The Role of Lipid Sensing Nuclear Receptors (Ppars and LXR) and Metabolic Lipases in Obesity, Diabetes and NAFLD
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Antidiabetic Drug Lobeglitazone Has the Potential to Inhibit PTP1B T Activity ⁎ Ruth F
Bioorganic Chemistry 100 (2020) 103927 Contents lists available at ScienceDirect Bioorganic Chemistry journal homepage: www.elsevier.com/locate/bioorg The antidiabetic drug lobeglitazone has the potential to inhibit PTP1B T activity ⁎ Ruth F. Rochaa, Tiago Rodriguesc, Angela C.O. Menegattia,b, , Gonçalo J.L. Bernardesc,d, Hernán Terenzia a Centro de Biologia Molecular Estrutural, Departamento de Bioquímica, Universidade Federal de Santa Catarina, Campus Trindade, 88040-900 Florianópolis, SC, Brazil b Universidade Federal do Piauí, CPCE, 64900-000 Bom Jesus, PI, Brazil c Instituto de Medicina Molecular, Faculdade de Medicina, Universidade de Lisboa, Avenida Professor Egas Moniz, 1649-028 Lisbon, Portugal d Department of Chemistry, University of Cambridge, Lensfield Road, CB2 1EW Cambridge, UK ARTICLE INFO ABSTRACT Keywords: Protein tyrosine phosphatase 1B (PTP1B) is considered a potential therapeutic target for the treatment of type 2 Thiazolidinediones diabetes mellitus (T2DM), since this enzyme plays a significant role to down-regulate insulin and leptin sig- Lobeglitazone nalling and its over expression has been implicated in the development of insulin resistance, T2DM and obesity. PPAR-γ Some thiazolidinediones (TZD) derivatives have been reported as promising PTP1B inhibitors with anti hy- PTP1B perglycemic effects. Recently, lobeglitazone, a new TZD, was described as an antidiabetic drug that targetsthe Non-competitive inhibitors PPAR-γ (peroxisome γ proliferator-activated receptor) pathway, but no information on its effects on PTP1B have been reported to date. We investigated the effects of lobeglitazone on PTP1B activity in vitro. Surprisingly, lobeglitazone led to moderate inhibition on PTP1B (IC50 42.8 ± 3.8 µM) activity and to a non-competitive reversible mechanism of action. -

Dualism of Peroxisome Proliferator-Activated Receptor Α/Γ: a Potent Clincher in Insulin Resistance
AEGAEUM JOURNAL ISSN NO: 0776-3808 Dualism of Peroxisome Proliferator-Activated Receptor α/γ: A Potent Clincher in Insulin Resistance Mr. Ravikumar R. Thakar1 and Dr. Nilesh J. Patel1* 1Faculty of Pharmacy, Shree S. K. Patel College of Pharmaceutical Education & Research, Ganpat University, Gujarat, India. [email protected] Abstract: Diabetes mellitus is clinical syndrome which is signalised by augmenting level of sugar in blood stream, which produced through lacking of insulin level and defective insulin activity or both. As per worldwide epidemiology data suggested that the numbers of people with T2DM living in developing countries is increasing with 80% of people with T2DM. Peroxisome proliferator-activated receptors are a family of ligand-activated transcription factors; modulate the expression of many genes. PPARs have three isoforms namely PPARα, PPARβ/δ and PPARγ that play a central role in regulating glucose, lipid and cholesterol metabolism where imbalance can lead to obesity, T2DM and CV ailments. It have pathogenic role in diabetes. PPARα is regulates the metabolism of lipids, carbohydrates, and amino acids, activated by ligands such as polyunsaturated fatty acids, and drugs used as Lipid lowering agents. PPAR β/δ could envision as a therapeutic option for the correction of diabetes and a variety of inflammatory conditions. PPARγ is well categorized, an element of the PPARs, also pharmacological effective as an insulin resistance lowering agents, are used as a remedy for insulin resistance integrated with type- 2 diabetes mellitus. There are mechanistic role of PPARα, PPARβ/δ and PPARγ in diabetes mellitus and insulin resistance. From mechanistic way, it revealed that dual PPAR-α/γ agonist play important role in regulating both lipids as well as glycemic levels with essential safety issues. -

Corporate Presentation June 2019 Disclaimer
Corporate Presentation June 2019 Disclaimer Some of the statements contained in this presentation constitute forward-looking statements. Statements that are not historical facts are forward-looking statements. Forward-looking statements generally can be identified by the use of forward-looking terminology such as “may”, “will”, “expect”, “intend”, “estimate”, “anticipate”, “believe”, “continue” or similar terminology. These statements are based on the Company’s current strategy, plans, objectives, assumptions, estimates and projections. Investors should therefore not place undue reliance on those statements. The Company makes no representation, warranty or prediction that the results anticipated by such forward- looking statements will be achieved, and such forward-looking statements represent, in each case, only one of many possible scenarios and should not be viewed as the most likely or standard scenario. Forward-looking statements speak only as of the date that they are made and the Company does not undertake to update any forward-looking statements in light of new information or future events. Forward-looking statements involve inherent risks and uncertainties. The Company cautions that a number of important factors could cause actual results to differ materially from those contained in any forward-looking statement. 2 Well Diversified Mid-to-Late Stage Metabolic Pipeline for Large Market Opportunities Global partnerships secured for late stage clinical program in type 2 diabetes • Imeglimin: First in class oral drug candidate targeting -

CDR Clinical Review Report for Soliqua
CADTH COMMON DRUG REVIEW Clinical Review Report Insulin glargine and lixisenatide injection (Soliqua) (Sanofi-Aventis) Indication: adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus inadequately controlled on basal insulin (less than 60 units daily) alone or in combination with metformin. Service Line: CADTH Common Drug Review Version: Final (with redactions) Publication Date: January 2019 Report Length: 118 Pages Disclaimer: The information in this document is intended to help Canadian health care decision-makers, health care professionals, health systems leaders, and policy-makers make well-informed decisions and thereby improve the quality of health care services. While patients and others may access this document, the document is made available for informational purposes only and no representations or warranties are made with respect to its fitness for any particular purpose. The information in this document should not be used as a substitute for professional medical advice or as a substitute for the application of clinical judgment in respect of the care of a particular patient or other professional judgment in any decision-making process. The Canadian Agency for Drugs and Technologies in Health (CADTH) does not endorse any information, drugs, therapies, treatments, products, processes, or services. While care has been taken to ensure that the information prepared by CADTH in this document is accurate, complete, and up-to-date as at the applicable date the material was first published by CADTH, CADTH does not make any guarantees to that effect. CADTH does not guarantee and is not responsible for the quality, currency, propriety, accuracy, or reasonableness of any statements, information, or conclusions contained in any third-party materials used in preparing this document. -

Advances in Hepatology
ADVANCES IN HEPATOLOGY Current Developments in the Treatment of Hepatitis and Hepatobiliary Disease Hepatology Section Editor: Eugene R. Schiff, MD Novel Therapies for Cholestatic Liver Disease Cynthia Levy, MD Professor of Medicine Arthur Hertz Chair in Liver Diseases Associate Director, Schiff Center for Liver Diseases Division of Hepatology University of Miami Miller School of Medicine Miami, Florida G&H Currently, how is cholestatic liver G&H What are the limitations of the therapies disease in adults typically treated? currently being used? CL Cholestatic liver disease in adults mainly consists of CL Up to 40% of patients with PBC may not respond to primary biliary cholangitis (PBC) and primary sclerosing UDCA therapy, meaning that they will not have signifi- cholangitis (PSC). For PBC, the traditional first-line treat- cant biochemical improvement in alkaline phosphatase, ment is ursodeoxycholic acid (UDCA), starting at a dose which will remain elevated above 1.5 or 2 times the upper of 13 to 15 mg/kg/day. In May 2016, obeticholic acid limit of normal. In addition, in the PBC clinical trials for (Ocaliva, Intercept Pharmaceuticals) was approved by the obeticholic acid, only half of the patients met the primary US Food and Drug Administration (FDA) for second- endpoint. Furthermore, as previously mentioned, there is line treatment of PBC patients who either do not respond no FDA-approved treatment for PSC. Therefore, there are to UDCA therapy or who are intolerant of it. Dosing for unmet needs for PBC and PSC treatment, which have led noncirrhotic or well-compensated cirrhotic patients is 5 to a plethora of ongoing clinical trials exploring drugs of mg daily, which can be increased to 10 mg daily after 3 various mechanisms of action. -

Us 2018 / 0296525 A1
UN US 20180296525A1 ( 19) United States (12 ) Patent Application Publication (10 ) Pub. No. : US 2018/ 0296525 A1 ROIZMAN et al. ( 43 ) Pub . Date: Oct. 18 , 2018 ( 54 ) TREATMENT OF AGE - RELATED MACULAR A61K 38 /1709 ( 2013 .01 ) ; A61K 38 / 1866 DEGENERATION AND OTHER EYE (2013 . 01 ) ; A61K 31/ 40 ( 2013 .01 ) DISEASES WITH ONE OR MORE THERAPEUTIC AGENTS (71 ) Applicant: MacRegen , Inc ., San Jose , CA (US ) (57 ) ABSTRACT ( 72 ) Inventors : Keith ROIZMAN , San Jose , CA (US ) ; The present disclosure provides therapeutic agents for the Martin RUDOLF , Luebeck (DE ) treatment of age - related macular degeneration ( AMD ) and other eye disorders. One or more therapeutic agents can be (21 ) Appl. No .: 15 /910 , 992 used to treat any stages ( including the early , intermediate ( 22 ) Filed : Mar. 2 , 2018 and advance stages ) of AMD , and any phenotypes of AMD , including geographic atrophy ( including non -central GA and Related U . S . Application Data central GA ) and neovascularization ( including types 1 , 2 and 3 NV ) . In certain embodiments , an anti - dyslipidemic agent ( 60 ) Provisional application No . 62/ 467 ,073 , filed on Mar . ( e . g . , an apolipoprotein mimetic and / or a statin ) is used 3 , 2017 . alone to treat or slow the progression of atrophic AMD Publication Classification ( including early AMD and intermediate AMD ) , and / or to (51 ) Int. CI. prevent or delay the onset of AMD , advanced AMD and /or A61K 31/ 366 ( 2006 . 01 ) neovascular AMD . In further embodiments , two or more A61P 27 /02 ( 2006 .01 ) therapeutic agents ( e . g ., any combinations of an anti - dys A61K 9 / 00 ( 2006 . 01 ) lipidemic agent, an antioxidant, an anti- inflammatory agent, A61K 31 / 40 ( 2006 .01 ) a complement inhibitor, a neuroprotector and an anti - angio A61K 45 / 06 ( 2006 .01 ) genic agent ) that target multiple underlying factors of AMD A61K 38 / 17 ( 2006 .01 ) ( e . -

Classification Decisions Taken by the Harmonized System Committee from the 47Th to 60Th Sessions (2011
CLASSIFICATION DECISIONS TAKEN BY THE HARMONIZED SYSTEM COMMITTEE FROM THE 47TH TO 60TH SESSIONS (2011 - 2018) WORLD CUSTOMS ORGANIZATION Rue du Marché 30 B-1210 Brussels Belgium November 2011 Copyright © 2011 World Customs Organization. All rights reserved. Requests and inquiries concerning translation, reproduction and adaptation rights should be addressed to [email protected]. D/2011/0448/25 The following list contains the classification decisions (other than those subject to a reservation) taken by the Harmonized System Committee ( 47th Session – March 2011) on specific products, together with their related Harmonized System code numbers and, in certain cases, the classification rationale. Advice Parties seeking to import or export merchandise covered by a decision are advised to verify the implementation of the decision by the importing or exporting country, as the case may be. HS codes Classification No Product description Classification considered rationale 1. Preparation, in the form of a powder, consisting of 92 % sugar, 6 % 2106.90 GRIs 1 and 6 black currant powder, anticaking agent, citric acid and black currant flavouring, put up for retail sale in 32-gram sachets, intended to be consumed as a beverage after mixing with hot water. 2. Vanutide cridificar (INN List 100). 3002.20 3. Certain INN products. Chapters 28, 29 (See “INN List 101” at the end of this publication.) and 30 4. Certain INN products. Chapters 13, 29 (See “INN List 102” at the end of this publication.) and 30 5. Certain INN products. Chapters 28, 29, (See “INN List 103” at the end of this publication.) 30, 35 and 39 6. Re-classification of INN products. -

Disease Progression and Pharmacological Intervention in a Nutrient‑Defcient Rat Model of Nonalcoholic Steatohepatitis
Digestive Diseases and Sciences https://doi.org/10.1007/s10620-018-5395-7 ORIGINAL ARTICLE Disease Progression and Pharmacological Intervention in a Nutrient‑Defcient Rat Model of Nonalcoholic Steatohepatitis Kirstine S. Tølbøl1,3,4 · Birgit Stierstorfer2 · Jörg F. Rippmann2 · Sanne S. Veidal1 · Kristofer T. G. Rigbolt1 · Tanja Schönberger2 · Matthew P. Gillum4 · Henrik H. Hansen1 · Niels Vrang1 · Jacob Jelsing1 · Michael Feigh1 · Andre Broermann2 Received: 14 June 2018 / Accepted: 22 November 2018 © The Author(s) 2018 Abstract Background There is a marked need for improved animal models of nonalcoholic steatohepatitis (NASH) to facilitate the development of more efcacious drug therapies for the disease. Methods Here, we investigated the development of fbrotic NASH in male Wistar rats fed a choline-defcient L-amino acid- defned (CDAA) diet with or without cholesterol supplementation for subsequent assessment of drug treatment efcacy in NASH biopsy-confrmed rats. The metabolic profle and liver histopathology were evaluated after 4, 8, and 12 weeks of dieting. Subsequently, rats with biopsy-confrmed NASH were selected for pharmacological intervention with vehicle, elafbranor (30 mg/kg/day) or obeticholic acid (OCA, 30 mg/kg/day) for 5 weeks. Results The CDAA diet led to marked hepatomegaly and fbrosis already after 4 weeks of feeding, with further progression of collagen deposition and fbrogenesis-associated gene expression during the 12-week feeding period. Cholesterol supple- mentation enhanced the stimulatory efect of CDAA on gene transcripts associated with fbrogenesis without signifcantly increasing collagen deposition. Pharmacological intervention with elafbranor, but not OCA, signifcantly reduced stea- tohepatitis scores, and fbrosis-associated gene expression, however, was unable to prevent progression in fbrosis scores. -
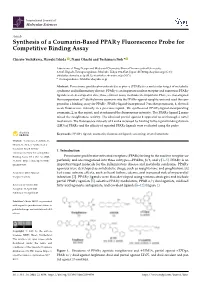
Synthesis of a Coumarin-Based PPAR Fluorescence Probe for Competitive Binding Assay
International Journal of Molecular Sciences Article Synthesis of a Coumarin-Based PPARγ Fluorescence Probe for Competitive Binding Assay Chisato Yoshikawa, Hiroaki Ishida , Nami Ohashi and Toshimasa Itoh * Laboratory of Drug Design and Medicinal Chemistry, Showa Pharmaceutical University, 3-3165 Higashi-Tamagawagakuen, Machida, Tokyo 194-8543, Japan; [email protected] (C.Y.); [email protected] (H.I.); [email protected] (N.O.) * Correspondence: [email protected] Abstract: Peroxisome proliferator-activated receptor γ (PPARγ) is a molecular target of metabolic syndrome and inflammatory disease. PPARγ is an important nuclear receptor and numerous PPARγ ligands were developed to date; thus, efficient assay methods are important. Here, we investigated the incorporation of 7-diethylamino coumarin into the PPARγ agonist rosiglitazone and used the com- pound in a binding assay for PPARγ. PPARγ-ligand-incorporated 7-methoxycoumarin, 1, showed weak fluorescence intensity in a previous report. We synthesized PPARγ-ligand-incorporating coumarin, 2, in this report, and it enhanced the fluorescence intensity. The PPARγ ligand 2 main- tained the rosiglitazone activity. The obtained partial agonist 6 appeared to act through a novel mechanism. The fluorescence intensity of 2 and 6 increased by binding to the ligand binding domain (LBD) of PPARγ and the affinity of reported PPARγ ligands were evaluated using the probe. Keywords: PPARγ ligand; coumarin; fluorescent ligand; screening; crystal structure Citation: Yoshikawa, C.; Ishida, H.; Ohashi, N.; Itoh, T. Synthesis of a Coumarin-Based PPARγ 1. Introduction Fluorescence Probe for Competitive Binding Assay. Int. J. Mol. Sci. 2021, Peroxisome proliferator-activated receptors (PPARs) belong to the nuclear receptor su- 22, 4034. -

A61p1/16 (2006.01) A61p3/00 (2006.01) Km, Ml, Mr, Ne, Sn, Td, Tg)
( (51) International Patent Classification: TR), OAPI (BF, BJ, CF, CG, Cl, CM, GA, GN, GQ, GW, A61P1/16 (2006.01) A61P3/00 (2006.01) KM, ML, MR, NE, SN, TD, TG). A61K 31/192 (2006.01) C07C 321/28 (2006.01) Declarations under Rule 4.17: (21) International Application Number: — as to the applicant's entitlement to claim the priority of the PCT/IB2020/000808 earlier application (Rule 4.17(iii)) (22) International Filing Date: Published: 25 September 2020 (25.09.2020) — with international search report (Art. 21(3)) (25) Filing Language: English — before the expiration of the time limit for amending the claims and to be republished in the event of receipt of (26) Publication Language: English amendments (Rule 48.2(h)) (30) Priority Data: 62/906,288 26 September 2019 (26.09.2019) US (71) Applicant: ABIONYX PHARMA SA [FR/FR] ; 33-43 Av¬ enue Georges Pompidou, Batiment D, 31130 Bahna (FR). (72) Inventor: DASSEUX, Jean-Louis, Henri; 7 Allees Charles Malpel, Bat. B, 31300 Toulouse (FR). (74) Agent: HOFFMANN EITLE PATENT- UND RECHTSANWALTE PARTMBB, ASSOCIATION NO. 151; Arabellastrasse 30, 81925 Munich (DE). (81) Designated States (unless otherwise indicated, for every kind of national protection available) : AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DJ, DK, DM, DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, HN, HR, HU, ID, IL, IN, IR, IS, IT, JO, JP, KE, KG, KH, KN, KP, KR, KW, KZ, LA, LC, LK, LR, LS, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, SC, SD, SE, SG, SK, SL, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, WS, ZA, ZM, ZW. -

2 to Modulate Hepatic Lipolysis and Fatty Acid Metabolism
Original article Bioenergetic cues shift FXR splicing towards FXRa2 to modulate hepatic lipolysis and fatty acid metabolism Jorge C. Correia 1,2, Julie Massart 3, Jan Freark de Boer 4, Margareta Porsmyr-Palmertz 1, Vicente Martínez-Redondo 1, Leandro Z. Agudelo 1, Indranil Sinha 5, David Meierhofer 6, Vera Ribeiro 2, Marie Björnholm 3, Sascha Sauer 6, Karin Dahlman-Wright 5, Juleen R. Zierath 3, Albert K. Groen 4, Jorge L. Ruas 1,* ABSTRACT Objective: Farnesoid X receptor (FXR) plays a prominent role in hepatic lipid metabolism. The FXR gene encodes four proteins with structural differences suggestive of discrete biological functions about which little is known. Methods: We expressed each FXR variant in primary hepatocytes and evaluated global gene expression, lipid profile, and metabolic fluxes. Gene À À delivery of FXR variants to Fxr / mouse liver was performed to evaluate their role in vivo. The effects of fasting and physical exercise on hepatic Fxr splicing were determined. Results: We show that FXR splice isoforms regulate largely different gene sets and have specific effects on hepatic metabolism. FXRa2 (but not a1) activates a broad transcriptional program in hepatocytes conducive to lipolysis, fatty acid oxidation, and ketogenesis. Consequently, FXRa2 À À decreases cellular lipid accumulation and improves cellular insulin signaling to AKT. FXRa2 expression in Fxr / mouse liver activates a similar gene program and robustly decreases hepatic triglyceride levels. On the other hand, FXRa1 reduces hepatic triglyceride content to a lesser extent and does so through regulation of lipogenic gene expression. Bioenergetic cues, such as fasting and exercise, dynamically regulate Fxr splicing in mouse liver to increase Fxra2 expression. -

Regulation of Thyroid Hormone Activation Via the Liver X-Receptor/Retinoid X-Receptor Pathway
179 Regulation of thyroid hormone activation via the liver X-receptor/retinoid X-receptor pathway Marcelo A Christoffolete*, Ma´rton Doleschall1,*, Pe´ter Egri1, Zsolt Liposits1, Ann Marie Zavacki2, Antonio C Bianco3 and Bala´zs Gereben1 Human and Natural Sciences Center, Federal University of ABC, Santo Andre-SP 09210-370, Brazil 1Laboratory of Endocrine Neurobiology, Institute of Experimental Medicine, Hungarian Academy of Sciences, Szigony u. 43, Budapest H-1083, Hungary 2Division of Endocrinology, Diabetes, and Hypertension, Thyroid Section, Brigham and Women’s Hospital, Boston, Massachusetts MA 02115, USA 3Division of Endocrinology, Diabetes and Metabolism, Miller School of Medicine, University of Miami, Miami, Florida FL 33136, USA (Correspondence should be addressed to B Gereben; Email: [email protected]) *(M A Christoffolete and M Doleschall contributed equally to this work) (M Doleschall is now at Inflammation Biology and Immungenomics Research Group, Hungarian Academy of Sciences, Semmelweis University, Budapest, Hungary) Abstract Thyroid hormone receptor (TR) and liver X-receptor (LXR) investigated if 9-cis retinoic acid (9-cis RA), the ligand for are the master regulators of lipid metabolism. Remarkably, a the heterodimeric partner of TR and LXR, RXR, could mouse with a targeted deletion of both LXRa and LXRb is regulate the hDIO2 promoter. Notably, 9-cis RA repressed resistant to western diet-induced obesity, and exhibits ectopic the hDIO2 luciferase reporter (1 mM, approximately four- liver expression of the thyroid hormone activating type 2 fold) in a dose-dependent manner, while coexpression of an deiodinase (D2). We hypothesized that LXR/retinoid inactive mutant RXR abolished this effect. However, it is X-receptor (RXR) signaling inhibits hepatic D2 expression, unlikely that RXR homodimers mediate the repression of and studied this using a luciferase reporter containing the hDIO2 since mutagenesis of a DR-1 at K506 bp did not human DIO2 (hDIO2) promoter in HepG2 cells.