Optimizing a Head-Tracked Stereo Display System to Guide Hepatic Tumor Ablation
Total Page:16
File Type:pdf, Size:1020Kb
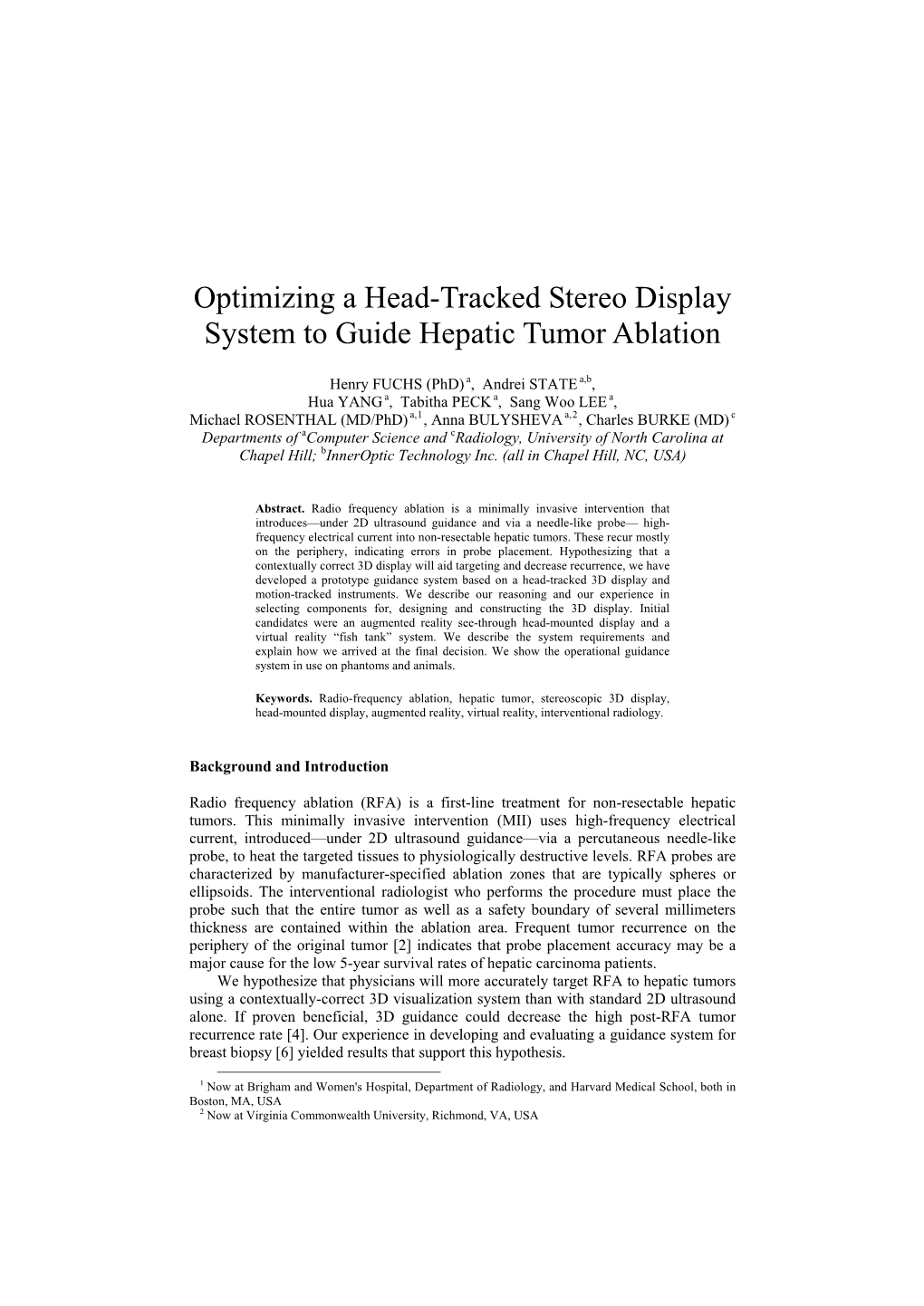
Load more
Recommended publications
-

Stereo Capture and Display At
Creation of a Complete Stereoscopic 3D Workflow for SoFA Allison Hettinger and Ian Krassner 1. Introduction 1.1 3D Trend Stereoscopic 3D motion pictures have recently risen to popularity once again following the success of films such as James Cameron’s Avatar. More and more films are being converted to 3D but few films are being shot in 3D. Current available technology and knowledge of that technology (along with cost) is preventing most films from being shot in 3D. Shooting in 3D is an advantage because two slightly different images are produced that mimic the two images the eyes see in normal vision. Many take the cheaper route of shooting in 2D and converting to 3D. This results in a 3D image, but usually nowhere near the quality as if the film was originally shot in 3D. This is because a computer has to create the second image, which can result in errors. It is also important to note that a 3D image does not necessarily mean a stereo image. 3D can be used to describe images that have an appearance of depth, such as 3D animations. Stereo images refer to images that make use of retinal disparity to create the illusion of objects going out of and into the screen plane. Stereo images are optical illusions that make use of several cues that the brain uses to perceive a scene. Examples of monocular cues are relative size and position, texture gradient, perspective and occlusion. These cues help us determine the relative depth positions of objects in an image. Binocular cues such as retinal disparity and convergence are what give the illusion of depth. -

Stereoscopic Vision, Stereoscope, Selection of Stereo Pair and Its Orientation
International Journal of Science and Research (IJSR) ISSN (Online): 2319-7064 Impact Factor (2012): 3.358 Stereoscopic Vision, Stereoscope, Selection of Stereo Pair and Its Orientation Sunita Devi Research Associate, Haryana Space Application Centre (HARSAC), Department of Science & Technology, Government of Haryana, CCS HAU Campus, Hisar – 125 004, India , Abstract: Stereoscope is to deflect normally converging lines of sight, so that each eye views a different image. For deriving maximum benefit from photographs they are normally studied stereoscopically. Instruments in use today for three dimensional studies of aerial photographs. If instead of looking at the original scene, we observe photos of that scene taken from two different viewpoints, we can under suitable conditions, obtain a three dimensional impression from the two dimensional photos. This impression may be very similar to the impression given by the original scene, but in practice this is rarely so. A pair of photograph taken from two cameras station but covering some common area constitutes and stereoscopic pair which when viewed in a certain manner gives an impression as if a three dimensional model of the common area is being seen. Keywords: Remote Sensing (RS), Aerial Photograph, Pocket or Lens Stereoscope, Mirror Stereoscope. Stereopair, Stere. pair’s orientation 1. Introduction characteristics. Two eyes must see two images, which are only slightly different in angle of view, orientation, colour, A stereoscope is a device for viewing a stereoscopic pair of brightness, shape and size. (Figure: 1) Human eyes, fixed on separate images, depicting left-eye and right-eye views of same object provide two points of observation which are the same scene, as a single three-dimensional image. -
Interacting with Autostereograms
See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/336204498 Interacting with Autostereograms Conference Paper · October 2019 DOI: 10.1145/3338286.3340141 CITATIONS READS 0 39 5 authors, including: William Delamare Pourang Irani Kochi University of Technology University of Manitoba 14 PUBLICATIONS 55 CITATIONS 184 PUBLICATIONS 2,641 CITATIONS SEE PROFILE SEE PROFILE Xiangshi Ren Kochi University of Technology 182 PUBLICATIONS 1,280 CITATIONS SEE PROFILE Some of the authors of this publication are also working on these related projects: Color Perception in Augmented Reality HMDs View project Collaboration Meets Interactive Spaces: A Springer Book View project All content following this page was uploaded by William Delamare on 21 October 2019. The user has requested enhancement of the downloaded file. Interacting with Autostereograms William Delamare∗ Junhyeok Kim Kochi University of Technology University of Waterloo Kochi, Japan Ontario, Canada University of Manitoba University of Manitoba Winnipeg, Canada Winnipeg, Canada [email protected] [email protected] Daichi Harada Pourang Irani Xiangshi Ren Kochi University of Technology University of Manitoba Kochi University of Technology Kochi, Japan Winnipeg, Canada Kochi, Japan [email protected] [email protected] [email protected] Figure 1: Illustrative examples using autostereograms. a) Password input. b) Wearable e-mail notification. c) Private space in collaborative conditions. d) 3D video game. e) Bar gamified special menu. Black elements represent the hidden 3D scene content. ABSTRACT practice. This learning effect transfers across display devices Autostereograms are 2D images that can reveal 3D content (smartphone to desktop screen). when viewed with a specific eye convergence, without using CCS CONCEPTS extra-apparatus. -

Multi-Perspective Stereoscopy from Light Fields
Multi-Perspective stereoscopy from light fields The MIT Faculty has made this article openly available. Please share how this access benefits you. Your story matters. Citation Changil Kim, Alexander Hornung, Simon Heinzle, Wojciech Matusik, and Markus Gross. 2011. Multi-perspective stereoscopy from light fields. ACM Trans. Graph. 30, 6, Article 190 (December 2011), 10 pages. As Published http://dx.doi.org/10.1145/2070781.2024224 Publisher Association for Computing Machinery (ACM) Version Author's final manuscript Citable link http://hdl.handle.net/1721.1/73503 Terms of Use Creative Commons Attribution-Noncommercial-Share Alike 3.0 Detailed Terms http://creativecommons.org/licenses/by-nc-sa/3.0/ Multi-Perspective Stereoscopy from Light Fields Changil Kim1,2 Alexander Hornung2 Simon Heinzle2 Wojciech Matusik2,3 Markus Gross1,2 1ETH Zurich 2Disney Research Zurich 3MIT CSAIL v u s c Disney Enterprises, Inc. Input Images 3D Light Field Multi-perspective Cuts Stereoscopic Output Figure 1: We propose a framework for flexible stereoscopic disparity manipulation and content post-production. Our method computes multi-perspective stereoscopic output images from a 3D light field that satisfy arbitrary prescribed disparity constraints. We achieve this by computing piecewise continuous cuts (shown in red) through the light field that enable per-pixel disparity control. In this particular example we employed gradient domain processing to emphasize the depth of the airplane while suppressing disparities in the rest of the scene. Abstract tions of autostereoscopic and multi-view autostereoscopic displays even glasses-free solutions become available to the consumer. This paper addresses stereoscopic view generation from a light field. We present a framework that allows for the generation However, the task of creating convincing yet perceptually pleasing of stereoscopic image pairs with per-pixel control over disparity, stereoscopic content remains difficult. -

Fast-Response Switchable Lens for 3D and Wearable Displays
Fast-response switchable lens for 3D and wearable displays Yun-Han Lee, Fenglin Peng, and Shin-Tson Wu* CREOL, The College of Optics and Photonics, University of Central Florida, Orlando, Florida 32816, USA *[email protected] Abstract: We report a switchable lens in which a twisted nematic (TN) liquid crystal cell is utilized to control the input polarization. Different polarization state leads to different path length in the proposed optical system, which in turn results in different focal length. This type of switchable lens has advantages in fast response time, low operation voltage, and inherently lower chromatic aberration. Using a pixelated TN panel, we can create depth information to the selected pixels and thus add depth information to a 2D image. By cascading three such device structures together, we can generate 8 different focuses for 3D displays, wearable virtual/augmented reality, and other head mounted display devices. ©2016 Optical Society of America OCIS codes: (230.3720) Liquid-crystal devices; (080.3620) Lens system design. References and links 1. O. Cakmakci and J. Rolland, “Head-worn displays: a review,” J. Display Technol. 2(3), 199–216 (2006). 2. B. Furht, Handbook of Augmented Reality (Springer, 2011). 3. H. Ren and S. T. Wu, Introduction to Adaptive Lenses (Wiley, 2012). 4. K. Akeley, S. J. Watt, A. R. Girshick, and M. S. Banks, “A stereo display prototype with multiple focal distances,” ACM Trans. Graph. 23(3), 804–813 (2004). 5. S. Liu and H. Hua, “A systematic method for designing depth-fused multi-focal plane three-dimensional displays,” Opt. Express 18(11), 11562–11573 (2010). -
STAR 1200 & 1200XL User Guide
STAR 1200 & 1200XL Augmented Reality Systems User Guide VUZIX CORPORATION VUZIX CORPORATION STAR 1200 & 1200XL – User Guide © 2012 Vuzix Corporation 2166 Brighton Henrietta Town Line Road Rochester, New York 14623 Phone: 585.359.5900 ! Fax: 585.359.4172 www.vuzix.com 2 1. STAR 1200 & 1200XL OVERVIEW ................................... 7! System Requirements & Compatibility .................................. 7! 2. INSTALLATION & SETUP .................................................. 14! Step 1: Accessory Installation .................................... 14! Step 2: Hardware Connections .................................. 15! Step 3: Adjustment ..................................................... 19! Step 4: Software Installation ...................................... 21! Step 5: Tracker Calibration ........................................ 24! 3. CONTROL BUTTON & ON SCREEN DISPLAY ..................... 27! VGA Controller .................................................................... 27! PowerPak+ Controller ......................................................... 29! OSD Display Options ........................................................... 30! 4. STAR HARDWARE ......................................................... 34! STAR Display ...................................................................... 34! Nose Bridge ......................................................................... 36! Focus Adjustment ................................................................ 37! Eye Separation ................................................................... -

A Novel Walk-Through 3D Display
A Novel Walk-through 3D Display Stephen DiVerdia, Ismo Rakkolainena & b, Tobias Höllerera, Alex Olwala & c a University of California at Santa Barbara, Santa Barbara, CA 93106, USA b FogScreen Inc., Tekniikantie 12, 02150 Espoo, Finland c Kungliga Tekniska Högskolan, 100 44 Stockholm, Sweden ABSTRACT We present a novel walk-through 3D display based on the patented FogScreen, an “immaterial” indoor 2D projection screen, which enables high-quality projected images in free space. We extend the basic 2D FogScreen setup in three ma- jor ways. First, we use head tracking to provide correct perspective rendering for a single user. Second, we add support for multiple types of stereoscopic imagery. Third, we present the front and back views of the graphics content on the two sides of the FogScreen, so that the viewer can cross the screen to see the content from the back. The result is a wall- sized, immaterial display that creates an engaging 3D visual. Keywords: Fog screen, display technology, walk-through, two-sided, 3D, stereoscopic, volumetric, tracking 1. INTRODUCTION Stereoscopic images have captivated a wide scientific, media and public interest for well over 100 years. The principle of stereoscopic images was invented by Wheatstone in 1838 [1]. The general public has been excited about 3D imagery since the 19th century – 3D movies and View-Master images in the 1950's, holograms in the 1960's, and 3D computer graphics and virtual reality today. Science fiction movies and books have also featured many 3D displays, including the popular Star Wars and Star Trek series. In addition to entertainment opportunities, 3D displays also have numerous ap- plications in scientific visualization, medical imaging, and telepresence. -

Investigating Intermittent Stereoscopy: Its Effects on Perception and Visual Fatigue
©2016 Society for Imaging Science and Technology DOI: 10.2352/ISSN.2470-1173.2016.5.SDA-041 INVESTIGATING INTERMITTENT STEREOSCOPY: ITS EFFECTS ON PERCEPTION AND VISUAL FATIGUE Ari A. Bouaniche, Laure Leroy; Laboratoire Paragraphe, Université Paris 8; Saint-Denis; France Abstract distance in virtual environments does not clearly indicate that the In a context in which virtual reality making use of S3D is use of binocular disparity yields a better performance, and a ubiquitous in certain industries, as well as the substantial amount cursory look at the literature concerning the viewing of of literature about the visual fatigue S3D causes, we wondered stereoscopic 3D (henceforth abbreviated S3D) content leaves little whether the presentation of intermittent S3D stimuli would lead to doubt as to some negative consequences on the visual system, at improved depth perception (over monoscopic) while reducing least for a certain part of the population. subjects’ visual asthenopia. In a between-subjects design, 60 While we do not question the utility of S3D and its use in individuals under 40 years old were tested in four different immersive environments in this paper, we aim to position conditions, with head-tracking enabled: two intermittent S3D ourselves from the point of view of user safety: if, for example, the conditions (Stereo @ beginning, Stereo @ end) and two control use of S3D is a given in a company setting, can an implementation conditions (Mono, Stereo). Several optometric variables were of intermittent horizontal disparities aid in depth perception (and measured pre- and post-experiment, and a subjective questionnaire therefore in task completion) while impacting the visual system assessing discomfort was administered. -

THE INFLUENCES of STEREOSCOPY on VISUAL ARTS Its History, Technique and Presence in the Artistic World
University of Art and Design Cluj-Napoca PhD THESIS SUMMARY THE INFLUENCES OF STEREOSCOPY ON VISUAL ARTS Its history, technique and presence in the artistic world PhD Student: Scientific coordinator: Nyiri Dalma Dorottya Prof. Univ. Dr. Ioan Sbârciu Cluj-Napoca 2019 1 CONTENTS General introduction ........................................................................................................................3 Chapter 1: HISTORY OF STEREOSCOPY ..............................................................................4 1.1 The theories of Euclid and the experiments of Baptista Porta .........................................5 1.2 Leonardo da Vinci and Francois Aguillon (Aguilonius) .................................................8 1.3 The Inventions of Sir Charles Wheatstone and Elliot ...................................................18 1.4 Sir David Brewster's contributions to the perfection of the stereoscope .......................21 1.5 Oliver Wendell Holmes, the poet of stereoscopy ..........................................................23 1.6 Apex of stereoscopy .......................................................................................................26 1.7 Underwood & Keystone .................................................................................................29 1.8 Favorite topics in stereoscopy ........................................................................................32 1.8.1 Genre Scenes33 .........................................................................................................33 -
2018 First Call for Papers4 2013+First+Call+For+Papers+V4.Qxd
FIRST CALL FOR PAPERS Display Week 2018 Society for Information Display INTERNATIONAL SYMPOSIUM, SEMINAR & EXHIBITION May 20 – 25, 2018 LOS ANGELES CONVENTION CENTER LOS ANGELES, CALIFORNIA, USA www.displayweek.org • Photoluminescence and Applications – Using quantum Special Topics for 2018 nanomaterials for color-conversion applications in display components and in pixel-integrated configurations. Optimizing performance and stability for integration on- The Display Week 2018 Technical Symposium will chip (inside LED package) and in remote phosphor be placing special emphasis on four Special Topics configurations for backlight units. of Interest to address the rapid growth of the field of • Micro Inorganic LEDs and Applications – Emerging information display in the following areas: Augmented technologies based on scaling down inorganic LEDs for Reality, Virtual Reality, and Artificial Intelligence; use as arrayed emitters in display applications, with Quantum Dots and Micro-LEDs; and Wearable opportunities from large video displays down to high Displays, Sensors, and Devices. Submissions relating resolution microdisplays. Science and technology of to these special topics are highly encouraged. micro LED devices, materials, and processes for the fabrication and integration with electronic drive back- 1. AUGMENTED REALITY, VIRTUAL REALITY, AND planes. Color generation, performance, and stability. ARTIFICIAL INTELLIGENCE (AR, VR, AND AI) Packaging and module assembly solutions for emerging This special topic will cover the technologies and -

Digital 3DTV
Digital 3DTV Alexey Polyakov The advent of the digital 3DTV era is a fait accompli. The question is: how is it going to develop in the future? Currently the Standard definition(SD) TV is being changed into High definition(HD) TV. As you know, quantitative changes tend to transform into qualitative ones. Many observers believe that the next quantum leap will be the emergence of 3D TV. They predict that such TV will appear within a decade. In this article I will explain how it is possible to create stereoscopic video systems using commercial devices. Brief historical retrospective The following important stages can be singled out in the history of TV and digital video development: 1—black and white TV – image brightness is transmitted. 2 – colored TV – image brightness and color components are transmitted. From the data volume perspective, adding color is a quantitative change. From the viewer perspective, it is a qualitative change. 3 – digital video emergence (Video CD, DVD) – a qualitative change from the data format perspective. 4 – HD digital video and TV (Blu-Ray, HDTV) – from the data volume perspectiveit is a quantitative change. However, exactly the same components are transmitted: brightness and color. Specialists and viewers have been anticipating for the change that had been predicted by sci-fi writers long ago, - 3D TV emergency. For a long time data volume was a bottleneck preventing stereoscopic video demonstration as the existing media couldn’t transmit it. Digital TV enabled to transmit enough data and became the basis for a number of devices that helped to realize 3D visualization. -

The Role of Focus Cues in Stereopsis, and the Development of a Novel Volumetric Display
The role of focus cues in stereopsis, and the development of a novel volumetric display by David Morris Hoffman A dissertation submitted in partial satisfaction of the requirements for the degree of Doctor of Philosophy in Vision Science in the GRADUATE DIVISION of the UNIVERSITY OF CALIFORNIA, BERKELEY Committee in charge: Professor Martin S. Banks, Chair Professor Austin Roorda Professor John Canny Spring 2010 1 Abstract The role of focus cues in stereopsis, and the development of a novel volumetric display by David Morris Hoffman Doctor of Philosophy in Vision Science University of California, Berkeley Professor Martin S. Banks, Chair Typical stereoscopic displays produce a vivid impression of depth by presenting each eye with its own image on a flat display screen. This technique produces many depth signals (including disparity) that are consistent with a 3-dimensional (3d) scene; however, by using a flat display panel, focus information will be incorrect. The accommodation distance to the simulated objects will be at the screen distance, and blur will be inconsistent with the simulated depth. In this thesis I will described several studies investigating the importance of focus cues for binocular vision. These studies reveal that there are a number of benefits to presenting correct focus information in a stereoscopic display, such as making it easier to fuse a binocular image, reducing visual fatigue, mitigating disparity scaling errors, and helping to resolve the binocular correspondence problem. For each of these problems, I discuss the theory for how focus cues could be an important factor, and then present psychophysical data showing that indeed focus cues do make a difference.