Bisphenol a and Bile Acids
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Polymorphic Human Sulfotransferase 2A1 Mediates the Formation of 25-Hydroxyvitamin
Supplemental material to this article can be found at: http://dmd.aspetjournals.org/content/suppl/2018/01/17/dmd.117.078428.DC1 1521-009X/46/4/367–379$35.00 https://doi.org/10.1124/dmd.117.078428 DRUG METABOLISM AND DISPOSITION Drug Metab Dispos 46:367–379, April 2018 Copyright ª 2018 by The American Society for Pharmacology and Experimental Therapeutics Polymorphic Human Sulfotransferase 2A1 Mediates the Formation of 25-Hydroxyvitamin D3-3-O-Sulfate, a Major Circulating Vitamin D Metabolite in Humans s Timothy Wong, Zhican Wang, Brian D. Chapron, Mizuki Suzuki, Katrina G. Claw, Chunying Gao, Robert S. Foti, Bhagwat Prasad, Alenka Chapron, Justina Calamia, Amarjit Chaudhry, Erin G. Schuetz, Ronald L. Horst, Qingcheng Mao, Ian H. de Boer, Timothy A. Thornton, and Kenneth E. Thummel Departments of Pharmaceutics (T.W., Z.W., B.D.C., M.S., K.G.C., C.G., B.P., Al.C., J.C., Q.M., K.E.T.), Medicine and Kidney Research Institute (I.H.d.B.), and Biostatistics (T.A.T.), University of Washington, Seattle, Washington; Department of Pharmacokinetics and Drug Metabolism, Amgen Inc., South San Francisco, California (Z.W.); Department of Pharmacokinetics and Drug Metabolism, Amgen Inc., Cambridge, Massachusetts (R.S.F.); St. Jude Children’s Research Hospital, Memphis, Tennessee Downloaded from (Am.C., E.G.S.); and Heartland Assays LLC, Ames, Iowa (R.L.H.) Received September 1, 2017; accepted January 10, 2018 ABSTRACT dmd.aspetjournals.org Metabolism of 25-hydroxyvitamin D3 (25OHD3) plays a central role in with the rates of dehydroepiandrosterone sulfonation. Further analysis regulating the biologic effects of vitamin D in the body. -

Transcriptomic Characterization of Fibrolamellar Hepatocellular
Transcriptomic characterization of fibrolamellar PNAS PLUS hepatocellular carcinoma Elana P. Simona, Catherine A. Freijeb, Benjamin A. Farbera,c, Gadi Lalazara, David G. Darcya,c, Joshua N. Honeymana,c, Rachel Chiaroni-Clarkea, Brian D. Dilld, Henrik Molinad, Umesh K. Bhanote, Michael P. La Quagliac, Brad R. Rosenbergb,f, and Sanford M. Simona,1 aLaboratory of Cellular Biophysics, The Rockefeller University, New York, NY 10065; bPresidential Fellows Laboratory, The Rockefeller University, New York, NY 10065; cDivision of Pediatric Surgery, Department of Surgery, Memorial Sloan-Kettering Cancer Center, New York, NY 10065; dProteomics Resource Center, The Rockefeller University, New York, NY 10065; ePathology Core Facility, Memorial Sloan-Kettering Cancer Center, New York, NY 10065; and fJohn C. Whitehead Presidential Fellows Program, The Rockefeller University, New York, NY 10065 Edited by Susan S. Taylor, University of California, San Diego, La Jolla, CA, and approved September 22, 2015 (received for review December 29, 2014) Fibrolamellar hepatocellular carcinoma (FLHCC) tumors all carry a exon of DNAJB1 and all but the first exon of PRKACA. This deletion of ∼400 kb in chromosome 19, resulting in a fusion of the produced a chimeric RNA transcript and a translated chimeric genes for the heat shock protein, DNAJ (Hsp40) homolog, subfam- protein that retains the full catalytic activity of wild-type PKA. ily B, member 1, DNAJB1, and the catalytic subunit of protein ki- This chimeric protein was found in 15 of 15 FLHCC patients nase A, PRKACA. The resulting chimeric transcript produces a (21) in the absence of any other recurrent mutations in the DNA fusion protein that retains kinase activity. -

Chronic Exposure to Bisphenol a Reduces SULT1A1 Activity in the Human Placental Cell Line Bewo
Chronic exposure to bisphenol A reduces SULT1A1 activity in the human placental cell line BeWo Pallabi Mitra Department of Pharmaceutical Chemistry University of Kansas October 27, 2006 Outline ▪ Placental structure and models ▪ Placental permeation ▪ Placental metabolism and regulation (induction/inhibition) ▪ Sulfotransferase enzymes in trophoblast ▪ Bisphenol A ▪ Effects of bisphenol A on SULT1A1 ▪ Conclusions The placental barrier The placental barrier Mother’s blood •Trophoblasts and syncytiotrophoblasts line the maternal villar surface in a monolayer- like fashion. •Constitute the rate limiting barrier to exchange between the maternal and fetal blood. Syme et al., Drug transfer and metabolism by the human placenta, Clin Pharmacokinet 2004: 43(8): 487-514 Models of the human placenta ▪ In vivo models – Anatomical and functional differences between mammalian placentas makes it difficult to extrapolate animal studies to humans. ▪ In vitro models ▪ Perfused placental cotyledon ▪ Isolated trophoblast plasma membrane ▪ Isolated transporters and receptors ▪ Villous explants ▪ Primary cultures (cytotrophoblasts) ▪ Immortalized cell lines (BeWo, JAr, JEG, HRP-1, etc.) Refn. Bode et al. In Vitro models for studying trophoblast transcellular transport, Methods Mol Med. 2006;122:225-39 Sastry, B.V., Adv Drug Deliv Rev., 1999 Jun 14. 38(1): p. 17-39. Placental permeation - Factors Efflux Carrier-mediated Passive diffusion transport Metabolism A A X A A Maternal side A X-OH A Fetal side Placental metabolism ▪ Though enzyme expression is much more restricted than hepatic metabolism, those that are functional metabolize xenobiotics as well as hormones. ▪ Placental enzymes CYP1A1/1A2, CYP19 (aromatase), GST, UGT, SULT ▪ Maternal blood-borne chemicals (drugs/polychlorinated biphenyls/pesticides) alter expression and activity. • Altered steroid metabolism. -

Regulation of Xenobiotic and Bile Acid Metabolism by the Anti-Aging Intervention Calorie Restriction in Mice
REGULATION OF XENOBIOTIC AND BILE ACID METABOLISM BY THE ANTI-AGING INTERVENTION CALORIE RESTRICTION IN MICE By Zidong Fu Submitted to the Graduate Degree Program in Pharmacology, Toxicology, and Therapeutics and the Graduate Faculty of the University of Kansas in partial fulfillment of the requirements for the degree of Doctor of Philosophy. Dissertation Committee ________________________________ Chairperson: Curtis Klaassen, Ph.D. ________________________________ Udayan Apte, Ph.D. ________________________________ Wen-Xing Ding, Ph.D. ________________________________ Thomas Pazdernik, Ph.D. ________________________________ Hao Zhu, Ph.D. Date Defended: 04-11-2013 The Dissertation Committee for Zidong Fu certifies that this is the approved version of the following dissertation: REGULATION OF XENOBIOTIC AND BILE ACID METABOLISM BY THE ANTI-AGING INTERVENTION CALORIE RESTRICTION IN MICE ________________________________ Chairperson: Curtis Klaassen, Ph.D. Date approved: 04-11-2013 ii ABSTRACT Calorie restriction (CR), defined as reduced calorie intake without causing malnutrition, is the best-known intervention to increase life span and slow aging-related diseases in various species. However, current knowledge on the exact mechanisms of aging and how CR exerts its anti-aging effects is still inadequate. The detoxification theory of aging proposes that the up-regulation of xenobiotic processing genes (XPGs) involved in phase-I and phase-II xenobiotic metabolism as well as transport, which renders a wide spectrum of detoxification, is a longevity mechanism. Interestingly, bile acids (BAs), the metabolites of cholesterol, have recently been connected with longevity. Thus, this dissertation aimed to determine the regulation of xenobiotic and BA metabolism by the well-known anti-aging intervention CR. First, the mRNA expression of XPGs in liver during aging was investigated. -

Identification of Human Sulfotransferases Involved in Lorcaserin N-Sulfamate Formation
1521-009X/44/4/570–575$25.00 http://dx.doi.org/10.1124/dmd.115.067397 DRUG METABOLISM AND DISPOSITION Drug Metab Dispos 44:570–575, April 2016 Copyright ª 2016 by The American Society for Pharmacology and Experimental Therapeutics Identification of Human Sulfotransferases Involved in Lorcaserin N-Sulfamate Formation Abu J. M. Sadeque, Safet Palamar,1 Khawja A. Usmani, Chuan Chen, Matthew A. Cerny,2 and Weichao G. Chen3 Department of Drug Metabolism and Pharmacokinetics, Arena Pharmaceuticals, Inc., San Diego, California Received September 30, 2015; accepted January 7, 2016 ABSTRACT Lorcaserin [(R)-8-chloro-1-methyl-2,3,4,5-tetrahydro-1H-3-benza- and among the SULT isoforms SULT1A1 was the most efficient. The zepine] hydrochloride hemihydrate, a selective serotonin 5-hydroxy- order of intrinsic clearance for lorcaserin N-sulfamate is SULT1A1 > Downloaded from tryptamine (5-HT) 5-HT2C receptor agonist, is approved by the U.S. SULT2A1 > SULT1A2 > SULT1E1. Inhibitory effects of lorcaserin Food and Drug Administration for chronic weight management. N-sulfamate on major human cytochrome P450 (P450) enzymes Lorcaserin is primarily cleared by metabolism, which involves were not observed or minimal. Lorcaserin N-sulfamate binds to multiple enzyme systems with various metabolic pathways in human plasma protein with high affinity (i.e., >99%). Thus, despite humans. The major circulating metabolite is lorcaserin N-sulfamate. being the major circulating metabolite, the level of free lorcaserin Both human liver and renal cytosols catalyze the formation of N-sulfamate would be minimal at a lorcaserin therapeutic dose and lorcaserin N-sulfamate, where the liver cytosol showed a higher unlikely be sufficient to cause drug-drug interactions. -

Taurine Conjugated Bile Acids in Healthy Subjects
Gut: first published as 10.1136/gut.24.3.249 on 1 March 1983. Downloaded from Cl1t,I98-3. 24, 2249-252 Postprandial plasma concentrations of glycine and taurine conjugated bile acids in healthy subjects K LINNET Fronti tlh,e Departmen t of (-Ctlnicll (Chew istrrv ktred(riksbe,rg, Hospital. C(openIhagen Dentllark SUMMARY Fasting and postprandial plasma concentrations of glycine and taurine conjugates of cholic, chenodeoxycholic. and deoxvcholic acid were measured by a high pressure liquid chromatography-enzymatic assay in nine healthy subjects. The mean value of each bile acid concentration increased significantly (2 4-4.7 times) in the postprandial period. The total glycine/taurine ratio of 2.5 in the fasting state increased significantly to a maximum value of 3 3 at one to 18 hours postprandially and then declined. This shift in glycine/taurine ratio shows, that the relative increase in concentrations of glvcine conjugates exceeds the relative increase in concentrations of taurine conjugates in the early postprandial period, and supports the view that there is significant absorption of glycine conjugated bile acids from the proximal small intestine. Measurements of fasting and postprandial serum Methods concentrations of individual bile acids have so far been performed by radioimmunoassav or gas SUBJECTS chromatographv.' Before analvsis by aas The study was carried out in nine healthy http://gut.bmj.com/ chromatography the bile acids are deconjugated. so volunteers, four women and five men, with a mean that both free and conjugated bile acids are age of 24 years (interval 17-40 years). The subjects measured and no information is obtained regarding were fasted overnight, and in the morning blood the amino acid of the conjugate (glycine or taurine). -

Systemic Gut Microbial Modulation of Bile Acid Metabolism in Host Tissue Compartments
Systemic gut microbial modulation of bile acid metabolism in host tissue compartments Jonathan R. Swanna,b, Elizabeth J. Wanta, Florian M. Geiera, Konstantina Spagoua, Ian D. Wilsonc, James E. Sidawayd, Jeremy K. Nicholsona,1, and Elaine Holmesa,1 aBiomolecular Medicine, Department of Surgery and Cancer, Faculty of Medicine, Imperial College, London SW7 2AZ, United Kingdom; bDepartment of Food and Nutritional Sciences, School of Chemistry, Food and Pharmacy, The University of Reading, Reading RG6 6AP, United Kingdom; cAstraZeneca, Department of Clinical Pharmacology, Drug Metabolism and Pharmacokinetics; and dAstraZeneca, Global Safety Assessment, Cheshire SK10 4TG, United Kingdom Edited by Todd R. Klaenhammer, North Carolina State University, Raleigh, NC, and approved July 30, 2010 (received for review May 26, 2010) We elucidate the detailed effects of gut microbial depletion on the deconjugation, dehydrogenation, dehydroxylation, and sulfation bile acid sub-metabolome of multiple body compartments (liver, reactions (8) to produce secondary bile acids, which are reabsorbed kidney, heart, and blood plasma) in rats. We use a targeted ultra- and returned to the liver for further processing. performance liquid chromatography with time of flight mass-spec- Historically, bile acids have been primarily viewed as detergent trometry assay to characterize the differential primary and secondary molecules important for the absorption of dietary fats and lipid- bile acid profiles in each tissue and show a major increase in the soluble vitamins in the small intestine and the maintenance of proportion of taurine-conjugated bile acids in germ-free (GF) and cholesterol homeostasis in the liver. However, their role in the antibiotic (streptomycin/penicillin)-treated rats. Although conjugated mammalian system is much broader than this, and they are now bile acids dominate the hepatic profile (97.0 ± 1.5%) of conventional recognized as important signaling molecules with systemic endo- animals, unconjugated bile acids comprise the largest proportion of crine functions. -
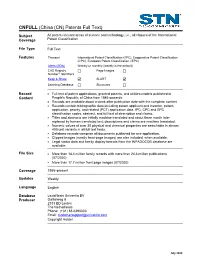
CNFULL Database Summary Sheet (DBSS)
(China (CN) Patents Full Text) CNFULL Subject All patent-relevant areas of science and technology, i.e., all classes of the International Coverage Patent Classification File Type Full Text Features Thesauri International Patent Classification (/IPC), Cooperative Patent Classification (CPC), European Patent Classification (/EPC) Alerts (SDIs) Weekly or monthly (weekly is the default) CAS Registry Page Images ® Number Identifiers Keep & Share SLART Learning Database Structures Record • Full text of patent applications, granted patents, and utilities models published in Content People's Republic of China from 1985 onwards. • Records are available about a week after publication date with the complete content • Records contain bibliographic data including patent applicant and inventor, patent, application, priority, and related (PCT) application data, IPC, CPC and EPC classification codes, abstract, and full text of description and claims. • Titles and abstracts are initially machine translated and about three month later replaced by human translated text; descriptions and claims are machine translated. • Numeric values of over 30 physical and chemical properties are searchable in almost 400 unit variants in all full text fields. • Database records comprise all documents published for one application. • Clipped images (mostly front-page images) are also included, when available. • Legal status data and family display formats from the INPADOCDB database are available. File Size • More than 18.4 million family records with more than 24.8 million publications (07/2020) • More than 17.7 million front page images (07/2020) Coverage 1985–present Updates Weekly Language English Database LexisNexis Univentio BV Producer Galileiweg 8 2333 BD Leiden The Netherlands Phone: (+31) 88-6390000 Email: [email protected] Copyright Holder July 2020 2 CNFULL Database FIZ Karlsruhe Supplier STN Europe P.O. -

Increased Serum Bile Acid Concentration Following Low-Dose Chronic Administration of Thioacetamide in Rats, As Evidenced by Metabolomic Analysis
YTAAP-13425; No of Pages 10 Toxicology and Applied Pharmacology xxx (2015) xxx–xxx Contents lists available at ScienceDirect Toxicology and Applied Pharmacology journal homepage: www.elsevier.com/locate/ytaap Increased serum bile acid concentration following low-dose chronic administration of thioacetamide in rats, as evidenced by metabolomic analysis Eun Sook Jeong a, Gabin Kim a, Ho Jung Shin a, Se-Myo Park b, Jung-Hwa Oh b,Yong-BumKimb, Kyoung-Sik Moon b, Hyung-Kyoon Choi c, Jayoung Jeong d, Jae-Gook Shin a,DongHyunKima,⁎ a Department of Pharmacology and Pharmacogenomics Research Center, Inje University, College of Medicine, Bokjiro 75, Busanjin-Gu, Busan 614-735, Republic of Korea b Korea Institute of Toxicology, 141 Gajeong-ro, Yuseong-gu, Daejeon 305-343, Republic of Korea c College of Pharmacy, Chung-Ang University, Seoul, Republic of Korea d Ministry of Food and Drug Safety, Osong-eup, Heungdeok-gu, Cheongju-si, Chungcheongbuk-do 361-951, Republic of Korea article info abstract Article history: A liquid chromatography/time-of-flight mass spectrometry (LC/TOF-MS)-based metabolomics approach was Received 23 March 2015 employed to identify endogenous metabolites as potential biomarkers for thioacetamide (TAA)-induced liver in- Revised 18 July 2015 jury. TAA (10 and 30 mg/kg), a well-known hepatotoxic agent, was administered daily to male Sprague–Dawley Accepted 20 July 2015 (SD) rats for 28 days. We then conducted untargeted analyses of endogenous serum and liver metabolites. Partial Available online xxxx least squares discriminant analysis (PLS-DA) was performed on serum and liver samples to evaluate metabolites associated with TAA-induced perturbation. -

Molecular Genetic Markers Associated with Boar Taint – Could Molecular Genetics Contribute to Its Reduction?
RESEARCH IN PIG BREEDING, 13, 2019 (1) REVIEW: MOLECULAR GENETIC MARKERS ASSOCIATED WITH BOAR TAINT – COULD MOLECULAR GENETICS CONTRIBUTE TO ITS REDUCTION? Falková L. and Vrtková I. Laboratory of Agrogenomics, Department of Animal Morphology, Physiology and Genetics, Mendel University in Brno, Czech Republic Abstract Boar taint is an unpleasant meat odour or taste occurring in uncastrated male pigs usually. Naturally occurring compounds – androstenone, skatole and indole – and their accumulation in the adipose tissue of entire boars cause the perceptible boar taint. Individual levels or combination of these compounds lead to perception of boar taint observed during culinary process and pork consumption. The ban on surgical castration based on EU legislation makes it necessary to find a solution that enables our producers to adapt to these new conditions and ensure their competitiveness. Alternative options include the use of molecular genetic markers that affect the levels of androstenone and skatole in pig adipose tissue by Marker Assisted Selection (MAS). The aim of this review is to provide overview in recent facts in the field of molecular genetics and possibility in boar taint reduction solution. Key Words: Boar taint, genomic markers, selection Boar taint degree while in the skatole level besides genetic Boar taint is an unpleasant odour or taste of and age factor the nutrition and environmental meat from entire male pigs. The occurrence in factors play key role (Zamartskaia and Squires, adult pig males is connected with the hormone 2009). Skatole occurs in both male and female changes during maturation (Duijvesteijn et al., pigs but in male ones three times more (Wesoly 2010). -

Early Feeding of a High-Cholesterol Diet Enhances Intestinal Permeability to Lipids in Rabbits
003 1-3998/87/2 104-0347$02.00/0 PEDIATRIC RESEARCH Vol. 21, No. 4, 1987 Copyright O 1987 International Pediatric Research Foundation, Inc. I'rinted in U.S. A. Early Feeding of a High-Cholesterol Diet Enhances Intestinal Permeability to Lipids in Rabbits A. B. R. THOMSON, M. KEELAN, AND M. TAVERNINI Nutrition and Metabolism Research Group, University ofAlberta, Edmonton, Alberta, Canada ABSTRACT. This study was undertaken in young and stages in the animal's development (4). Complex changes occur growing rabbits to establish the of feeding a high- (2%) in the form and function of the digestive tract as animals develop cholesterol diet (HC) on the intestinal in vitro uptake of a (5, 6) and it remains unclear by what mechanism(s) the intestine homologous series of saturated fatty acids, dodecanol, cho- adapts (7). The reduced permeability of the intestine which lesterol, and bile acids. In the jejunum there was an in- occurs with aging is not due to major alterations in the mucosal crease in the uptake of myristic acid and dodecanol in HC surface area, although the perturbations in the lipid composition as compared with animals fed Purina Chow, whereas in of the microvillus membrane may account for some of these the ileum the uptake of stearic acid, cholesterol, and tau- changes in transport function (8, 9). Variations in dietary triac- rocholic acid was reduced. There was increased jejunal ylglycerol saturation alter the lipid composition and fluidity of uptake of medium-chain length fatty acids, increased in- rat intestinal plasma membranes (10) and there is considerable cremental change in free energy (JAFw -+ C), increased evidence that other dietary factors may influence the intestinal uptake of palmitic, taurocholic acid, and glycocholic acid absorption of nutrients (1 1). -

Estrogen-Metabolizing Gene Polymorphisms in the Assessment of Female Hormone-Dependent Cancer Risk
The Pharmacogenomics Journal (2006) 6, 189–193 & 2006 Nature Publishing Group All rights reserved 1470-269X/06 $30.00 www.nature.com/tpj ORIGINAL ARTICLE Estrogen-metabolizing gene polymorphisms in the assessment of female hormone-dependent cancer risk ON Mikhailova1, LF Gulyaeva1, Allelic variants of cytochrome P450: CYP1A1, CYP1A2, CYP19 (Aromatase) 1 2 and II-phase enzyme Sulfotransferase (SULT1A1) genes are associated with a AV Prudnikov , AV Gerasimov high risk of hormone-dependent cancers. We estimated a frequency of these 2 and SE Krasilnikov allelic variants in the female Caucasian population of the Novosibirsk region of Russia and their association with the elevated risk of ovarian and 1Institute of Molecular Biology and Biophysics, Novosibirsk, Russia and 2Regional Clinical endometrial cancer. A DNA bank of gynecologic oncology patients, patients Oncological Hospital, Novosibirsk, Russia with benign gynecologic diseases and healthy women was created, and the following single nucleotide polymorphisms (SNPs) were examined: CYP1A1 Correspondence: M1 polymorphism, that is, T264-C transition in the 30-noncoding region; Dr ON Mikhailova, Department of Molecular CYP1A2*1F polymorphism, that is, C734-A transversion in CYP1A2 gene; Mechanisms of Carcinogenesis, Institute of - Molecular Biology and Biophysics, Siberian C T transition (Arg264Cys) in exon 7 of CYP19; SULT1A1*2 polymorphism, Branch of the Russian Academy of Medical that is, G638-A transition (Arg213His) in SULT1A1 gene. A positive Sciences, Timakov Str. 2, Novosibirsk, correlation of C allele of CYP1A2*1F and G allele of SULT1A1*2 with 630117, Russia. hormone-dependent cancers in women was found. Thus, these genes are E-mail: [email protected] appropriate candidates for studying the contribution of genetic factors to endocrine disorder and environmentally determined diseases susceptibility.