PNHP Newsletter Spring 2016 PHYSICIANS for a NATIONAL HEALTH PROGRAM ▪ 29 E
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Event Winners
Meet History -- NCAA Division I Outdoor Championships Event Winners as of 6/17/2017 4:40:39 PM Men's 100m/100yd Dash 100 Meters 100 Meters 1992 Olapade ADENIKEN SR 22y 292d 10.09 (2.0) +0.09 2017 Christian COLEMAN JR 21y 95.7653 10.04 (-2.1) +0.08 UTEP {3} Austin, Texas Tennessee {6} Eugene, Ore. 1991 Frank FREDERICKS SR 23y 243d 10.03w (5.3) +0.00 2016 Jarrion LAWSON SR 22y 36.7652 10.22 (-2.3) +0.01 BYU Eugene, Ore. Arkansas Eugene, Ore. 1990 Leroy BURRELL SR 23y 102d 9.94w (2.2) +0.25 2015 Andre DE GRASSE JR 20y 215d 9.75w (2.7) +0.13 Houston {4} Durham, N.C. Southern California {8} Eugene, Ore. 1989 Raymond STEWART** SR 24y 78d 9.97w (2.4) +0.12 2014 Trayvon BROMELL FR 18y 339d 9.97 (1.8) +0.05 TCU {2} Provo, Utah Baylor WJR, AJR Eugene, Ore. 1988 Joe DELOACH JR 20y 366d 10.03 (0.4) +0.07 2013 Charles SILMON SR 21y 339d 9.89w (3.2) +0.02 Houston {3} Eugene, Ore. TCU {3} Eugene, Ore. 1987 Raymond STEWART SO 22y 80d 10.14 (0.8) +0.07 2012 Andrew RILEY SR 23y 276d 10.28 (-2.3) +0.00 TCU Baton Rouge, La. Illinois {5} Des Moines, Iowa 1986 Lee MCRAE SO 20y 136d 10.11 (1.4) +0.03 2011 Ngoni MAKUSHA SR 24y 92d 9.89 (1.3) +0.08 Pittsburgh Indianapolis, Ind. Florida State {3} Des Moines, Iowa 1985 Terry SCOTT JR 20y 344d 10.02w (2.9) +0.02 2010 Jeff DEMPS SO 20y 155d 9.96w (2.5) +0.13 Tennessee {3} Austin, Texas Florida {2} Eugene, Ore. -
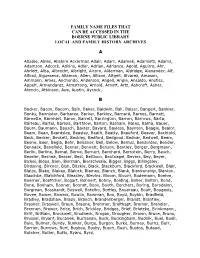
Family Name Files That Can Be Accessed in the Boerne Public Library Local and Family History Archives
FAMILY NAME FILES THAT CAN BE ACCESSED IN THE BOERNE PUBLIC LIBRARY LOCAL AND FAMILY HISTORY ARCHIVES A Abadie, Ables, Abshire Ackerman Adair, Adam, Adamek, Adamietz, Adams, Adamson, Adcock, Adkins, Adler, Adrian, Adriance, Agold, Aguirre, Ahr, Ahrlett, Alba, Albrecht, Albright, Alcorn, Alderman, Aldridge, Alexander, Alf, Alford, Algueseva, Allamon, Allen, Allison, Altgelt, Alvarez, Amason, Ammann, Ames, Anchondo, Anderson, Angell, Angle, Ansaldo, Anstiss, Appelt, Armendarez, Armstrong, Arnold, Arnott, Artz, Ashcroft, Asher, Atencio, Atkinson, Aue, Austin, Aycock, B Backer, Bacon, Bacorn, Bain, Baker, Baldwin, Ball, Balser, Bangert, Bankier, Banks, Bannister, Barbaree, Barker, Barkley, Barnard, Barnes, Barnett, Barnette, Barnhart, Baron, Barrett, Barrington, Barron, Barrows, Barta, Barteau, Bartel, Bartels, Barthlow, Barton, Basham, Bates, Batha, Bauer, Baum, Baumann, Bausch, Baxter, Bayard, Bayless, Baynton, Beagle, Bealor, Beam, Bean, Beardslee, Beasley, Beath, Beatty, Beauford, Beaver, Bechtold, Beck, Becker, Beckett, Beckley, Bedford, Bedgood, Bednar, Bedwell, Beem, Beene, Beer, Begia, Behr, Beissner, Bell, Below, Bemus, Benavides, Bender, Bennack, Benefield, Benner, Bennett, Benson, Bentley, Berger, Bergmann, Berlin, Berline, Bernal, Berne, Bernert, Bernhard, Bernstein, Berry, Besch, Beseler, Beshea, Besser, Best, Bettison, Beutnagel, Bevers, Bey, Beyer, Bickel, Bidus, Bien, Bierman, Bierschwale, Bigger, Biggs, Billingsley, Birdsong, Birkner, Bish, Bitzkie, Black, Blackburn, Blackford, Blackwell, Blair, Blaize, Blake, Blakey, Blalock, -

The German Surname Atlas Project ± Computer-Based Surname Geography Kathrin Dräger Mirjam Schmuck Germany
Kathrin Dräger, Mirjam Schmuck, Germany 319 The German Surname Atlas Project ± Computer-Based Surname Geography Kathrin Dräger Mirjam Schmuck Germany Abstract The German Surname Atlas (Deutscher Familiennamenatlas, DFA) project is presented below. The surname maps are based on German fixed network telephone lines (in 2005) with German postal districts as graticules. In our project, we use this data to explore the areal variation in lexical (e.g., Schröder/Schneider µtailor¶) as well as phonological (e.g., Hauser/Häuser/Heuser) and morphological (e.g., patronyms such as Petersen/Peters/Peter) aspects of German surnames. German surnames emerged quite early on and preserve linguistic material which is up to 900 years old. This enables us to draw conclusions from today¶s areal distribution, e.g., on medieval dialect variation, writing traditions and cultural life. Containing not only German surnames but also foreign names, our huge database opens up possibilities for new areas of research, such as surnames and migration. Due to the close contact with Slavonic languages (original Slavonic population in the east, former eastern territories, migration), original Slavonic surnames make up the largest part of the foreign names (e.g., ±ski 16,386 types/293,474 tokens). Various adaptations from Slavonic to German and vice versa occurred. These included graphical (e.g., Dobschinski < Dobrzynski) as well as morphological adaptations (hybrid forms: e.g., Fuhrmanski) and folk-etymological reinterpretations (e.g., Rehsack < Czech Reåak). *** 1. The German surname system In the German speech area, people generally started to use an addition to their given names from the eleventh to the sixteenth century, some even later. -
UNIVERSITY of NOTRE DAME TRACK and FIELD HISTORY & RECORDS Men’S All-Americans Notes: All Finishes, If Available, Are Indicated in Parentheses
UNIVERSITY OF NOTRE DAME TRACK AND FIELD HISTORY & RECORDS Men’s All-Americans Notes: All finishes, if available, are indicated in parentheses. The distance medley relay, one-mile run (after 1965), two-mile relay, 55 meters, 60 meters, 55-meter hurdles, 60-meter hurdles and 3,000-meter run are indoor events only. All other indoor events are indicated. If no indoor indication exists, the event is outdoor. (y – yards; m – meters) 1921 Greg Rice .................Mile (4th), Two-Mile (1st) 1966 1994 Gus Desch ....................220y Low Hurdles (1st) 1941 Ed Dean .............................................Mile (3rd) Randy Kinder .................... Indoor 200m (10th) Billy Hayes ....................100y (2nd), 220y (4th) Jim Delaney ................................Shot Put (4th) Pete Farrell......880y (6th), Indoor 1,000y (4th) 1995 Johnny Murphy .......................High Jump (1st) John O’Rourke ........................High Jump (3rd) 1967 Eugene Oberst ...............................Javelin (1st) John Cowan ......................Steeplechase (11th) Chet Wynne ................120y High Hurdles (4th) 1942 Pete Farrell............................Indoor 880y (6th) Mike McWilliams .....................10,000m (14th) Allen Rossum....................................55m (7th) 1922 Frank Conforti ................................... Mile (4th) 1968 Jim Delaney ................................Shot Put (3rd) Ed Broderick ........................High Jump (t-4th) 1996 Billy Hayes ...................100y (2nd), 220y (2nd) Oliver Hunter .......................... -

Family Group Sheets Surname Index
PASSAIC COUNTY HISTORICAL SOCIETY FAMILY GROUP SHEETS SURNAME INDEX This collection of 660 folders contains over 50,000 family group sheets of families that resided in Passaic and Bergen Counties. These sheets were prepared by volunteers using the Societies various collections of church, ceme tery and bible records as well as city directo ries, county history books, newspaper abstracts and the Mattie Bowman manuscript collection. Example of a typical Family Group Sheet from the collection. PASSAIC COUNTY HISTORICAL SOCIETY FAMILY GROUP SHEETS — SURNAME INDEX A Aldous Anderson Arndt Aartse Aldrich Anderton Arnot Abbott Alenson Andolina Aronsohn Abeel Alesbrook Andreasen Arquhart Abel Alesso Andrews Arrayo Aber Alexander Andriesse (see Anderson) Arrowsmith Abers Alexandra Andruss Arthur Abildgaard Alfano Angell Arthurs Abraham Alje (see Alyea) Anger Aruesman Abrams Aljea (see Alyea) Angland Asbell Abrash Alji (see Alyea) Angle Ash Ack Allabough Anglehart Ashbee Acker Allee Anglin Ashbey Ackerman Allen Angotti Ashe Ackerson Allenan Angus Ashfield Ackert Aller Annan Ashley Acton Allerman Anners Ashman Adair Allibone Anness Ashton Adams Alliegro Annin Ashworth Adamson Allington Anson Asper Adcroft Alliot Anthony Aspinwall Addy Allison Anton Astin Adelman Allman Antoniou Astley Adolf Allmen Apel Astwood Adrian Allyton Appel Atchison Aesben Almgren Apple Ateroft Agar Almond Applebee Atha Ager Alois Applegate Atherly Agnew Alpart Appleton Atherson Ahnert Alper Apsley Atherton Aiken Alsheimer Arbuthnot Atkins Aikman Alterman Archbold Atkinson Aimone -

Surname Folders.Pdf
SURNAME Where Filed Aaron Filed under "A" Misc folder Andrick Abdon Filed under "A" Misc folder Angeny Abel Anger Filed under "A" Misc folder Aberts Angst Filed under "A" Misc folder Abram Angstadt Achey Ankrum Filed under "A" Misc folder Acker Anns Ackerman Annveg Filed under “A” Misc folder Adair Ansel Adam Anspach Adams Anthony Addleman Appenzeller Ader Filed under "A" Misc folder Apple/Appel Adkins Filed under "A" Misc folder Applebach Aduddell Filed under “A” Misc folder Appleman Aeder Appler Ainsworth Apps/Upps Filed under "A" Misc folder Aitken Filed under "A" Misc folder Apt Filed under "A" Misc folder Akers Filed under "A" Misc folder Arbogast Filed under "A" Misc folder Albaugh Filed under "A" Misc folder Archer Filed under "A" Misc folder Alberson Filed under “A” Misc folder Arment Albert Armentrout Albight/Albrecht Armistead Alcorn Armitradinge Alden Filed under "A" Misc folder Armour Alderfer Armstrong Alexander Arndt Alger Arnold Allebach Arnsberger Filed under "A" Misc folder Alleman Arrel Filed under "A" Misc folder Allen Arritt/Erret Filed under “A” Misc folder Allender Filed under "A" Misc folder Aschliman/Ashelman Allgyer Ash Filed under “A” Misc folder Allison Ashenfelter Filed under "A" Misc folder Allumbaugh Filed under "A" Misc folder Ashoff Alspach Asper Filed under "A" Misc folder Alstadt Aspinwall Filed under "A" Misc folder Alt Aston Filed under "A" Misc folder Alter Atiyeh Filed under "A" Misc folder Althaus Atkins Filed under "A" Misc folder Altland Atkinson Alwine Atticks Amalong Atwell Amborn Filed under -
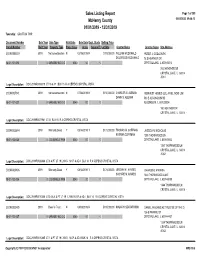
Sales Report
Sales Listing Report Page 1 of 309 McHenry County 05/04/2020 09:46:13 01/01/2019 - 12/31/2019 Township: GRAFTON TWP Document Number Sale Year Sale Type Valid Sale Sale Date Dept. Study Selling Price Parcel Number Built Year Property Type Prop. Class Acres Square Ft. Lot Size Grantor Name Grantee Name Site Address 2019R0006019 2019 Not advertised on mN 02/19/2019 N $115,000.00 WILLIAM MCDONALD PETER J. GODLEWSKI DOLORESS MCDONALD 78 S HEATHER DR 18-01-101-013 0 GARAGE/ NO O O 0040 .00 0 CRYSTAL LAKE, IL 600145018 78 S HEATHER DR CRYSTAL LAKE, IL 60014 -5018 Legal Description: DOC 2019R0006019 LT 16 & 17 BLK 15 R A CEPEKS CRYSTAL VISTA 2019R0027941 2019 Not advertised on mN 07/08/2019 N $150,000.00 CHARLES G. ALEMAN REINVEST HOMES LLC, AN ILLINOIS LIMIT DAWN S. ALEMAN 503 E ALGONQUIN RD 18-01-101-027 0 GARAGE/ NO O O 0040 .00 0 ALGONQUIN, IL 601023004 160 HEATHER DR CRYSTAL LAKE, IL 60014 - Legal Description: DOC 2019R0027941 LT 31 BLK 15 R A CEPEKS CRYSTAL VISTA 2019R0026844 2019 Warranty Deed Y 08/14/2019 Y $172,000.00 THOMAS M. COFFMAN JESSICA N. NICHOLAS KATRINA COFFMAN 1350 THORNWOOD LN 18-01-102-035 0 LDG SINGLE FAM 0040 .00 0 CRYSTAL LAKE, IL 600145042 1350 THORNWOOD LN CRYSTAL LAKE, IL 60014 -5042 Legal Description: DOC 2019R0026844 LT 6 & PT LT 19 LYING N OF & ADJ BLK 14 R A CEPEKS CRYSTAL VISTA 2019R0010406 2019 Warranty Deed Y 04/12/2019 Y $174,000.00 JEREMY M. -

Start Number Name Surname Team City, Country Time 11001 Tommy
Start number Name Surname Team City, Country Time 11001 Tommy Frølund Jensen Kongens lyngby, Denmark 89:20:46 11002 Emil Boström Lag Nord Linköping, Sweden 98:19:04 11003 Lovisa Johansson Lag Nord Burträsk, Sweden 98:19:02 11005 Maurice Lagershausen Huddinge, Sweden 102:01:54 11011 Hyun jun Lee Korea, (south) republic of 122:40:49 11012 Viggo Fält Team Fält Linköping, Sweden 57:45:24 11013 Richard Fält Team Fält Linköping, Sweden 57:45:28 11014 Rasmus Nummela Rackmannarna Pjelax, Finland 98:59:06 11015 Rafael Nummela Rackmannarna Pjelax, Finland 98:59:06 11017 Marie Zølner Hillerød, Denmark 82:11:49 11018 Niklas Åkesson Mellbystrand, Sweden 99:45:22 11019 Viggo Åkesson Mellbystrand, Sweden 99:45:22 11020 Damian Sulik #StopComplaining Siegen, Germany 101:13:24 11023 Bruno Svendsen Tylstrup, Denmark 74:48:08 11024 Philip Oswald Lakeland, USA 55:52:02 11025 Virginia Marshall Lakefield, Canada 55:57:54 11026 Andreas Mathiasson Backyard Heroes Ödsmål, Sweden 75:12:02 11028 Stine Andersen Brædstrup, Denmark 104:35:37 11030 Patte Johansson Tiger Södertälje, Sweden 80:24:51 11031 Frederic Wiesenbach BB Dahn, Germany 101:21:50 11032 Romea Brugger BB Berlin, Germany 101:22:44 11034 Oliver Freudenberg Heyda, Germany 75:07:48 11035 Jan Hennig Farum, Denmark 82:11:50 11036 Robert Falkenberg Farum, Denmark 82:11:51 11037 Edo Boorsma Sint annaparochie, Netherlands 123:17:34 11038 Trijneke Stuit Sint annaparochie, Netherlands 123:17:35 11040 Sebastian Keck TATSE Gieäen, Germany 104:08:01 11041 Tatjana Kage TATSE Gieäen, Germany 104:08:02 11042 Eun Lee -

Butler Alumnal Quarterly University Special Collections
Butler University Digital Commons @ Butler University Butler Alumnal Quarterly University Special Collections 1926 Butler Alumnal Quarterly (1926) Butler University Follow this and additional works at: https://digitalcommons.butler.edu/bualumnalquarterly Part of the Other History Commons Recommended Citation Butler University, "Butler Alumnal Quarterly (1926)" (1926). Butler Alumnal Quarterly. 14. https://digitalcommons.butler.edu/bualumnalquarterly/14 This Book is brought to you for free and open access by the University Special Collections at Digital Commons @ Butler University. It has been accepted for inclusion in Butler Alumnal Quarterly by an authorized administrator of Digital Commons @ Butler University. For more information, please contact [email protected]. THE BUTLER ALUMNAL QUARTERLY yjr ^'{ APRIL, 1926 INDIANAPOLIS Entered as second-class matter March 26, 1912, at the post office at Indianapolis, Ind., under the Act of March 3, 1879. CONTENTS The Beginnings of Butler College Lee Burns The Founders op Butler College Demarchus C. Brown Founders^ Day Dinner Talks Journalism at Butler College H. E. Birdsong The Modern College Professor Arthur G. Long The Divine Right of Alumni Monticello George A. Schumacher The Duffer's Hope—A poem Clarence L. Goodwin College News Harlan 0. Page From the City Office Athletics Recent College Affiliation Honored Students A Loved Landmark Moores' Lincoln Collection Butler Publications ''Butler Day" in Chicago Women's League Alumni Scholarships Commencement Class Reunions Butler DRIFT Personal Mention Marriages Births Deaths Notice Digitized by tine Internet Arciiive in 2010 witii funding from Lyrasis IVIembers and Sloan Foundation http://www.archive.org/details/butleralumnalqua15butl BU I LER ALUMNAL QUARTERLY Vol. XV APRIL, 1926 No. 1 THE BEGINNINGS OF BUTI.ER COLLEGE By Lee Burns A characteristic of the American people has been their con- stant interest in the cause of education. -

PNHP Newsletter Winter 2011 PHYSICIANS for a NATIONAL HEALTH PROGRAM » 29 E
PNHP Newsletter Winter 2011 PHYSICIANS FOR A NATIONAL HEALTH PROGRAM » 29 E. MADISON, SUITE 602, CHICAGO, IL 60602 » WWW.PNHP.ORG » WINTER 2011 NEWSLETTER Single-payer governor elected in Vermont; $56.5 million for 6 insurance CEOs while In Congress, H.R. 676 sponsors retained uninsured figure skyrockets to 50.7 million Vermont’s single-payer movement took a giant step forward on CEOs at six of the nation’s largest health insurers averaged Nov. 2 with the election of the pro-single-payer candidate for gover- $9.4 million in pay in 2009. Top earners included Aetna’s Ronald nor, Peter Shumlin. The state Legislature has already hired William Williams, who took home $15.3 million, including salary, incen- Hsiao, architect of Taiwan’s single-payer system, to design three tives, and stock options; WellPoint’s Angela Braly ($12.8 million); options for health reform, including a single-payer plan. PNHP’s Dr. UnitedHealth Group’s Stephen Hemsley ($9.5 million, on top of Deb Richter is mobilizing physician, grassroots and business support $99 million in stock option gains the previous year); Humana’s to make Vermont the first state to pass single payer. Funds are need- Michael B. McCallister ($6.2 million), Cigna’s David Cordani ed to hire organizers and to “immunize” Vermonters against an ($5.6 million) and Centene’s Michael Neidorff ($7.1 million) inevitable tide of propaganda from the insurance industry. (Wall Street Journal CEO Compensation Study, 11/16/10). California and Hawaii also elected gubernatorial candidates who The number of Americans without health insurance climbed to have supported single payer in the past – 50.7 million in 2009. -

Human Genetics and Clinical Aspects of Neurodevelopmental Disorders
bioRxiv preprint doi: https://doi.org/10.1101/000687; this version posted October 6, 2014. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Human genetics and clinical aspects of neurodevelopmental disorders Gholson J. Lyon1,2,3,*, Jason O’Rawe1,3 1Stanley Institute for Cognitive Genomics, One Bungtown Road, Cold Spring Harbor Laboratory, NY, USA, 11724 2Institute for Genomic Medicine, Utah Foundation for Biomedical Research, E 3300 S, Salt Lake City, Salt Lake City, UT, USA, 84106 3Stony Brook University, 100 Nicolls Rd, Stony Brook, NY, USA, 11794 * Corresponding author: Gholson J. Lyon Email: [email protected] Other author emails: Jason O'Rawe: [email protected] 1 bioRxiv preprint doi: https://doi.org/10.1101/000687; this version posted October 6, 2014. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. Introduction “our incomplete studies do not permit actual classification; but it is better to leave things by themselves rather than to force them into classes which have their foundation only on paper” – Edouard Seguin (Seguin, 1866) “The fundamental mistake which vitiates all work based upon Mendel’s method is the neglect of ancestry, and the attempt to regard the whole effect upon off- spring, produced by a particular parent, as due to the existence in the parent of particular structural characters; while the contradictory results obtained by those who have observed the offspring of parents apparently identical in cer- tain characters show clearly enough that not only the parents themselves, but their race, that is their ancestry, must be taken into account before the result of pairing them can be predicted” – Walter Frank Raphael Weldon (Weldon, 1902). -

Music in I Ndiaiiapolis, 1900-1944'
Music In I ndiaiiapolis, 1900-1944’ MARTHAF. EELLINGER Developments in music since nineteen hundred, which were based largely on the foundations pi’eviously laid, in- volved notable and significant advances. The outstanding features of this peviod are the establishment of the People’s Concert Association and the People’s Chorus, the foundation of the lndianapolis hranch of the National Federation of Music Clubs, the expansion of the Matinee Musicale, the rapid development of applied and theoretical music in the public schools, and the founding of the Indiana State Sym- phony Orchestra. In the early years of the century a group of citizens headed by Edward €3. Birge, Director of Music in the Public Schools, conceiving the idea oi offering good music, com- parable to that of the May fePtival days, on a non-profit sys- tem, and of making a bid for a larger audience, organized the People’s Concert Association. The sale of two or three thousand seats, at twenty-five or fifty cents each, would guarantee the engagement of fine artists, and at the same time afford opportunity for the production of major com- positions in which the local organizations would participate. Mindful of financial hazards, the committee at first sought and obtained eighty guarantors who promised to back the enterprise to the extent of ten dollars each, but as it turned out, no guarantor was ever asked to pay. The creation of an audience-a x:er*y large audience-was the crux of the problem, and it was solved iii a large measure by the fine co-operation of the puhlic school teaching staffs.