Dental Nanomaterials
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Effect of Cation Substitutions in an Ionomer Glass Composition on The
Effect of Cation Substitutions in an Ionomer Glass Composition on the Setting Reaction and Properties of the Resulting Glass Ionomer Cements By Mitra A. M. P. Kashani A thesis submitted to the University of Birmingham for the degree of DOCTOR OF PHILOSOPHY School of Metallurgy and Materials University of Birmingham April 2013 University of Birmingham Research Archive e-theses repository This unpublished thesis/dissertation is copyright of the author and/or third parties. The intellectual property rights of the author or third parties in respect of this work are as defined by The Copyright Designs and Patents Act 1988 or as modified by any successor legislation. Any use made of information contained in this thesis/dissertation must be in accordance with that legislation and must be properly acknowledged. Further distribution or reproduction in any format is prohibited without the permission of the copyright holder. Abstract This study investigated the effect of Ba2+ and Sr2+ substitutions for Ca2+ in an ionomer glass composition 4.5SiO2-3Al2O3-1.5P2O5-3CaO-2CaF2 on the setting reaction and properties of the resulting glass ionomer cements (GICs). Experimental GICs (Ca-GIC, Ca-Sr-GIC and Ca-Ba-GIC) were characterized via various techniques: Diametral tensile strength, compressive strength, flexural strength, Vickers hardness and nano-indentation measurements were conducted at different time points during setting. Real time Fourier transform infrared (FTIR) spectroscopy was used to study the effect of the glass composition on cement setting reactions. A resistance to penetration method evaluated the cement setting time. Additionally, the wear resistance of the experimental GIC was measured by a ball-on- flat wear test. -

Comprehensive Investigation on Fluorosilicate Glass Prepared By
330 Journal of The Electrochemical Society, 147 (1) 330-334 (2000) S0013-4651(99)04-019-7 CCC: $7.00 © The Electrochemical Society, Inc. Comprehensive Investigation on Fluorosilicate Glass Prepared by Temperature-Difference-Based Liquid-Phase Deposition Ching-Fa Yeh,z Yueh-Chuan Lee,* Kwo-Hau Wu, Yuh-Ching Su, and Su-Chen Lee Department of Electronics Engineering and Institute of Electronics, National Chiao Tung University, Hsinchu, Taiwan This study investigates the properties of fluorosilicate glass film prepared by temperature-difference-based liquid-phase deposition. Experimental results indicate that the deposition temperature can significantly affect the deposition rate and film properties. As the deposition temperature increases from 15 to 358C, the deposition rate increases exponentially from 30 to 687 Å/h. Meanwhile, the F and OH contents increase from 2.56 to 3.49% and from 0.16 to 0.5%, respectively. The dielectric constants and stresses for the films deposited at 15, 25, and 358C, are 3.56/63 MPa, 3.46/43 MPa, and 3.66/73 MPa, respectively. The current densities at 2 MV/cm for the films deposited at 15, 25, and 358C are 6.9 3 1029, 4.6 3 1029, and 3.6 3 1027 A/cm2, respectively. For the film deposited at 258C, the dielectric constant and the stress are minimal because of the high F content, low OH content, and low bond strain. The properties are also compared with those of fluorosilicate glass prepared by plasma-enhanced chemical vapor depo- sition. In addition to exhibiting a lower dielectric constant and much better resistance to moisture, the film prepared by tempera- ture-difference-based liquid-phase deposition also shows a comparable or better insulating property, revealing a reliable intermet- al dielectric with a low dielectric constant. -

A Mica/Nepheline Glass-Ceramic Prepared by Melting and Powder Metallurgy at Low Temperatures Wei, Wei; Yong, Liu; Yanni, Tan; Grover, Liam; Yu, Guo; Bowei, Liu
University of Birmingham A mica/nepheline glass-ceramic prepared by melting and powder metallurgy at low temperatures Wei, Wei; Yong, Liu; Yanni, Tan; Grover, Liam; Yu, Guo; Bowei, Liu DOI: 10.1016/j.mtcomm.2017.02.007 License: Creative Commons: Attribution-NonCommercial-NoDerivs (CC BY-NC-ND) Document Version Peer reviewed version Citation for published version (Harvard): Wei, W, Yong, L, Yanni, T, Grover, L, Yu, G & Bowei, L 2017, 'A mica/nepheline glass-ceramic prepared by melting and powder metallurgy at low temperatures', Materials Today Communications. https://doi.org/10.1016/j.mtcomm.2017.02.007 Link to publication on Research at Birmingham portal General rights Unless a licence is specified above, all rights (including copyright and moral rights) in this document are retained by the authors and/or the copyright holders. The express permission of the copyright holder must be obtained for any use of this material other than for purposes permitted by law. •Users may freely distribute the URL that is used to identify this publication. •Users may download and/or print one copy of the publication from the University of Birmingham research portal for the purpose of private study or non-commercial research. •User may use extracts from the document in line with the concept of ‘fair dealing’ under the Copyright, Designs and Patents Act 1988 (?) •Users may not further distribute the material nor use it for the purposes of commercial gain. Where a licence is displayed above, please note the terms and conditions of the licence govern your use of this document. When citing, please reference the published version. -
Near-Infrared Luminescence and Single-Mode Laser Emission from Nd3+ Doped Compound Glass and Glass Microsphere
ORIGINAL RESEARCH published: 25 September 2019 doi: 10.3389/fmats.2019.00237 Near-Infrared Luminescence and Single-Mode Laser Emission From Nd3+ Doped Compound Glass and Glass Microsphere Xin Wang 1, Haiyan Zhao 1, Angzhen Li 1, Ke Tian 1, Gilberto Brambilla 2 and Pengfei Wang 1,3* 1 Key Laboratory of In-fiber Integrated Optics of Ministry of Education, College of Science, Harbin Engineering University, Harbin, China, 2 Optoelectronics Research Centre, University of Southampton, Southampton, United Kingdom, 3 Key Laboratory of Optoelectronic Devices and Systems of Ministry of Education and Guangdong Province, College of Optoelectronic Engineering, Shenzhen University, Shenzhen, China In this letter, an Nd3+-doped compound fluorosilicate glass was successfully fabricated with the method of melt-quenching. Under the excitation of a 808 nm laser, enhanced near-infrared photoluminescence emission at the range from 1,065 to 1,140 nm was observed in the glass sample. To characterize its stability and resistance to environmental Edited by: effects, transmission spectra at the range of NIR-MIR were measured under different Guoping Dong, environments, including humidity and temperature. In addition, the obtained fluorosilicate South China University of Technology, China glass was also developed as a microsphere resonator by using CO2 laser heating Reviewed by: method. When the diameter of the microsphere was controlled at 61.5 µm, coupling Zhixu Jia, with a tapered fiber, single-multimode lasing in the wavelength range λ1,056–1,071 nm Jilin University, China Jayasankar Chalicheemalapalli Kulala, was achieved with a low lasing threshold of 1.5 mW. Compared to silica and phosphate Sri Venkateswara University, India glasses, this fluorosilicate glasses have lower phonon energy, which can reduce the Danping Chen, probability of non-radiative transitions and improve the photoluminescence efficiency. -
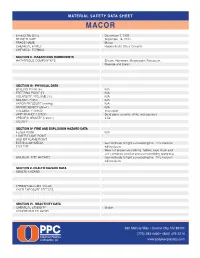
Macor Material Safety Data Sheet
MATERIAL SAFETY Data SHEET MACOR EFFECTIVE DATE December 1, 1993 REVISED DATE Sepember 16, 2011 TRADE NAME Macor CHEMICAL FAMILY Fluorosilicate Glass-Ceramic CHEMICAL FORMUA SECTION II - HAZARDOUS INGREDIENTS HAZARDOUS COMPONENTS Silicon, Aluminum, Magnesium, Potassium, Fluoride and Boron SECTION III - PHYSICAL DATA BOILING POINT (F) N/A FREEZING POINT (F) N/A VOLATILITY / VOLUME (%) N/A MELTING POINT N/A VAPOR PRESSURE (mmHg) N/A VAPOR DENSITY (Air=1) N/A SOLUBILITY IN H20 Insoluable APPEARANCE / ODOR Solid glass ceramic, white and odorless SPECIFIC GRAVITY (H20=1) 2.52 ACIDITY SECTION IV- FIRE AND EXPLOSION HAZARD DATA FLASH POINT N/A LOWER FLAME POINT HIGHER FLAME POINT EXTINGUISH MEDIA Use methods to fight surrounding fire. This material FOR FIRE will not burn. Wear full protective clothing, helmet, face mask and self-contained positive pressure breathing apparatus. UNUSUAL FIRE HAZARD Use methods to fight surrounding fire. This material will not burn. SECTION V- HEALTH HAZARD DATA HEALTH HAZARD THRESHOLD LIMIT VALUE OVER EXPOSURE EFFECTS SECTION VI - REACTIVITY DATA CHEMICAL STABILITY Stable CONDITIONS TO AVOID 550 Mallory Way • Carson City, NV 89701 (775) 283-4400 • (800) 475-2214 www.polymerplastics.com MATERIAL SAFETY Data SHEET MACOR SECTION VI - REACTIVITY DATA - CONTINUED INCOMPATIBLE MATERIALS Material will begin softeing at above 800° C, will proceed DECOMPOSITION PRODUCTS to a liquid and form irrtating and toxic gaseous metallic oxides at extremely high temperatures. HAZARDOUS POLYMERIZATIONS Will not occur POLYMERIZATION AVOID SECTION VII - SPILL OR LEAK PROCEDURE FOR SPILL Collect spill with a vacuum cleaner with a HEPA filter. Recycle or dispose off according to local regualtions. -

(12) United States Patent (10) Patent No.: US 6,541,400 B1 Tian Et Al
USOO6541400B1 (12) United States Patent (10) Patent No.: US 6,541,400 B1 Tian et al. (45) Date of Patent: Apr. 1, 2003 (54) PROCESS FOR CVD DEPOSITION OF T. Fukuda et al., Highly Reliable SiOF Film Formation by FLUORINATED SILICON GLASS LAYER ON ECR-CVD Using SiFH, Tech. Digest on 1996 Symp. On SEMCONDUCTOR WAFER VLSI Tech., p. 114-115 (1996). (75) Inventors: Jason L. Tian, Milpitas, CA (US); Shapiro et al., “CVD of Fluorosilicate Glass For ULSI Harald Te Nijenhuis, Fremont, CA Applications,” Elsevier Science S.A., 1995, pp. 503-507. (US) Laxman, "Low e Dielectrics: CVD Fluorinated Silicon Dioxides,” Semiconductor International, vol. 18, No. 5, (73) Assignee: Novellus Systems, Inc., San Jose, CA May 1995, pp. 71–74. (US) Singer, “Low K Dielectrics: The Search Continues,” Semi (*) Notice: Subject to any disclaimer, the term of this conductor International, vol. 19, No. 3, May 1996, pp. patent is extended or adjusted under 35 88-96. U.S.C. 154(b) by 0 days. T. Tamura et al., Ext. Abstracts 43th Spring Meeting; The Japan Soc. Appl. Phys. And Related Soc., p. 658 (1996) (21) Appl. No.: 09/501,347 (without English Translation). (22) Filed: Feb. 9, 2000 T. Fukuda et al., Highly Reliable SiOF Film Formation by (51) Int. Cl." ....................... H01L 21/31; H01L 21/469; ECR-CVD. Using SiFH, Tech. Digest 1996 symp. On VLSI H05H 1/02; H05H 1/24 Tech., pp. 114-115 (1996). (52) U.S. Cl. ....................... 438/784; 438/788; 427/574; 427/579 * cited by examiner (58) Field of Search ................................. 438/783, 784, 438/787, 788; 427/574, 578,579 Primary Examiner Olik Chaudhuri ASSistant Examiner Erik Kielin (56) References Cited (74) Attorney, Agent, or Firm-Skjerven Morrill LLP U.S. -

Glass Filler Material and Method of Production
Europäisches Patentamt *EP001547572A1* (19) European Patent Office Office européen des brevets (11) EP 1 547 572 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.7: A61K 6/027, C03C 13/00, 29.06.2005 Bulletin 2005/26 C03C 13/04, C03C 21/00, A61K 6/083 (21) Application number: 03029538.0 (22) Date of filing: 22.12.2003 (84) Designated Contracting States: (72) Inventors: AT BE BG CH CY CZ DE DK EE ES FI FR GB GR • Hoescheler, Stefan HU IE IT LI LU MC NL PT RO SE SI SK TR D-82211 Herrsching (DE) Designated Extension States: • Albrecht, Dirk AL LT LV MK D-82211 Herrsching (DE) • Stippschild, Andrea (71) Applicant: 3M ESPE AG D-86899 Landsberg (DE) 82229 Seefeld (DE) • Dede, Karsten D-86899 Landsberg (DE) (54) Glass filler material and method of production (57) The present invention relates to a glass filler and/or other lanthanidoxides, 0.05 - 4 mol% alkali metal material with an average particle size of 0.1 - 20 µm. It oxides (Na2O, Li2O, K2O, Rb2O, Cs2O), 0 - 25 mol% further relates to a method for producing a glass filler earth alkali metal oxides (MgO, CaO, SrO, BaO). material. The glass filler material comprises 65 - 99.95 The glass filler material shows a low concentration mol% silicon dioxide (SiO2), 0 - 15 mol% aluminum and/ of alkali ions and is used for composites with cationically or boron oxide (Al2O3,B2O3), 0 - 30 mol % zirconium curing properties and for dental composites and dental and/or titanium and/or hafnium oxide (ZrO2,TiO2, restoration materials. -

A Comprehensive Report on Ultrasonic Attenuation of Engineering Materials, Including Metals, Ceramics, Polymers, Fiber-Reinforced Composites, Wood, and Rocks
applied sciences Review A Comprehensive Report on Ultrasonic Attenuation of Engineering Materials, Including Metals, Ceramics, Polymers, Fiber-Reinforced Composites, Wood, and Rocks Kanji Ono Department of Materials Science and Engineering, University of California, Los Angeles (UCLA), Los Angeles, + http://www.ndt.net/?id=25454 CA 90095, USA; [email protected]; Tel.: 1-310-825-5534 Received: 24 February 2020; Accepted: 18 March 2020; Published: 25 March 2020 Abstract: In this paper, ultrasonic attenuation of engineering materials is evaluated comprehensively, covering metals, ceramics, polymers, fiber-reinforced composites, wood, and rocks. After verifying two reliable experimental methods, 336 measurements are conducted and their results are tabulated. Attenuation behavior is determined over broadband spectra, extending up to 15 MHz in low More info about this article: attenuating materials. The attenuation spectra are characterized in combination with four power law terms, with many showing linear frequency dependence, with or without Rayleigh scattering. Dislocation damping effects are re-evaluated and a new mechanism is proposed to explain some of the linear frequency dependencies. Additionally, quadratic and cubic dependencies due to Datta–Kinra scattering and Biwa scattering, respectively, are used for some materials to construct model relations. From many test results, some previously hidden behaviors emerged upon data evaluation. Effects of cold working, tempering, and annealing are complex and sometimes contradictory. Comparison to available literature was attempted for some, but most often prior data were unavailable. This collection of new attenuation data will be of value in materials selection and in designing structural health monitoring and non-destructive inspection protocols. Keywords: ultrasonic attenuation; damping factor; metals; ceramics; polymers; fiber-reinforced composites; wood; rocks; dislocation damping; Mason–McSkimin relation; Rayleigh scattering; Datta–Kinra scattering; Biwa scattering 1. -

Pdf/23/3/1/1819240/1559-2863-23-3-1.Pdf by Guest on 30 September 2021 DENTISTRY
OPE TIVE Downloaded from http://meridian.allenpress.com/operative-dentistry/article-pdf/23/3/1/1819240/1559-2863-23-3-1.pdf by guest on 30 September 2021 DENTISTRY march-april 1998 • volume 23 • number 3 • 105-160 (ISSN 0361-7734) OPERATIVE DENTISTRY MAY-JUNE 1998 VOLUME 23 NUMBER 3 • 105- 160 Aim and Scope Editorial Office Operative Dentistry publishes articles that advance the University of Washington, OPERATIVE DENTISTRY, practice ofoperative dentistry. The scope of the journal Box 357457, Seattle, WA 98195-7457 includes conservation and restoration of teeth; the Telephone: (206) 543-5913, FAX (206) 543-7783 scientific foundation of operative dental therapy; URL: http:!/weber . u. washington . edu/~opdent/ dental materials; dental education; and the social, political, and economic aspects of dental practice. Subscription Manager: Judy Valela Downloaded from http://meridian.allenpress.com/operative-dentistry/article-pdf/23/3/1/1819240/1559-2863-23-3-1.pdf by guest on 30 September 2021 Review papers, book reviews, letters, and classified ads also are published. Editorial Staff Editor: Richard B McCoy Editorial Assistant: Darlyne J Bales OPERATIVE DENTISTRY (ISSN 0361-7734) is pub lished bimonthly for $55.00 per year in the US Editorial Associate: Kate Flynn Connolly and Canada (other countries $70.00 per year) by University of Washington, Operative Dentistry, Associate Editor: Michael A Cochran Health Sciences Bldg, Rm D-775, Seattle, WA98195- Managing Editor: J Martin Anderson 7457. Periodicals postage paid at Seattle, WA, and at additional mailing offices. POSTMASTER: Send Assistant Managing Editors: Paul Y Hasegawa and address changes to: University of Washington, Ralph J Werner OPERATIVE DENTISTRY, Box 357457, Seattle, WA 98195-7457. -

Ebook < Glass Compositions ~ Read
WELDL2TJPF ~ Glass compositions // Kindle Glass compositions By Source Reference Series Books LLC Jun 2011, 2011. Taschenbuch. Book Condition: Neu. 246x189x5 mm. Neuware - Source: Wikipedia. Pages: 45. Chapters: Egyptian faience, Lead glass, Tin-glazing, Vitreous enamel, Sodium silicate, Glass-to-metal seal, Bioglass, Salt glaze pottery, Borosilicate glass, Fused quartz, Phosphorus pentoxide, Uranium glass, Ground granulated blast furnace slag, Germanium dioxide, Soda-lime glass, Ceramic glaze, Boron trioxide, Low dispersion glass, Bioactive glass, Photochromic lens, Dichroic glass, Phosphate glass, Wood's glass, Sodium hexametaphosphate, Potassium silicate, Crown glass, Cranberry glass, Milk glass, Reagent bottle, Glass- ceramic-to-metal seals, Amorphous carbonia, Opaline glass, Flint glass, Scotchlite, Fluorophosphate glass, Cobalt glass, Glass with embedded metal and sulfides, Underglaze, Aluminosilicate, Borophosphosilicate glass, Vitrite, Ultra low expansion glass, Fluorosilicate glass, Leaded glass, Tellurite glass, Soluble glass. Excerpt: Egyptian faience is a non-clay based ceramic displaying surface vitrification which creates a bright lustre of various blue-green colours. Having not been made from clay it is often not classed as pottery. It is called 'Egyptian faience' to distinguish it from faience, the tin glazed pottery associated with Faenza in northern Italy. Egyptian faience, both locally produced and exported from Egypt, occurs widely in the ancient world, and is well known from Mesopotamia, the Mediterranean and in northern Europe as far away... READ ONLINE [ 2.27 MB ] Reviews This is the greatest pdf i actually have go through right up until now. It is actually packed with knowledge and wisdom I found out this book from my dad and i advised this publication to find out. -

Annual Report 2017
The Key Laboratory of Weak Light Nonlinear Photonics, Ministry of Education Annual Report 2017 南开大学弱光非线性光子学 教育部重点实验室 Annual Report 2017 The Key Laboratory of Weak Light Nonlinear Photonics, Ministry of Education 南开大学弱光非线性光子学 教育部重点实验室 弱光非线性光子学教育部重点实验室学术年会在泰达应用物理研究院召开。 (2017.1.7) 弱光非线性光子学教育部重点实验室在泰达应用物理研究院召开 2017 年学术委员会会 议暨 2016 年度考核会议。 (2017.3.19) 清华大学物理系吴扬博士访问重点实验室,并为师生做题为“Topological quantum phases in low-dimensional materials”的学术报告。 (2017.3.30) Nature communications 编辑 Nina Meinzer 访问重点实验室,并为师生作题为“Nature Communications: Open Access all areas”的学术报告。 (2017.4.26) 弱光非线性光子学教育部重点实验室外聘专家、乌克兰国家科学院 Andrey Ilyin 研究员来 重点实验室进行研究工作,并指导研究生的科研实验工作。 (2017.6.21-7.29) 弱光非线性光子学教育部重点实验室外聘专家、美国阿拉巴马农工大学物理系 Nickolai V.Kukhtarev 教授来重点实验室进行科研和指导研究生工作。 (2017.7.9-8.9) 弱光非线性光子学教育部重点实验室外聘专家、奥地利维也纳大学 Romano Rupp 教授 来重点实验室进行科研和指导研究生工作,并为研究生授课。(2017.7.6-9.30) 物理科学学院和泰达应用物理研究院于 2017 年 7 月 4 日至 7 月 7 日举办“2017 年南开 大学‘我爱物理’优秀大学生夏令营”。7 月 6 日,近 70 名夏令营学生参观弱光非线性 光子学教育部重点实验室,并进行师生交流等。 (2017.7.6) 为增强实验室安全意识,吴强教授和潘雷霆副教授为即将进入重点实验室进行科研实验 的学生分别做光学、电学、生物和化学等方面的实验室安全知识讲座,并安排学生进行 相关实验室安全知识学习。 (2017.7.12) 奥地利维也纳大学物理系研究生 Dominik Lucas WIND 和 Mathias FLEISCH 作为留学生来 重点实验室进行为期五个月的国际合作项目研究。 (2017.8.30-2018.1.31) 陈树琪教授课题组接收平顶山学院电气与机械工程学院教师万明理来重点实验室进行 为期一年的访问学习。 (2017.9-2018.6) 为培养学术交流能力,拓展学术视野,促进学术交流,泰达应用物理研究院学生会举办 了第七届“南开大学光学与光子学前沿科学论坛”。 (2017.9.23) 教育部重点实验室特聘教授,卢布雅尔娜大学& 斯特藩研究所教授 Irena Drevenšek-Olenik 来重点实验室从事教学和科研工作,并为师生作题为“Tunable Surface Properties of Soft Magnetoactive Elastomers”的学术报告。 (2017.9.26) 国家千人计划入选者、重点实验室陈志刚教授召开国家重点研发计划“量子调控与量子 信息”重点专项“具有拓扑特性的空间光场产生、调控及与微结构相互作用”项目启动 会。 (2017.9.30) -

A Mica/Nepheline Glass-Ceramic Prepared by Melting and Powder Metallurgy at Low Temperatures Wei, Wei; Yong, Liu; Yanni, Tan; Grover, Liam; Yu, Guo; Bowei, Liu
University of Birmingham A mica/nepheline glass-ceramic prepared by melting and powder metallurgy at low temperatures Wei, Wei; Yong, Liu; Yanni, Tan; Grover, Liam; Yu, Guo; Bowei, Liu DOI: 10.1016/j.mtcomm.2017.02.007 License: Creative Commons: Attribution-NonCommercial-NoDerivs (CC BY-NC-ND) Document Version Peer reviewed version Citation for published version (Harvard): Wei, W, Yong, L, Yanni, T, Grover, L, Yu, G & Bowei, L 2017, 'A mica/nepheline glass-ceramic prepared by melting and powder metallurgy at low temperatures', Materials Today Communications. https://doi.org/10.1016/j.mtcomm.2017.02.007 Link to publication on Research at Birmingham portal General rights Unless a licence is specified above, all rights (including copyright and moral rights) in this document are retained by the authors and/or the copyright holders. The express permission of the copyright holder must be obtained for any use of this material other than for purposes permitted by law. •Users may freely distribute the URL that is used to identify this publication. •Users may download and/or print one copy of the publication from the University of Birmingham research portal for the purpose of private study or non-commercial research. •User may use extracts from the document in line with the concept of ‘fair dealing’ under the Copyright, Designs and Patents Act 1988 (?) •Users may not further distribute the material nor use it for the purposes of commercial gain. Where a licence is displayed above, please note the terms and conditions of the licence govern your use of this document. When citing, please reference the published version.