 Medium 267mm x 368 URO 1602 BOOKWALTER RETRACTOR CLAMPS Universal Machanisms (Set of 4) URO 1604 Large 300mm -

Instruments for Cardiac and Vascular Surgery
Instruments for Cardiac and Vascular Surgery Aesculap Surgical Specialty Products - Cardiothoracic Instruments for Cardiac and Vascular Surgery OPERATE WITH GREATER PRECISION At Aesculap, we understand your practice faces evolving challenges from a rapidly aging patient population and increasingly complex diseases. For that reason, we are committed to delivering innovative cardiothoracic technologies, designed and manufactured with the same high standard of quality we have maintained for over 150 years. Our focus on solutions for minimally-invasive cardiothoracic surgery is driven by the desire to improve patient outcomes. In addition to our portfolio of cutting-edge technologies for beating heart coronary surgery, we offer a broad line of specialized instruments and retractors designed to meet the demanding needs of today’s cardiovascular, vascular and thoracic surgeons. In this catalog, you will find a select range of instruments that are commonly used in cardiac and vascular surgery. As the world’s largest instrument manufacturer, we are proud of our strict quality standards and meticulous workmanship that allow you to address challenging cardiac and vascular procedures with greater precision. The working surfaces of Aesculap DUROGRIP™ The non-reflective TITANIUM instruments the jaws of all needle holders have NOIR™ coating is six provide incomparable Dia Dust™ instruments jaws with high quality times as hard as normal operating sensitivity are coated with a fine tungsten carbide inserts. instrument steel, through light-weight layer of diamond dust, The smooth jaw surface providing increased handling. With a non- which results in a hard as well as the 0.2 mm resistance against both reflective finish and surface with high wear micro serration guarantee wear and corrosion.