What Works – the African Regional Health Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

North Minneapolis—A Welcoming Home for Business Welcome
GrowNorth! North Minneapolis—A welcoming home for business Welcome If you have any questions or ideas, please contact your personal business development consultant at the City of Minneapolis, Casey Dzieweczynski 612-673-5070 On behalf of the City of Minneapolis, we would like to thank you for considering North Minneapolis as the new location for your business. Today is a great time to invest, and here’s why: • North Minneapolis is conveniently located near downtown, accessible from the entire metro and has great freeway access to Interstates 94 and 394. The area is also served by Olson Highway and Highway 100 with a connection to South Minneapolis via the Van White Memorial Boulevard. • The City’s economic development team can help find the right location for your busi- ness through its site assistance support. Available real estate includes significant areas of industrially zoned land, well-served by freeways and freight rail. • The City offers several business financing programs, ranging from $1,000 to $10 million and development grants to assist business owners in acquiring property, purchasing equipment and making building improvements. • The City’s employment and training program team can assist with workforce recruit- ment and training programs so your staff is knowledgeable and productive the minute they are hired. • The Minneapolis-coordinated development review will help you successfully navigate the regulatory process, which includes Planning/Zoning, Building Plan Review, Permit- ting and Licensing, and other regulatory review agencies. No one knows Minneapolis the way we do. The Department of Community Planning and Economic Development is ready to support you with all your business needs—from finance to site location, to customized training to fit your employment needs—and is here to help you every step of the way. -

G8 Research Group May 30, 2010
Join the Global Conversation Policy Brief The Group of Eight G8 Research Group May 30, 2010 The 36th G8 summit, taking place in Muskoka, Canada, on June 25-26, 2010, will strengthen governance both within itself and in its relationship with the new G20. At Muskoka, the world’s most powerful leaders will have frank, face-to-face intimate discussions, backed by deeply shared values, to deal with critical global issues in the domains of development and security. For the first time, the G8 summit will occur in tandem with the summit of the G20 in Toronto on June 26-27, the first since the G20’s proclamation at Pittsburgh in September 2009 that it is the world’s premier permanent forum for international economic cooperation. In March 2010, Canadian prime minister Stephen Harper stated that “the G8 remains the principal forum for advancing our common agenda of peace and security, as well as democracy and development. This is critical work. Indeed, progress made on economic issues at the G20 table risks being undone if the world’s pressing security and development concerns are not addressed with equal vigour.” Today’s G8 first met in 1975 as the Group of Six, with the leaders of France, Germany, Italy, Japan, the United Kingdom and the United States. Its initial mission was to govern economic and related issues, based on their shared values and responsibilities to protect open democracy, individual liberty and social advance around the world. In 1976, at the urging of Henry Kissinger, Canada was added. Russia became a full member in 1998. -

Evidence-Based Allocation in Global Health: Lessons Learned for Germany
A Service of Leibniz-Informationszentrum econstor Wirtschaft Leibniz Information Centre Make Your Publications Visible. zbw for Economics Minasyan, Anna Working Paper Evidence-based allocation in global health: lessons learned for Germany Discussion Paper, No. 4/2018 Provided in Cooperation with: German Development Institute / Deutsches Institut für Entwicklungspolitik (DIE), Bonn Suggested Citation: Minasyan, Anna (2018) : Evidence-based allocation in global health: lessons learned for Germany, Discussion Paper, No. 4/2018, ISBN 978-3-96021-060-3, Deutsches Institut für Entwicklungspolitik (DIE), Bonn, http://dx.doi.org/10.23661/dp4.2018 This Version is available at: http://hdl.handle.net/10419/199524 Standard-Nutzungsbedingungen: Terms of use: Die Dokumente auf EconStor dürfen zu eigenen wissenschaftlichen Documents in EconStor may be saved and copied for your Zwecken und zum Privatgebrauch gespeichert und kopiert werden. personal and scholarly purposes. Sie dürfen die Dokumente nicht für öffentliche oder kommerzielle You are not to copy documents for public or commercial Zwecke vervielfältigen, öffentlich ausstellen, öffentlich zugänglich purposes, to exhibit the documents publicly, to make them machen, vertreiben oder anderweitig nutzen. publicly available on the internet, or to distribute or otherwise use the documents in public. Sofern die Verfasser die Dokumente unter Open-Content-Lizenzen (insbesondere CC-Lizenzen) zur Verfügung gestellt haben sollten, If the documents have been made available under an Open gelten abweichend von -

G8 Research Group June 11, 2010
Join the Global Conversation Policy Brief The Group of Eight G8 Research Group June 11, 2010 The 36th G8 summit, taking place in Muskoka, Canada, on June 25-26, 2010, will strengthen governance both within itself and in its relationship with the new G20. At Muskoka, the world’s most powerful leaders will have frank, face-to-face intimate discussions, backed by deeply shared values, to deal with critical global issues in the domains of development and security. For the first time, the G8 summit will occur in tandem with the summit of the G20 in Toronto on June 26-27. In March 2010, Canadian prime minister Stephen Harper stated that “the G8 remains the principal forum for advancing our common agenda of peace and security, as well as democracy and development. This is critical work. Indeed, progress made on economic issues at the G20 table risks being undone if the world’s pressing security and development concerns are not addressed with equal vigour.” Today’s G8 first met in 1975 as the Group of Six, with the leaders of France, Germany, Italy, Japan, the United Kingdom and the United States. Its initial mission was to govern economic and related issues, based on their shared values and responsibilities to protect open democracy, individual liberty and social advance around the world. In 1976, at the urging of Henry Kissinger, Canada was added. Russia became a full member in 1998. Over the next three decades, the G8’s agenda grew to include a wide range of issues, including energy, trade, food security, health, water and sanitation, and security in old and new forms. -

Working to Overcome the Global Impact of Neglected Tropical Diseases Annexe I
Working to Overcome the Global Impact of Neglected Tropical Diseases Annexe I Working to overcome the global impact of neglected tropical diseases First WHO report on neglected tropical diseases WHO Library Cataloguing-in-Publication Data First WHO report on neglected tropical diseases: working to overcome the global impact of neglected tropical diseases. 1 Tropical medicine - trends. 2 Endemic diseases. 3 Poverty areas. 4. Parasitic diseases. 5 Developing countries. 6. Annual reports. I. World Health Organization ISBN 978 92 4 1564090 (NLM Classification: WC 680) Working to overcome the global impact of neglected tropical diseases was produced under the overall direction and supervision of Dr Lorenzo Savioli (Director, WHO Department of Control of Neglected Tropical Diseases) and Dr Denis Daumerie (Programme Manager, WHO Department of Control of Neglected Tropical Diseases), with contributions from staff serving in the department. Regional directors and members of their staff provided support and advice. Valuable inputs in the form of contributions, peer reviews and suggestions were received by members of the Strategic and Technical Advisory Group for Neglected Tropical Diseases. The report was edited by Professor David W.T. Crompton, assisted by Mrs Patricia Peters. © World Health Organization 2010 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; e-mail: [email protected]). -

Download&Gid=20125
154th SESSION OF THE EXECUTIVE COMMITTEE Washington, D.C., USA, 16-20 June 2014 Provisional Agenda Item 4.1 CE154/10 17 April 2014 Original: English PRELIMINARY FINAL REPORT OF THE PAHO STRATEGIC PLAN 2008-2013 AND END-OF-BIENNIUM ASSESSMENT OF THE PROGRAM AND BUDGET 2012-2013 CE154/10 TABLE OF CONTENTS Page I. EXECUTIVE SUMMARY .........................................................................................3 II. INTRODUCTION........................................................................................................7 III. OVERVIEW OF THE PERFORMANCE MONITORING AND ASSESSMENT (PMA) PROCESS IN PAHO………………………………………… 8 Programmatic Assessment .......................................................................................9 Budgetary Assessment and Resource Analysis .......................................................9 IV. REGIONAL HEALTH OVERVIEW......................................................................11 A. Communicable Diseases .................................................................................11 B. NCDs and Risk Factors ..................................................................................14 C. Maternal, Child, Adolescent, and Elderly Health and Nutrition ....................17 D. Emergency and Disaster Preparedness ...........................................................18 E. Social, Economic, and Environmental Determinants of Health .....................20 F. Health Systems and Services ..........................................................................22 Main -

North-South Dialogue and Global Inequality: Meaning, Challenges and Prospects
NORTH-SOUTH DIALOGUE AND GLOBAL INEQUALITY: MEANING, CHALLENGES AND PROSPECTS ALEXANDER NNAEMEKA AGBAENYI [email protected] and [email protected] and PROF. MICHAEL CHEDEBE ODDIH Department of Political Science, Nnamdi Azikiwe University, Awka, Nigeria, Abstract General inequality in development between global North and South is identified as a major source of crises threatening global peace and security. North-South Dialogue is an approach designed to use summits, conferences, dialogues, negotiations, and meetings to achieve agreements, and programmes that can reduce this imbalance. However, analysts have argued that North-South Dialogue is characterized by words without actions based on the persistent socio-economic and political inequality existing between the two divides. This paper looks at the meaning and yardstick for classifying North and South. It shows the manifestations of this inequality and identified factors that contributed to it. We look at some of these dialogues and x-ray those problems that undermine North-South Dialogue from achieving its objectives. Insincerity in words and actions from both Northern and Southern participants is identified as a major setback for achieving the targeted objectives. For the North, national and business interests, selfishly perceived, are seen to have constituted major hindrances to the implementation of agreements and programmes reached in the dialogues. Again, corrupt practices, and poor leadership are spotted as major hindrances undermining South's strength in the struggle to reduce the gap. Keywords: North and South, North-South Dialogue, Global Inequality Introduction The global environment is characterized by relations that cut across states, regions, and the wider North-South divisions. Gap in socio-economic, political and military developments between the North and the South has attracted reactions and dialogues seeking to address the prevailing imbalances existing between them. -

Bourses De L'école De Santé Publique, Université De Montréal
Bourses de l’École de Santé Publique, Université de Montréal, Canada Information aux partenaires Commonwealth dans le cadre du projet des bourses de la reine Elizabeth II 1. Informations générales du projet Organisme subventionnaire : Gouvernement du Canada Programme : Bourses du jubilé de diamant de la reine Élizabeth II, 2015-2018 Montant total : $998,737 (Montant alloué par le programme Bourses de la Reine: $496,630/ Montant contribué par l’Université de Montréal $440,041) Comité du pilotage : Pierre Fournier, Christina Zarowsky, Mira Johri, Islene Lazo Directrice du projet : Christina Zarowsky Coordonnatrice du projet : Islene Lazo Professeurs collaborateurs : Nicole Beaudet, Valery Ridde, Barthélemy Kuate Defo, Nazmul Alam Institutions partenaires : ONG, CAREH, Caring for Education and Health Foundation, Cameroun careh.info@careh- cm.org Indian Institute of Health Management Research, IIHMR University Jaipur, Rajasthan, Inde [email protected] International Centre for Diarrheal Disease Research, Bangladesh [email protected] African Population and Health Research Centre, ONG, Kenya [email protected] School of Public Health, university of the Western Cape Université, Afrique du Sud [email protected] 2. Résumé du projet Projet : «Partenariat pour un leadership en santé globale bilingue dans le Commonwealth». L'École de Santé Publique de l'Université de Montréal/USI a remporté par concours un projet des bourses de la reine Elizabeth II, 2015 – 2018. Ces bourses favorisent les échanges interculturels axés sur l’acquisition d’expériences -
Screen Toronto's G20 Protests, Police Brutality, and the Unaccountability
Socialist Studies / Études socialistes 7(1/2) Spring/Fall 2011: 282‐302 Copyright © 2011 The Author(s) SPECIAL ISSUE ON ORGANIZING FOR AUSTERITY: THE NEOLIBERAL STATE, REGULATING LABOUR AND WORKING CLASS RESISTANCE “The Big Smoke” Screen Toronto’s G20 Protests, Police Brutality, and the Unaccountability of Public Officials IAN HUSSEY and PATRICE LeCLERC Sociology, York University. Toronto, Ontario, Canada. Sociology, St. Lawrence University. Canton, New York, USA. Abstract The G8 and G20 summits took place in Huntsville and Toronto, Ontario, Canada on 25‐ 26 and 26‐27 June 2010 respectively. Summits such as these often have large budgets attached to them and attract protests from people with various political leanings deploying a diversity of tactics, and these particular summits were no exception. In this article, we contrast official and media accounts of the protest and the policing of the events with a narrative grounded in protestors’ experience, in an attempt to complicate present popular understandings of these protests. In the discussion section of the article we provide theoretical and analytic insights into what the events of last summer can tell us about organizing and policing dissent. Résumé Le sommets du G8 et du G20 se sont tenus à Huntsville et Toronto, Ontario, Canada le 25‐26 et 26‐27 juin 2010 respectivement. Les sommets comme ceux‐ci ont généralement des budgets importants et attirent des manifestations organisées par des individus avec des tendances politiques multiples, utilisant des stratégies diverses. Ces sommets ne font pas exception. Dans cet article, nous contrastons les descriptions des manifestations et du comportement de la police par les sources officielles et les médias, avec les récits issus de l’expérience des manifestants, dans un souci de complexifier la compréhension populaire des ces manifestations. -
Epn Forum 2014 Report
EPN FORUM 2014 REPORT 28 - 29 April 2014 Maternal and Child Health Care- NAIROBI Access to Safe Pharmaceuticals. EPN FORUM 2014 REPORT Contents MATERNAL AND CHILD HEALTH CARE-ACCESS TO SAFE PHARMACEUTICALS 3 Introduction .............................................................................................. 3 EPN Achievements since 2012 ...................................................................... 4 Priority Life-Saving Medicines for Maternal and Child Health .............................. 5 Introduction ............................................................................................ 5 Paediatric medicines Regulators' Network ..................................................... 7 Improving Access to Essential Commodities for Maternal, Newborn and Child Health - Improved Access. Improved Services. Better Health Outcomes. ....................................... 7 SIAPS Goal and Objective .......................................................................... 7 Selection ................................................................................................ 8 Procurement ........................................................................................... 9 Distribution and storage ............................................................................ 9 Inventory Management ............................................................................10 Use ......................................................................................................10 Management Support ..............................................................................10 -

THE CBW CONVENTIONS BULLETIN News, Background and Comment on Chemical and Biological Weapons Issues
THE CBW CONVENTIONS BULLETIN News, Background and Comment on Chemical and Biological Weapons Issues ISSUE NO. 63 MARCH 2004 Quarterly Journal of the Harvard Sussex Program on CBW Armament and Arms Limitation IMPACT OF THE CWC: PROGRESSIVE DEVELOPMENT OF CUSTOMARY INTERNATIONAL LAW AND EVOLUTION OF THE CUSTOMARY NORM AGAINST CHEMICAL WEAPONS Lisa Tabassi* Legal Officer, OPCW Technical Secretariat Sources of law creating the norm prohibiting plex international verification regime ever: encompassing chemical weapons reporting obligations, intrusive international inspections, and The most authoritative statement on the sources and hierar- trade restrictions. However, the Chemical Weapons Con- chy of international law is set forth in Article 38 of the Stat- vention represents a novelty in the field of disarmament and ute of the International Court of Justice as follows: (a) inter- arms control2 and is very recent. At this point in time, what national conventions; (b) international custom, as evidence is the content of the rule as crystallized in custom and what of a general practice accepted as law; (c) general principles might be developing under the Convention as emergent cus- of law recognised by civilised nations; and, finally, (d) judi- tomary law? The number of states parties to the CWC is cial decisions (without according them precedential value) nearly universal and state practice consistently reflects re- and the teachings of the most highly qualified publicists of spect for the treaty norms. As these factors persist, the the various nations, as a subsidiary means for the determina- impact of the CWC on customary international law could tion of rules of law. become markedly significant, particularly if states parties In the case of the prohibition of chemical weapons, the exercise treaty obligations vis-à-vis states not party. -
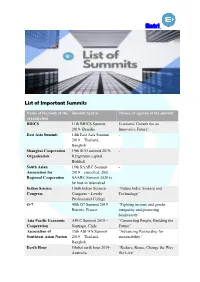
Entri List of Important Summits
Entri List of Important Summits Name of the body of the Summit held at Theme or agenda of the summit organization BRICS 11th BRICS Summit Economic Growth for an 2019- Brasilia Innovative Future’. East Asia Summit 14th East Asia Summit - 2019 – Thailand, Bangkok Shanghai Cooperation 19th SCO summit 2019- - Organisation Kyrgyzstan capital, Bishkek South Asian 19th SAARC Summit - Association for 2019 – cancelled. 20th Regional Cooperation SAARC Summit 2020 to be host in Islamabad Indian Science 106th Indian Science “Future India: Science and Congress Congress – Lovely Technology” Professional College G-7 45th G7 Summit 2019 – “Fighting income and gender Biarritz, France inequality and protecting biodiversity” Asia Pacific Economic APEC Summit 2019 – “Connecting People, Building the Cooperation Santiago, Chile Future” Association of 35th ASEAN Summit “Advancing Partnership for Southeast Asian Nation 2019 – Thailand, sustainability.” Bangkok. Earth Hour Global earth hour 2019- “Reduce, Reuse, Change the Way Australia We Live” Entri BIMSTEC 5th BIMSTEC Summit - 2019 – Sri Lanka (to be held) Indo-Africa Summit 4th Indo-Africa Forum “India and Africa: Deepening the Summit 2018 – New Security Engagement” Delhi. This Summit is held every 3 years CHOGM Summit CHOGM 2019 Meeting – Delivering A Common Future: Rwanda Connecting, Innovating, Transforming’ COP (UNFCCC) COP 25th 2019- Madrid, - Spain (to be held in December) HEMCE- High Energy 12th High Energy - Materials Society of Materials Conference India 2019 – IIT Madras, Chennai, India. 3rd Asian Ministerial New Delhi Tiger conservation Conference on Tiger Conservation World Government 7th World Government ‘Shaping Future Governments,’ Summit Summit- Dubai G-20 14th G 20 Summit 2019 – 8 themes of G 20 Summit – Osaka, Japan “Global Economy”, “Trade and Investment”, “Innovation”, “Environment and Energy”, “Employment”, “Women’s empowerment”, “Development” and “Health”.