A New Parent Guide
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nursing Strike
Nursing Strike When a baby who has been nursing happily for some length of time suddenly refuses to latch and feed at the breast, we call it a nursing strike. It can be very upsetting for both a mother and her baby. Nursing strikes happen for many reasons, and we often do not know exactly why. Often it seems as though a baby is trying to communicate Community some form of stress. It is unlikely that your baby is ready to wean, especially if your Breastfeeding baby is less than a year old. Center A nursing strike can last several hours, or several days. While your baby is refusing to 5930 S. 58th Street feed at your breast, use a high-quality pump and remove milk just as often as your (in the Trade Center) Lincoln, NE 68516 baby was nursing. If your breasts get very full and firm, your baby may notice the (402) 423-6402 difference and it may be harder for baby to latch. You may also risk developing a 10818 Elm Street plugged duct. Rockbrook Village Omaha, NE 68144 (402) 502-0617 The following is a list of common reasons that babies refuse the breast, For additional adapted from La Leche League International information: information: www • You changed your deodorant, soap, perfume, lotion, etc. and you smell “different” to your baby. • You have been under stress (such as having extra company, returning to work, traveling, moving, or dealing with a family crisis). • Your baby or toddler has an illness or injury that makes nursing uncomfortable (an ear infection, a stuffy nose, thrush, a cut in the mouth, or sore gums from teething). -

The Lactating Angel Or Activist? Public Breatsfeeding As Symbolic Speech
Michigan Journal of Gender & Law Volume 15 Issue 1 2008 The Lactating Angel or Activist? Public Breatsfeeding as Symbolic Speech Elizabeth Hildebrand Matherne Law Offices of Robert Wesley, Public Defender, Ninth Judicial Circuit of Florida Follow this and additional works at: https://repository.law.umich.edu/mjgl Part of the First Amendment Commons, and the Law and Gender Commons Recommended Citation Elizabeth H. Matherne, The Lactating Angel or Activist? Public Breatsfeeding as Symbolic Speech, 15 MICH. J. GENDER & L. 121 (2008). Available at: https://repository.law.umich.edu/mjgl/vol15/iss1/3 This Article is brought to you for free and open access by the Journals at University of Michigan Law School Scholarship Repository. It has been accepted for inclusion in Michigan Journal of Gender & Law by an authorized editor of University of Michigan Law School Scholarship Repository. For more information, please contact [email protected]. THE LACTATING ANGEL OR ACTIVIST? PUBLIC BREASTFEEDING AS SYMBOLIC SPEECHt Elizabeth Bildebrand c.atherne* INTRODUCTION- 121 1. CULTURAL CONTEXT-THE BENEFITS OF BREASTFEEDING • 123 A. Breastfeeding Benefits the Infant • 124 B. Breastfeeding Benefits the Mother • 125 C. Breastfeeding Benefits Society . 126 II. CULTURAL CONTEXT-SOCIAL STIGMA • 127 III. SOCIETY'S MESSAGE-WOMEN BELONG IN THE HOME . 128 IV. No VIABLE LEGAL RECOURSE • 131 V. HISTORY OF FIRST AMENDMENT AND SYMBOLIC SPEECH • 134 VI. SYMBOLIC SPEECH UNDER THE SPENCE TEST • 136 VII. BREASTFEEDING IS SYMBOLIC SPEECH • 139 CONCLUSION . 142 INTRODUCTION "[T]he history of women's visibility is predominately the history of women's objectification and oppression. "' t The term "lactating angel" borrowed with the author's permission from the article of St. -

General Instructions for Infant and Child Care
Name _______________________________________________ Birth Date ____________________________________________ GENERAL INSTRUCTIONS FOR INFANT AND CHILD CARE GUIDELINES FOR HEALTH EVALUATION VISITS Richmond Pediatrics Pediatric & Adolescent Medicine . for over 50 years 357 N.W. Richmond Beach Road Shoreline, Washington 98177 (206) 546-2421 (206) 546-8436 – Fax www.Richmond-Pediatrics.com Age Immunization Date Given Immunizations >9 Years Old Birth Hepatitis B Immunization Date Given Hepatitis B MCV4 (Meningitis) #1 DtaP MCV4 (Meningitis) #2 IPV (Polio) 2 Months TdaP Hib (Meningitis) HPV #1 PCV13 (Pneumonia) Rotavirus HPV #2 DtaP HPV #3 IPV (Polio) 4 Months Hib (Meningitis) We also recommend a yearly influenza immunization. PCV13 (Pneumonia) Rotavirus Hepatitis B DtaP IPV (Polio) 6 Months Hib (Meningitis) PCV13 (Pneumonia) Rotavirus MMR VZV (Chickenpox) DtaP 12 -18 Hib (Meningitis) Months PCV13 (Pneumonia) Hepatitis A #1 Hepatitis A #2 18mos-4yrs PCV13 booster DtaP IPV 5 Years MMR VZV (Chickenpox) Influenza #1 6mos-5 yrs Influenza #2 TABLE OF CONTENTS Infant Care Page Breast Feeding ..............................................................6 Diarrhea .......................................................................20 Formula .........................................................................8 Dehydration .................................................................20 Feeding Schedule .........................................................9 Fever ...........................................................................22 -
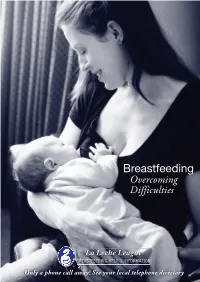
Overcoming Difficulties (PDF)
Breastfeeding Overcoming Difficulties ® Only a phone call away! See your local telephone directory Breastfeeding is a gift only you can give to your baby. A healthy full-term baby is likely to know instinctively what to do at the breast. For many mothers and babies breastfeeding goes well right from the start, for others it can take a little longer to learn. Common problems can be minimized or avoided entirely if a mother has accurate and consistent breastfeeding information and support. “Breastfeeding is a long term commitment. In order to succeed, a mother needs the encouragement and companionship of other mothers. La Leche League succeeded in the beginning and continues to work well because it meets the dual need for sound practical information and loving support. Babies don’t change and neither do mothers, though the circumstances in which they find themselves differ from one generation to the next.” Mary Ann Cahill, Founder LLL Sore Nipples Many mothers experience some nipple tenderness at the beginning of a feed during the first two to three days of breastfeeding, however, breastfeeding should not hurt. If you have continued discomfort or pain while breastfeeding or have discomfort or pain between breastfeeds, some adjustment or treatment may be needed. Research shows that good positioning of the baby at the breast will help prevent and heal sore nipples. Positioning Baby at the Breast There are a number of ways to hold your baby while breastfeeding. Getting your baby started at the breast smoothly and easily will soon become second nature to you. Nursing a baby at the breast is actually much less involved than any description of the process. -

Breastfeeding Your Baby: the First Few Weeks
healthy living Breastfeeding Your Baby: The First Few Weeks Allow your baby to nurse for as long as • Make sure that your baby’s head is he or she wants. If your baby is still at the level of your breast and that hungry after finishing the first breast, his or her lips are lined up with your offer the second breast. Some newborn nipple. Your baby’s face, chest, and babies may nurse for about 10 to 15 knees should be turned toward you minutes on each breast. Others may so that the two of you are tummy nurse for 15 to 20 minutes on only to tummy. one side per feeding. You should wake • Tickle the baby’s lower lip with your your baby up to eat if more than 3 nipple and wait for the baby to hours have passed since the last feed- make a wide “O” with his or her ing. Feedings should be timed from mouth before putting the baby to the beginning of one to the beginning your breast. of the next. • Quickly bring your baby towards Unless your baby’s doctor tells you to, you, centering your nipple in the don’t offer any supplements such as baby’s mouth. water or formula. • Make sure your baby is taking the nipple and a good portion of the How do I help my baby latch areola in his or her mouth. reastfeeding is the natural way onto my breast? • Make sure your baby’s lower lip is Bto provide all the nutrition your Find a comfortable chair to sit in. -

Preparing to Breastfeed Ome Women Wonder What They Need to Do • Room for Expansion
Preparing to Breastfeed ome women wonder what they need to do • Room for expansion. Your breasts may go up a full cup during pregnancy to prepare for breastfeeding. size when your milk comes in. Actually, your body knows what to do. Lactation • Breathable fabrics are best while breastfeeding. S(milk production) naturally follows pregnancy. The • Consider buying only 1 or 2 bras during the final hormones produced during pregnancy prepare your weeks of pregnancy and waiting until a couple of breasts to make milk once your baby is born. The best weeks postpartum to add more to your wardrobe. preparation, and what most women need in order (A gift certificate for a new bra makes a great shower to breastfeed effectively, is accurate information and gift.) Many mothers-to-be like to know that their someone to provide support and encouragement. breast size will settle into a moderately larger size after about three months. During Pregnancy At one time a great deal of emphasis was placed on Concerns About Nipple Size or Shape preparing your nipples during pregnancy. However, it is In order for the baby to suck effectively, he needs to now recognized that correct positioning and latch-on draw your nipple far back into his mouth. Babies can of the baby in the early days is the best prevention for breastfeed effectively with a large variety of nipple nipple soreness. So what shapes. The nipple is only a part of the breast called the should you expect before nipple-areola complex. The softness and stretchiness the baby is born? of the tissue just behind the nipple is actually more • Your breasts will likely important than the nipple shape. -

Why Baby Cries
Why Does My Baby Cry? All babies cry, and some cry a lot. La Leche League Leader, lactation consultant, midwife or nurse) if you are worried. When it’s your baby who is crying a lot, it can be very frustrating and upsetting for you, too. You try burping him, After day three or four: rocking him - and he’s still wailing. What’s wrong? You At this point, the amount of milk in your breasts will might be worried about making enough milk to fill him. increase significantly. Your baby may have trouble latching Or think that your milk is not good enough. Or maybe you on to your fuller breasts, and that might cause more crying. are worried that something you are eating is upsetting his Try to express a little milk to make your breasts tummy through your milk. softer and help him latch on. If that doesn’t work, ask for some help. You’re not alone in these concerns. Many mothers worry about these things. But most of the time, Your baby lost weight in the first few days your baby’s crying has nothing to do with the (as he got rid of the dark-coloured poop quality or amount of milk in your breasts. called meconium that was previously in his gut) but now he will start gaining. The truth is that there are many reasons babies Between 5 and 8 ounces or 140-250 grams cry. Crying is one way your baby communicates each week is typical. That means he is with you, but at first it can be a challenge to getting plenty of milk - one worry you figure out what he’s trying to tell you. -

The New Family
The New Family Your Child’s Early Months Key Points for New Families If you need more information about any of these topics, please tell your nurse before leaving the hospital. In the Hospital: Things You Should Know Before You Leave: Things You Should Do Right after delivery: ☐ Fill out paperwork for your baby’s birth certificate and social security card ...... page c ☐ Mom’s recovery and comfort care ......page 4 ☐ Make sure you have a rear-facing car seat for ☐ Hospital security ...............................page 4 your baby ........................................page 24 ☐ Early breastfeeding ..........................page 29 After You Go Home ☐ Skin-to-skin contact ........................page 29 ☐ Get help if you have trouble Safety: breastfeeding ..................................... page a ☐ Signs of jaundice ............................ page 13 ☐ Schedule your baby’s first doctor visit ........................................ page a ☐ Shaken Baby Syndrome ...................page 23 ☐ Know when it’s safe to resume sex .....page 5 ☐ Safe sleep .........................................page 24 ☐ Choose a method of birth control .....page 5 ☐ Newborn safety ...............................page 24 ☐ Know when to call: Baby-care skills: Your doctor ..................................page 6 Your baby’s doctor ......................page 25 ☐ Circumcision care ...........................page 16 ☐ Watch for signs of depression ............page 8 ☐ Cord care ........................................page 18 ☐ Schedule a postpartum visit ☐ Bathing -

Breastfeeding in Custody Proceedings: a Modern-Day Manifestation of Liberal and Conservative Family Traditions
BREASTFEEDING IN CUSTODY PROCEEDINGS: A MODERN- DAY MANIFESTATION OF LIBERAL AND CONSERVATIVE FAMILY TRADITIONS Kate Baxter-Kauf In the past decade, popular and medical opinions have coa- lesced around the conclusion that breastfeeding an infant for at least the first year of life,2 preferably to the exclusion of infant formula or * Law clerk to Justices Page, Meyer. and Dietzen, Minnesota Supreme Court. J.D., magna cum laude, University of Minnesota Law School, B.A., magna cum laude, Macalester Col- lege. Special thanks to Professor Jill Hasday for her helpful comments on earlier drafts of this article, and to Baxter and Kiernan, without whom this article would not be possible. 1 There appears to be no standardized spelling for the act of breastfeeding, at least in legal opinions. Various court decisions use "breast feeding." "breastfeeding" or "breast-feeding." Additionally, medical experts do not seem to differentiate between the giving of breast milk to an infant via the breast or via pumping expressed milk. This Comment will use the term "breastfeeding," in accordance with the spelling chosen by La Leche League International ("LLLI"), and uses it to refer to both traditional nursing and the feeding of expressed breast milk. See, e.g. LA LECHE LEAGUE INTERNATIONAL, All About La Leche League, http://www.lli.org/ab.html?m=1 (last updated Apr. 26, 2010). This Comment also uses the terms "nursing" and "breastfeeding" largely interchangeably, though "nursing" seems to be more typically used to describe the act of feeding an infant from the breast itself. For a dis- cussion of the potential inappropriateness of using the terms interchangeably in the legal context, see infra note 87 and accompanying text. -

La Leche League International Applauds American Academy of Pediatric’S Updated Infant Sleep Policy
For Immediate Release Media Inquiries: Diana West, Director of Media Relations La Leche League International [email protected] | 908-400-1820 llli.org/about_us/press/press.html LA LECHE LEAGUE INTERNATIONAL APPLAUDS AMERICAN ACADEMY OF PEDIATRIC’S UPDATED INFANT SLEEP POLICY RALEIGH, North Carolina (January 10, 2017) ― The American Academy of Pediatrics (AAP) and La Leche League International (LLLI) both have long histories of providing research- based information to breastfeeding mothers and their families ― the AAP through its guidelines and recommendations, and LLLI through mother-to-mother support and publications. The AAP’s revised policy statement, “SIDS and Other Sleep-Related Infant Deaths: Updated 2016 Recommendations for a Safe Infant Sleeping Environment,” is its latest update on safe infant sleep, reinforcing many earlier recommendations, adjusting others in light of new information, and bringing the two organizations into closer alignment. The 2016 AAP update renews its emphasis on keeping the baby in the parents’ room at night for at least the first six months. LLLI agrees that it is an important reminder to new parents that even a carefully-prepared nursery poses a risk to young babies who rely on responsive adults for their safety and wellbeing. The revised policy states more clearly that their recommendation against bedsharing is for infants younger than four months, which is an important clarification often missed by parents and healthcare providers. LLLI particularly applauds the AAP for recognizing the need for a safe place for drowsy nighttime breastfeeding sessions since hormones released during breastfeeding can make a mother sleepy: “Evidence suggests that it is less hazardous to fall asleep with the infant in the adult bed than on a sofa or armchair, should the parent fall asleep.” The new AAP guideline protects both babies and breastfeeding. -

Feeding Your Baby
_~Äó=eÉäé cÉÉÇáåÖ=~åÇ=fããìåáòáåÖ=vçìê=_~Äó cáêëí=bÇáíáçåW=NVTR cáêëí=oÉîáëáçåW=NVUM pÉÅçåÇ=oÉîáëáçåW=NVUQ qÜáêÇ=oÉîáëáçåW=NVVM cçìêíÜ=oÉîáëáçåW=NVVR cáÑíÜ=oÉîáëáçåW=NVVU páñíÜ=oÉîáëáçåW=OMMM pÉîÉåíÜ=oÉîáëáçåW=OMMP báÖÜíÜ=oÉîáëáçåW=OMMT mêÉé~êÉÇ=ÄóW= mêáåÅÉ=bÇï~êÇ=fëä~åÇ=aÉé~êíãÉåí=çÑ=eÉ~äíÜ _~Äó=eÉäé=oÉëçìêÅÉë `çããìåáíó `çããìåáíó=aáÉíáíá~å mìÄäáÅ=eÉ~äíÜ=kìêëÉ qáÖåáëÜ UUOJTPSS ^äÄÉêíçå URVJUTOM lÛiÉ~êó URVJUTOP URVJUTOM=EUTONF tÉääáåÖíçå URQJTORV pìããÉêëáÇÉ UUUJUNRS=EUNRTF UUUJUNSM hÉåëáåÖíçå UPSJPUSP `Ü~êäçííÉíçïå PSUJRPRT=ERPRPF=ERMTNF PSUJQRPM jçåí~ÖìÉ UPUJMTNV UPUJMTSO pçìêáë SUTJTMRN=ETMRRF SUTJTMQV iÉååçñ=fëä~åÇ=eÉ~äíÜ=`ÉåíêÉ UPNJOTNN ^ÄÉÖïÉáí=eÉ~äíÜ=`ÉåíêÉI=pÅçíÅÜÑçêí STSJPMMT=EORORF i~iÉÅÜÉ=iÉ~ÖìÉ qÜÉ=i~iÉÅÜÉ=iÉ~ÖìÉ=áë=~=Öêçìé=çÑ=ãçíÜÉêë=ïÜç=Ü~îÉ=ÄêÉ~ëíÑÉÇ=íÜÉáê=Ä~ÄáÉëK=qÜÉó=çÑÑÉê=ÜÉäé=~åÇ=~ÇîáÅÉ íç=íÜçëÉ=ïÜç=éä~å=íç=ÄêÉ~ëíÑÉÉÇ=çê=~êÉ=ÅìêêÉåíäó=ÄêÉ~ëíÑÉÉÇáåÖK=få=~ÇÇáíáçåI=íÜÉáê=ãçåíÜäó=ãÉÉíáåÖë éêçîáÇÉ=áåÑçêã~íáçå=~åÇ=ëìééçêí=íç=ãçíÜÉêëK=cÉÉä=ÑêÉÉ=íç=Åçåí~Åí=~=Öêçìé=äÉ~ÇÉê=áå=óçìê=~êÉ~=Ñêçã=íÜçëÉ äáëíÉÇ=ÄÉäçïW `Ü~êäçííÉíçïå `Üêáë=lêíÉåÄìêÖÉê STRJOOPV `çJäÉ~ÇÉê jÉä~åáÉ=t~äëÜJcê~ëÉê RSVJNSMQ `çããìåáíó i~Åí~íáçå=`çåëìäí~åíë eçëéáí~äë ^äÄÉêíçå URPJOPPM lÛiÉ~êó oáí~=^êëÉå~ìäíI=URVJUTOP URVJUTOM qóåÉ=s~ääÉó = UPNJTVMM pìããÉêëáÇÉ _~êÄ=máåÉ~ìI=UUUJUNSM QPOJORMM pìããÉêëáÇÉ açåå~=t~äëÜI=QPOJORMM QPSJVNPNI=Éñí=NPN Éñí=OPQ=çê=QPSJVNPNI=Éñí=OPQ= `Ü~êäçííÉíçïå qÜÉêÉë~=qê~áåçêI=PSUJQRPN oçëÉã~êó=aê~âÉI= UVQJOOST=EOOSUF UVOJSSTTEÜF UVQJOMMQ=EaáÉíáíá~åF UVQJOQQM=EmÉÇë=`äáåáÅF j~êáäóå=kçêíçåI UVQJRNRN=EÜFI=UVOJUTQQEïF jçåí~ÖìÉ UPUJMTTT pçìêáë SUTJTNRM -
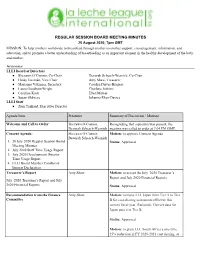
Regular Session Board Meeting Minutes
REGULAR SESSION BOARD MEETING MINUTES 25 August 2020, 7pm GMT MISSION: To help mothers worldwide to breastfeed through mother-to-mother support, encouragement, information, and education, and to promote a better understanding of breastfeeding as an important element in the healthy development of the baby and mother. ATTENDEES LLLI Board of Directors ● Shevawn O’Connor, Co-Chair Devorah Schesch-Wernick, Co-Chair ● Heidy Guzmán, Vice Chair Amy Shaw, Treasurer ● Marianne Vakiener, Secretary Carolyn Driver-Burgess ● Laura Goodwin-Wright Charlene Jenkins ● Caroline Kren Ellen Mateer ● Susan Oldrieve Johanna Rhys-Davies LLLI Staff ● Zion Tankard, Executive Director Agenda Item Presenter Summary of Discussion / Motions Welcome and Call to Order Shevawn O-Connor, Recognizing that a quorum was present, the Devorah Schesch-Wernick meeting was called to order at 7:04 PM GMT. Consent Agenda: Shevawn O-Connor, Motion: to approve Consent Agenda Devorah Schesch-Wernick 1. 28 July 2020 Regular Session Board Status: Approved Meeting Minutes 2. July 2020 Staff Time Usage Report 3. July 2020 Development Director Time Usage Report 4. LLLI Board Member Conflict of Interest Declaration Treasurer’s Report Amy Shaw Motion: to accept the July 2020 Treasurer’s Report and July 2020 Financial Reports July 2020 Treasurer’s Report and July 2020 Financial Reports Status: Approved Recommendation from the Finance Amy Shaw Motion: to move LLL Japan from Tier A to Tier Committee B for cost-sharing assessment effective this current fiscal year. Rationale: Current data for Japan puts it in Tier B. Status: Approved Motion: to grant LLL South Africa a one-time 25% reduction in FY 2020-2021 cost sharing, as requested by the IAN.