Responding to British Columbia's Public Health Emergency
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Football Program 2020
FOOTBALL PROGRAM 2020 20 19 92nd SEASON OF Wesgroup is a proud supporter of Vancouver College’s Fighting Irish Football Team. FOOTBALL 5400 Cartier Street, Vancouver BC V6M 3A5 TABLE OF CONTENTS Principal’s Message ...............................................................2 Irish Football Team Awards 1941-2019 ..............................19 Head Coach’s Message .........................................................2 Irish Records 1986-2019 ......................................................22 Vancouver College Staff and Schedules 2020 .......................3 Irish Provincial Championship Game 2020 Fighting Irish Coaches and Supporting Staff ................4 Award Winners 1966-2018 .................................................29 Irish Alumni Currently Playing in the CFL and NFL ................5 Back in the Day ....................................................................29 2020 Fighting Irish Graduating Seniors .................................6 Irish Cumulative Record Against Opponents 1929-2018 .....30 Fighting Irish Varsity Statistical Leaders 2019 ......................8 Fighting Irish Varsity Football Team 2019 ...........................34 Vancouver College Football Awards 2019 .............................9 Irish Statistics 1996-2018 ...................................................35 Irish Varsity Football Academic Awards ...............................10 Archbishops’ Trophy Series 1957-2018 .............................38 Irish Academics 2020 ..........................................................10 -

BC Lacrosse Association/Sportsfunder
Vancouver Warriors and BC Lacrosse Association LACROSSE ON THE MOVE Youth Travel Grant Program The Vancouver Warriors are pleased to support the LACROSSE ON THE MOVE Youth Travel Grant Program. This fund has been created to assist teams and athletes who are traveling to provincial and national championships. The LACROSSE ON THE MOVE Youth Travel Grant Program will help offset travel costs for youth field and minor box lacrosse member associations of the BC Lacrosse Association, with the priority funding to assist Minor Box and Youth Field lacrosse teams traveling to provincial championships. LACROSSE ON THE MOVE Youth Travel Grant Fund Policy Guidelines The LACROSSE ON THE MOVE Committee comprised of the Vancouver Warriors and the BC Lacrosse Association have determined that grants from this fund will be available to teams traveling to youth field and minor box provincial championships; Team BC athletes who would not otherwise be able to afford to travel to Nationals; and Team BC athletes who would not otherwise be able to afford to travel to practices while preparing for National Championships. The LACROSSE ON THE MOVE Committee will review applications and make decisions on the allocations of the Youth Travel Grant Fund that will offset travel costs with priority funding going to Minor Box and Youth Field Lacrosse member teams and to Team BC athletes who face financial barriers and would not be able to participate without this assistance. The travel grants will partially subsidize travel costs: 1. Within British Columbia for minor box/youth field TEAMS traveling a distance of not less than 200 km, unless ferry travel is involved in the travel expenses. -

FOOTBALL PROGRAM 2019 91Th SEASON OF
FOOTBALL PROGRAM 2019 91th SEASON OF FOOTBALL 5400 Cartier Street, Vancouver BC V6M 3A5 TABLE OF CONTENTS Growth of $10,000 since July 2003 Principal’s Message ...............................................................2 Irish Football Team Awards 1941-2018 ..............................23 TARGET ASSET ALLOCATION Head Coach’s Message .........................................................2 Irish Records 1986-2018 ......................................................26 $35,000 Vancouver College Staff and Schedules 2018 .......................3 Fighting Irish Junior Varsity Football Team 2019 ................34 $30,000 $30,072 2019 Fighting Irish Coaches and Supporting Staff ................4 Fighting Irish Varsity Football Team 2019 ...........................35 Fighting Irish Football Alumni Where are they now? ...........5 Irish Provincial Championship Game Award Winners 1966-2018 .................................................37 $25,000 2019 Fighting Irish Graduating Seniors .................................6 In Memory .............................................................................8 Back in the Day ....................................................................37 $20,000 Irish Alumni Currently Playing in the CFL and NFL ..............10 Irish Cumulative Record Against Opponents 1929-2018 .....38 Fighting Irish Varsity Statistical Leaders 2018 ....................12 Irish Statistics 1996-2018 ...................................................39 $15,000 Vancouver College Football Awards 2018 ..........................13 -

(“TOU”) Apply to Your Use of Vancouve
Updated as of October 10 2018 Terms Of Use The following terms of use (“TOU”) apply to your use of www.canucks.com, vancouverwarriors.com, rogersarena.com and www.thesportsbar.ca and all subdomains thereof, the Canucks mobile application and all other websites, applications and online services that display or provide an authorized link to the TOU (each a “Website” and collectively, the "Websites"), including your use of or access to the Services and the Content (each as defined below) available through the Websites. The Websites are owned or controlled by the entities which collectively operate as Canucks Sports & Entertainment, Rogers Arena and The Sportsbar Live! at Rogers Arena. These entities consist of Vancouver Canucks Limited Partnership, Vancouver Arena Limited Partnership, Aquilini Vancouver Lacrosse Limited Partnership, Aquilini Food Services Limited Partnership and Aquilini Sports Bar Limited Partnership (collectively, the “CSE Parties”). Please read the TOU carefully before using or accessing the Websites, the Services or the Content. By using or accessing the Websites, the Services or the Content, you signify your agreement to the TOU. Your use of or access to the Websites, the Services or the Content is also subject to all applicable laws and regulations. If you do not agree to any of the terms and conditions in the TOU, you should not use the Websites, the Services or the Content. Your use of the Websites, the Services and the Content is also governed by our Privacy Policy, which is available through a link on the Websites. 1. TERMS OF USE The CSE Parties provide the Websites, the Services and the Content to you subject to the following TOU. -

Introducing the Vancouver Titans: the New Overwatch League Team Competing in the 2019 Season
For Immediate Release: December 1, 2018 INTRODUCING THE VANCOUVER TITANS: THE NEW OVERWATCH LEAGUE TEAM COMPETING IN THE 2019 SEASON Logo and team colours designed to showcase the natural beauty of the Pacific Northwest Vancouver, B.C – The Aquilini Group is proud to present Vancouver’s new esports team: the Vancouver Titans of the Overwatch League. The team’s visual identity takes on a local feel, highlighting colours, geographical elements, and folklore associated with the West Coast. The team’s roster, management, and branding were officially unveiled today at Rogers Arena before thousands of fans watching the National Hockey League game between the Vancouver Canucks and the Dallas Stars. The Titans new brand can be seen on Twitter @VancouverTitans, on Instagram @VancouverTitans_, on Facebook @VancouverTitans, and on Twitch @Vancouver_OWL.* Vancouver will compete for the Overwatch League championship when the 2019 season starts on February 14, 2019. “We are thrilled to officially launch the Titans today and to bring a premier global esports team to Vancouver,” said Francesco Aquilini, managing director of the Aquilini Group. “In choosing our identity we wanted to introduce a team that would resonate with fans in the Pacific Northwest. With a local feel and an experienced, skilled team, we are ready and can’t wait to have the Titans compete at the highest level in esports.” Titans Identity The Vancouver Titans colours will be blue (primary), green (secondary), and white (accents) to represent Vancouver’s greenery surrounded by the Pacific Ocean. The colour shades signify a vibrant, contemporary take on the Vancouver Canucks palette, but still allow the Titans to develop their own West Coast style. -

Spr Bios for 2-19
SPRINGFIELD THUNDERBIRDS: COACHES BIOS GEORDIE KINNEAR - HEAD COACH Geordie Kinnear joins the Springfield Thunderbirds as head coach after serving as an AHL assistant coach since 2001. Kinnear began his coaching career with the Albany River Rats following an eight South Division -year professional playing career and also served as a special assignment scout for the New Jersey Devils during the 2004-05 season. After he played three seasons of junior hockey for the Peterborough Petes of the Ontario Hockey League, the New Jersey Devils drafted Kinnear in the seventh round (162nd overall) of the 1992 NHL Entry Draft. Beginning with the 1993-94 season, he skated with Albany for the first six years of his career, helping the team reach the playoffs each season. Over that time, he was a member of Albany’s 1995 Calder Cup championship team, appeared in four consecutive AHL All-Star Classics (1995-1999) and served as team captain for three seasons (1996-1999). Kinnear signed with the Atlanta Thrashers as a free agent in August of 1999, making his National Hockey League debut by appearing in four games with Atlanta, posting a total of 13 penalty minutes. He split the 1999-2000 season between Atlanta and the Thrashers’ IHL affiliate, the Orlando Solar Bears. After starting the 2000-01 season with Orlando, he was traded back to New Jersey on Nov. 6, 2000, and played 14 games with Albany before being forced to retire due to injury in December of 2000. A defenseman originally from Simcoe, Ontario, Kinnear totaled 30 goals, 68 assists and 1,094 penalty minutes over the course of 406 career AHL games with Albany. -

SPORT-SCAN DAILY BRIEF NHL 10/29/2020 Anaheim Ducks Nashville Predators 1180010 AHL Targets Feb
SPORT-SCAN DAILY BRIEF NHL 10/29/2020 Anaheim Ducks Nashville Predators 1180010 AHL targets Feb. 5 for start of coronavirus-delayed 2020- 1180037 Predators sign contract for community ice rink in 21 season Downtown Clarksville MPEC 1180038 The Predators have plenty of cap space, so how can they Arizona Coyotes weaponize it? 1180011 Report: Arizona Coyotes' Ekman-Larsson glad to remain with team after trade talk Ottawa Senators 1180039 The Belleville Senators will have to be patient as AHL Boston Bruins targets Feb. 5 for start date 1180012 Bruce Cassidy weighs in on Bruins’ roster 1180040 GARRIOCH: Ottawa Senators sign free agent Alex 1180013 The Beanpot Four, sidelined: College hockey in Boston Galchenyuk to one-year deal waits, hopes for a season 1180041 How much did the Senators actually improve this offseason? Buffalo Sabres 1180014 OHL's reported plan to hold season provides clarity for Pittsburgh Penguins Sabres, Jack Quinn 1180042 AHL moves target date for opening of 2020-21 season to 1180015 Rochester Americans' season could begin as early as Feb. 5 Feb. 5 San Jose Sharks Calgary Flames 1180043 AHL anticipates February start to 2021 season, nearly 11 1180016 Heat, AHL set new return-to-play date for February months after coronavirus shutdown Colorado Avalanche St Louis Blues 1180017 Devon Toews’ contract could impact the Avalanche in the 1180044 Blues' focus turns to 'Return to Play 2.0' expansion draft Toronto Maple Leafs Columbus Blue Jackets 1180045 American Hockey League’s 31 teams aim to open next 1180018 Blue Jackets' Kevin -
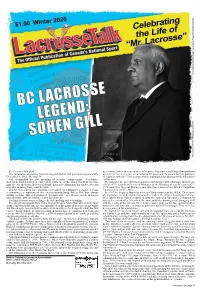
Winter 2020 Issue
By: LacrosseTalk Staff one season. Sohen then spent time in Victoria, Vancouver and Coquitlam uniforms The BC sports community has lost a legend. Sohen Gill passed away peacefully over the next seven years, accumulating 65 goals and 76 assists for 141 points in December 6, 2019. He was 78. 111 games. After the 1969 season, Sohen mothballed his playing stick, but not his Gill exemplified the true meaning of lacrosse volunteerism. Passionate, enthusiasm. dedicated, hard-working, a leader and mentor are of the many words to describe He took over the roles of Coach and General Manager of the Burnaby Junior team him. He was the heart and soul of the BC Lacrosse community for six decades and (1970-1972), Coach and General Manager of the Burnaby Senior B team (1972- a mentor to many from coast to coast. 1976) and then General Manager and sometime Coach of the WLA’s Coquitlam If there was a need for a position to be filled, to administer a league, a team, Adanacs club (1977-1986). a committee, a tournament, the ever-accommodating Sohen Gill was always In 1987, he began a four-year term as Commissioner of the WLA. Then came willing to help. This self-professed “lacrosse nut” as a player, coach, manager, the nightmare every firefighter faces on December 29, 1990. A lieutenant in charge administrator, official, volunteer, and fan did it all. of a ladder truck, Sohen scrambled onto the roof of a Vancouver restaurant to For him, lacrosse was a calling -- he did anything and everything. assess the extent of a fire when the roof suddenly disintegrated, plunging Gill The son of immigrants from India, Gill grew up in North Burnaby a block away into the centre of the inferno. -

SPORT-SCAN DAILY BRIEF NHL 4/22/2020 Anaheim Ducks Edmonton Oilers 1173829 a Look at the Ducks’ First-Round Draft Picks Through the 1173856 Gretzky Vs
SPORT-SCAN DAILY BRIEF NHL 4/22/2020 Anaheim Ducks Edmonton Oilers 1173829 A look at the Ducks’ first-round draft picks through the 1173856 Gretzky vs. Ovechkin should be fun on Xbox One years 1173857 One-on-one with Wayne Gretzky: On the time he visited Moscow during the Cold War Arizona Coyotes 1173858 Lowetide: Adam Larsson’s Oilers future uncertain as ‘sexy’ 1173830 Arizona Coyotes forward Nick Schmaltz 'just trying to get options emerge through' NHL quarantine period 1173831 Who stays, who goes? A speculative projection of the Los Angeles Kings Coyotes’ 2020-21 roster 1173859 Hockey star Hayley Wickenheiser earns her biggest assist during COVID-19 pandemic Boston Bruins 1173860 L.A. teams join forces to raise funds to help those affected 1173832 2010-11 Bruins get together (virtually) to watch Stanley by coronavirus Cup clincher 1173861 LOCAL TEAMS ALIGN TO CREATE “TEAMS FOR LA” 1173833 Charlie McAvoy recalls his Bruins debut TO BENEFIT THE MAYOR’S FUND FOR LOS ANGELES 1173834 Replica of Bobby Orr statue is being raffled to benefit pandemic workers Minnesota Wild 1173835 Charlie McAvoy discussed all things Bruins during video 1173862 Retold Glen Sonmor hockey stories still among the best town hall meeting 1173863 ‘This really is ours’: The Wild’s thrilling 2014 Game 7 OT 1173836 Bruce Cassidy: Age won’t necessarily hinder Bruins if NHL win, in their words resumes 1173837 This Day in Bruins History: Boston beats up on rival Montreal Canadiens Montreal Canadiens 1173864 Canadiens sign goaltender Vasili Demchenko to one-year 1173838 -

2017-18 AHL Regular Season
TORONTO MARLIES VS STOCKTON HEAT Wednesday, February 24, 2021 Scotiabank Saddledome — Calgary, AB 6:00 p.m. (MST) — AHL Game #406 RECORD: 4-2-0-0 RECORD: 0-2-0-0 TEAM GAME: 7 HOME RECORD: 0-0-0-0 TEAM GAME: 3 HOME RECORD: 0-2-0-0 AWAY GAME: 7 AWAY RECORD: 4-2-0-0 HOME GAME: 3 AWAY RECORD: 0-0-0-0 # GOALTENDER GP W L OT GAA SV% # GOALTENDER GP W L OT GAA SV% 1 Ian Scott 0 0 0 0 0.00 0.000 1 Louis Domingue 0 0 0 0 0.00 0.000 29 Andrew D'Agostini 6 4 2 0 1.86 0.933 30 Hayden Lavigne 0 0 0 0 0.00 0.000 31 Jeremy Link 0 0 0 0 0.00 0.000 31 Max Paddock 0 0 0 0 0.00 0.000 45 Kai Edmonds 0 0 0 0 0.00 0.000 32 Dustin Wolf 1 0 1 0 10.65 0.545 40 Garret Sparks 2 0 1 0 4.57 0.841 # P PLAYER GP G A P SOG PIM # P PLAYER GP G A P SOG PIM 6 D Teemu Kivihalme 6 1 2 3 12 6 2 D Connor Mackey 2 0 0 0 1 0 7 D Timothy Liljegren 6 0 5 5 14 4 3 D Greg Moro 0 0 0 0 0 0 10 LW Zack Trott 2 0 0 0 0 0 5 D Colton Poolman 2 0 0 0 4 0 11 C Kalle Kossila 0 0 0 0 0 0 6 D Alex Petrovic 2 0 0 0 3 2 12 RW Jeremy McKenna 2 0 2 2 2 0 7 D Noah King 0 0 0 0 0 0 14 C Adam Brooks 6 2 5 7 14 4 8 D Zach Leslie 2 0 0 0 2 2 15 C Rourke Chartier 6 0 3 3 9 0 11 RW Matthew Phillips 2 0 0 0 1 0 17 LW Rich Clune 6 2 0 2 6 12 14 D CJ Lerby 2 0 0 0 1 0 18 LW Kenny Agostino 6 2 5 7 18 2 16 C Mark Simpson 1 0 1 1 1 0 19 RW Gordie Green 0 0 0 0 0 0 17 RW Dmitry Zavgorodniy 2 0 0 0 3 0 21 D Joseph Duszak 6 1 3 4 10 0 20 LW Alex Gallant 2 1 0 1 3 7 24 RW Cole MacKay 0 0 0 0 0 0 22 RW Giorgio Estephan 0 0 0 0 0 0 25 D Dakota Krebs 0 0 0 0 0 0 23 LW Justin Kirkland 2 0 0 0 6 0 27 D Riley McCourt -

For Release Vancouver Sports
FOR RELEASE VANCOUVER SPORTS STARS AND PROVINCIAL REC LEADERS TEAM UP FOR FAMILIES WITH AUTISM Vancouver, BC – For the first time in Vancouver sports history, Canucks Autism Network (CAN) will bring all five professional sports teams together with provincial sport organizations for an unforgettable family event. On Sunday, May 12th, from 1:00-4:00 pm, over 250 families living with autism (850 individuals) will hit the field at BC Place for the 7th Annual CAN Sports Day, sponsored by Centaur Products Sports Contracting, The DB Perks Group and BC Place. As in previous years, professional players, alumni and mascots from the Vancouver Canucks, BC Lions, Vancouver Whitecaps FC and Vancouver Canadians will lead activity stations at the multisport event. New this year: The Vancouver Warriors will join the fold alongside BC Rugby, British Columbia Golf, BC Athletics, Tennis BC, Lacrosse BC and Jays Care Foundation Challenger Baseball. Confirmed athletes include: Antoine Roussel & Manny Malhotra - Vancouver Canucks Jake Nerwiknski & Brett Levis – Vancouver Whitecaps FC Jordan Herdman & Claudell Louis – BC Lions Professional sports heroes and community rec leaders alike will lead children, youth and young adults with autism in an unprecedented array of sports activities. In addition to giving CAN participants a truly memorable experience, the hope is to connect hundreds of individuals and families living with autism to a greater range of community-based sports organizations and spark a lifetime of physical activity. “Individuals with autism face many barriers for participating in community recreation,” says Stephanie Jull, Canucks Autism Network’s VP of Programs, Training and Community Engagement. “By uniting an entire community of BC sports leaders, we can work together to take individuals with autism off the sidelines and back into the field of play.” Media are invited to attend between 1:15pm and 3:45 pm and are asked to enter through the East Gate entrance. -

Vancouver Warriors and BC Lacrosse Association LACROSSE on the MOVE Youth Travel Grant Program
Vancouver Warriors and BC Lacrosse Association LACROSSE ON THE MOVE Youth Travel Grant Program The Vancouver Warriors are pleased to support the LACROSSE ON THE MOVE Youth Travel Grant Program. This fund has been created to assist teams and athletes who are traveling to provincial and national championships. The LACROSSE ON THE MOVE Youth Travel Grant Program will help offset travel costs for youth field and minor box lacrosse member associations of the BC Lacrosse Association, with the priority funding to assist Minor Box and Youth Field lacrosse teams traveling to provincial championships. LACROSSE ON THE MOVE Youth Travel Grant Fund Policy Guidelines The LACROSSE ON THE MOVE Committee comprised of the Vancouver Warriors and the BC Lacrosse Association have determined that grants from this fund will be available to teams traveling to youth field and minor box provincial championships; Team BC athletes who would not otherwise be able to afford to travel to Nationals; and Team BC athletes who would not otherwise be able to afford to travel to practices while preparing for National Championships. The LACROSSE ON THE MOVE Committee will review applications and make decisions on the allocations of the Youth Travel Grant Fund that will offset travel costs with priority funding going to Minor Box and Youth Field Lacrosse member teams and to Team BC athletes who face financial barriers and would not be able to participate without this assistance. The travel grants will partially subsidize travel costs: 1. Within British Columbia for minor box/youth field TEAMS traveling a distance of not less than 200 km, unless ferry travel is involved in the travel expenses.