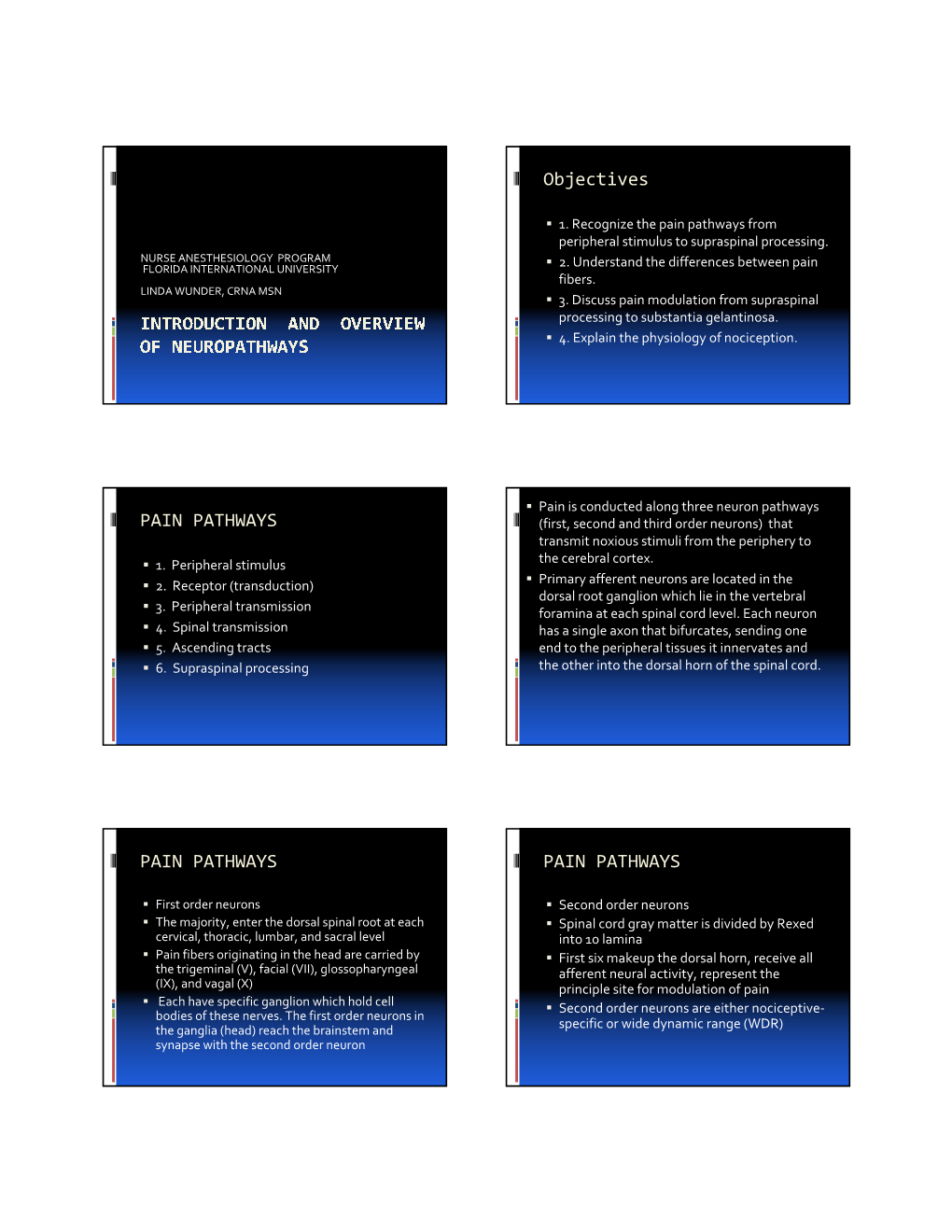
Objectives PAIN PATHWAYS PAIN PATHWAYS PAIN PATHWAYS
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Nerve Lesion in the Carpal Tunnel Syndrome
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.39.7.615 on 1 July 1976. Downloaded from Journal of Neurology, Neurosurgery, and Psychiatry, 1976, 39, 615-626 The nerve lesion in the carpal tunnel syndrome SYDNEY SUNDERLAND From the Department of Experimental Neurology, University of Melbourne, Parkville, Victoria, Australia SYNOPSIS The relative roles of pressure deformation and ischaemia in the production of compres- sion nerve lesions remain a controversial issue. This paper concerns the genesis of the structural changes which follow compression of the median nerve in the carpal tunnel. The initial lesion is an intrafunicular anoxia caused by obstruction to the venous return from the funiculi as the result of increased pressure in the tunnel. This leads to intrafunicular oedema and an increase in intrafunicular pressure which imperil and finally destroy nerve fibres by impairing their blood supply and by compression. The final outcome is the fibrous tissue replacement of the contents of the funiculi. Protected by copyright. In 1862 Waller described the motor, vasomotor, (Gasser, 1935; Allen, 1938; Bentley and Schlapp, and sensory changes which followed the com- 1943; Richards, 1951; Moldaver, 1954; Gelfan pression of nerves in his own arm. His account and Tarlov, 1956). carried no reference to the mechanism In the 1940s Weiss and his associates (Weiss, responsible for blocking conduction in the nerve 1943, 1944; Weiss and Davis, 1943; Weiss and fibres, presumably because he regarded it as Hiscoe, 1948), who were primarily concerned obvious that pressure was the offending agent. with the technical problem of uniting severed Interest in the effects of nerve compression nerves, observed that a divided nerve enclosed was not renewed until the 1920s when cuff or in a tightly fitting arterial sleeve became swollen tourniquet compression was used to produce a proximal and distal to the constriction. -

Deconstructing Spinal Interneurons, One Cell Type at a Time Mariano Ignacio Gabitto
Deconstructing spinal interneurons, one cell type at a time Mariano Ignacio Gabitto Submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy under the Executive Committee of the Graduate School of Arts and Sciences COLUMBIA UNIVERSITY 2016 © 2016 Mariano Ignacio Gabitto All rights reserved ABSTRACT Deconstructing spinal interneurons, one cell type at a time Mariano Ignacio Gabitto Abstract Documenting the extent of cellular diversity is a critical step in defining the functional organization of the nervous system. In this context, we sought to develop statistical methods capable of revealing underlying cellular diversity given incomplete data sampling - a common problem in biological systems, where complete descriptions of cellular characteristics are rarely available. We devised a sparse Bayesian framework that infers cell type diversity from partial or incomplete transcription factor expression data. This framework appropriately handles estimation uncertainty, can incorporate multiple cellular characteristics, and can be used to optimize experimental design. We applied this framework to characterize a cardinal inhibitory population in the spinal cord. Animals generate movement by engaging spinal circuits that direct precise sequences of muscle contraction, but the identity and organizational logic of local interneurons that lie at the core of these circuits remain unresolved. By using our Sparse Bayesian approach, we showed that V1 interneurons, a major inhibitory population that controls motor output, fractionate into diverse subsets on the basis of the expression of nineteen transcription factors. Transcriptionally defined subsets exhibit highly structured spatial distributions with mediolateral and dorsoventral positional biases. These distinctions in settling position are largely predictive of patterns of input from sensory and motor neurons, arguing that settling position is a determinant of inhibitory microcircuit organization. -

Spinal Cord Organization
Lecture 4 Spinal Cord Organization The spinal cord . Afferent tract • connects with spinal nerves, through afferent BRAIN neuron & efferent axons in spinal roots; reflex receptor interneuron • communicates with the brain, by means of cell ascending and descending pathways that body form tracts in spinal white matter; and white matter muscle • gives rise to spinal reflexes, pre-determined gray matter Efferent neuron by interneuronal circuits. Spinal Cord Section Gross anatomy of the spinal cord: The spinal cord is a cylinder of CNS. The spinal cord exhibits subtle cervical and lumbar (lumbosacral) enlargements produced by extra neurons in segments that innervate limbs. The region of spinal cord caudal to the lumbar enlargement is conus medullaris. Caudal to this, a terminal filament of (nonfunctional) glial tissue extends into the tail. terminal filament lumbar enlargement conus medullaris cervical enlargement A spinal cord segment = a portion of spinal cord that spinal ganglion gives rise to a pair (right & left) of spinal nerves. Each spinal dorsal nerve is attached to the spinal cord by means of dorsal and spinal ventral roots composed of rootlets. Spinal segments, spinal root (rootlets) nerve roots, and spinal nerves are all identified numerically by th region, e.g., 6 cervical (C6) spinal segment. ventral Sacral and caudal spinal roots (surrounding the conus root medullaris and terminal filament and streaming caudally to (rootlets) reach corresponding intervertebral foramina) collectively constitute the cauda equina. Both the spinal cord (CNS) and spinal roots (PNS) are enveloped by meninges within the vertebral canal. Spinal nerves (which are formed in intervertebral foramina) are covered by connective tissue (epineurium, perineurium, & endoneurium) rather than meninges. -

Nerve and Nerve Injuries” Sunderland : 50 Years Later
2019 Nerve and Nerve Injuries” Sunderland : 50 years later Faye Chiou Tan, MD Professor, Dir. EDX, H. Ben Taub PMR, Baylor College of Medicine Chief PMR, Dir. EDX, Harris Health System 2019 Financial Disclosure • Elsevier Book Royalties for “EMG Secrets” textbook • Revance, consultation panel 2019 Warning Videotaping or taking pictures of the slides associated with this presentation is prohibited. The information on the slides is copyrighted and cannot be used without permission and author attribution. Introduction – Sydney Sunderland was Professor of Experimental Neurology at the University of Melbourne. – His textbook “Nerve and Nerve lnjuries” published in 1968 is no longer in print (copies $1000 on the internet) – Here is a review as relates to new technology: Ultrahigh frequency musculoskeletal ultrasound Part I – I. Anatomic and physiologic features of A. Peripheral nerve fibers B. Peripheral nerve trunks I.A. Peripheral nerve fibers – Axoplasm – Increased flow of cytoplasm from cell body into axons during electrical stimulation (Grande and Richter 1950) – Although overall proximal to distal axoplasmic flow, the pattern of streaming in the axon is bidirectional and faster (up to 3-7 cm/day) (Lubinska 1964). I. A. Peripheral nerve fibers – Sheath – Myelinated – Length of internode elongates with growth (Vizoso and Young 1948, Siminoff 1965) – In contrast, remyelination in adults produce short internodes of same length (Leegarrd 1880, Young 1945,…) – Incisures of Schmidt-Lantermann are clefts conical clefts that open when a nerve trunk is stretched thereby preventing distortion of myelin. (Glees, 1943) Schmidt-Lantermann Clefts Sunderland S. Nerve and Nerve Injuries, Sunderland, Livingstone,LTD, Edinburgh/London, 1968, p. 8 I. A. -

Review of Spinal Cord Basics of Neuroanatomy Brain Meninges
Review of Spinal Cord with Basics of Neuroanatomy Brain Meninges Prof. D.H. Pauža Parts of Nervous System Review of Spinal Cord with Basics of Neuroanatomy Brain Meninges Prof. D.H. Pauža Neurons and Neuroglia Neuron Human brain contains per 1011-12 (trillions) neurons Body (soma) Perikaryon Nissl substance or Tigroid Dendrites Axon Myelin Terminals Synapses Neuronal types Unipolar, pseudounipolar, bipolar, multipolar Afferent (sensory, centripetal) Efferent (motor, centrifugal, effector) Associate (interneurons) Synapse Presynaptic membrane Postsynaptic membrane, receptors Synaptic cleft Synaptic vesicles, neuromediator Mitochondria In human brain – neurons 1011 (100 trillions) Synapses – 1015 (quadrillions) Neuromediators •Acetylcholine •Noradrenaline •Serotonin •GABA •Endorphin •Encephalin •P substance •Neuronal nitric oxide Adrenergic nerve ending. There are many 50-nm-diameter vesicles (arrow) with dark, electron-dense cores containing norepinephrine. x40,000. Cell Types of Neuroglia Astrocytes - Oligodendrocytes – Ependimocytes - Microglia Astrocytes – a part of hemoencephalic barrier Oligodendrocytes Ependimocytes and microglial cells Microglia represent the endogenous brain defense and immune system, which is responsible for CNS protection against various types of pathogenic factors. After invading the CNS, microglial precursors disseminate relatively homogeneously throughout the neural tissue and acquire a specific phenotype, which clearly distinguish them from their precursors, the blood-derived monocytes. The ´resting´ microglia -

High-Yield Neuroanatomy, FOURTH EDITION
LWBK110-3895G-FM[i-xviii].qxd 8/14/08 5:57 AM Page i Aptara Inc. High-Yield TM Neuroanatomy FOURTH EDITION LWBK110-3895G-FM[i-xviii].qxd 8/14/08 5:57 AM Page ii Aptara Inc. LWBK110-3895G-FM[i-xviii].qxd 8/14/08 5:57 AM Page iii Aptara Inc. High-Yield TM Neuroanatomy FOURTH EDITION James D. Fix, PhD Professor Emeritus of Anatomy Marshall University School of Medicine Huntington, West Virginia With Contributions by Jennifer K. Brueckner, PhD Associate Professor Assistant Dean for Student Affairs Department of Anatomy and Neurobiology University of Kentucky College of Medicine Lexington, Kentucky LWBK110-3895G-FM[i-xviii].qxd 8/14/08 5:57 AM Page iv Aptara Inc. Acquisitions Editor: Crystal Taylor Managing Editor: Kelley Squazzo Marketing Manager: Emilie Moyer Designer: Terry Mallon Compositor: Aptara Fourth Edition Copyright © 2009, 2005, 2000, 1995 Lippincott Williams & Wilkins, a Wolters Kluwer business. 351 West Camden Street 530 Walnut Street Baltimore, MD 21201 Philadelphia, PA 19106 Printed in the United States of America. All rights reserved. This book is protected by copyright. No part of this book may be reproduced or transmitted in any form or by any means, including as photocopies or scanned-in or other electronic copies, or utilized by any information storage and retrieval system without written permission from the copyright owner, except for brief quotations embodied in critical articles and reviews. Materials appearing in this book prepared by individuals as part of their official duties as U.S. government employees are not covered by the above-mentioned copyright. To request permission, please contact Lippincott Williams & Wilkins at 530 Walnut Street, Philadelphia, PA 19106, via email at [email protected], or via website at http://www.lww.com (products and services). -

Functional Studies of Descending Sympathetic Pathways in the Spinal Cord
Loyola University Chicago Loyola eCommons Dissertations Theses and Dissertations 1973 Functional Studies of Descending Sympathetic Pathways in the Spinal Cord Robert Dale Foreman Loyola University Chicago Follow this and additional works at: https://ecommons.luc.edu/luc_diss Recommended Citation Foreman, Robert Dale, "Functional Studies of Descending Sympathetic Pathways in the Spinal Cord" (1973). Dissertations. 1326. https://ecommons.luc.edu/luc_diss/1326 This Dissertation is brought to you for free and open access by the Theses and Dissertations at Loyola eCommons. It has been accepted for inclusion in Dissertations by an authorized administrator of Loyola eCommons. For more information, please contact [email protected]. This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 3.0 License. Copyright © 1973 Robert Dale Foreman FUNCTIONAL STUDIES OF DESCENDING SYMPATHEI'IC PATHWAYS IN THE SPDIAL CORD by Robert Dale Foreman A Disaertation Submitted to the Faculty of the Graduate School of Loyola University in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy June 1973 ·L l , Univers:t·J ,_~_cdi,a1 Center [ 10rary - oyo1a · Dedicated to my parents- Dad and Mom Foreman ii :BIOGRAPHY Robert D. Foreman was born on April 27, 1946, at Orange City, Iowa. He was raised on a farm near Montevideo, Minnesota and attended a small country school during his elementary school years. After moving back to Orange City, Iowa, he attended Western Christian High School at Hull, Iowa. :Before his college career began, he worked one year as a con struction worker in Artesia, California and later as a truck driver for a paint company in Orange City, Iowa. -

Nerve Injury: Anatomy and Definitions J
EQUINE VETERINARY EDUCATION / AE / january 2011 17 Clinical Commentaryeve_156 17..18 Nerve injury: Anatomy and definitions J. Peroni University of Georgia, Large Animal Medicine, 501 DW Brooks Drive College of Veterinary Medicine, College of Veterinary Medicine, Athens, USA. Nerve injury: anatomy and definitions Schwann cells. There are points along the axon called nodes of Ranvier at which the myelin sheath is Although the neuropathy in the horse in the report by discontinued. These nodes are sites at which ions are easily Ljungvall and Jonsson (2010) in this issue is an interesting exchanged between the nerve and the extracellular and unique cause of lameness, nerve trauma is generally matrix, a process impeded along the rest of the axon by uncommon in horses. Knowledge of the anatomy of the the insulating property of myelin sheath. Depolarisation of peripheral nerve fibre may be helpful in understanding the axon occurring at the nodes of Ranvier creates the nerve injury and restoration of nerve function. action potential responsible for the so-called saltatory (jump) neural conduction. Anatomy Nerves can be damaged as a result of trauma and lacerations and during invasive surgical procedures in which Most peripheral nerves are a collection of myelinated and the landmarks are obscured by abnormal tissues (Colohan unmyelinated neural fibres (axons) enclosed within a highly et al. 1996; Cornwall and Radomisli 2000; Trumble 2000). elastic connective tissue sheath called the epineurium. Equine surgeons electively transect the palmar digital nerves Bundles of nerve fibres contained within the epineurium in an attempt to eliminate pain arising from conditions are often referred to as fasciculi, which are comprised of localised within the caudal portion of the hoof that otherwise smaller neural fibres called funiculi. -

The Spinal Cord and Spinal Nerves
14 The Nervous System: The Spinal Cord and Spinal Nerves PowerPoint® Lecture Presentations prepared by Steven Bassett Southeast Community College Lincoln, Nebraska © 2012 Pearson Education, Inc. Introduction • The Central Nervous System (CNS) consists of: • The spinal cord • Integrates and processes information • Can function with the brain • Can function independently of the brain • The brain • Integrates and processes information • Can function with the spinal cord • Can function independently of the spinal cord © 2012 Pearson Education, Inc. Gross Anatomy of the Spinal Cord • Features of the Spinal Cord • 45 cm in length • Passes through the foramen magnum • Extends from the brain to L1 • Consists of: • Cervical region • Thoracic region • Lumbar region • Sacral region • Coccygeal region © 2012 Pearson Education, Inc. Gross Anatomy of the Spinal Cord • Features of the Spinal Cord • Consists of (continued): • Cervical enlargement • Lumbosacral enlargement • Conus medullaris • Cauda equina • Filum terminale: becomes a component of the coccygeal ligament • Posterior and anterior median sulci © 2012 Pearson Education, Inc. Figure 14.1a Gross Anatomy of the Spinal Cord C1 C2 Cervical spinal C3 nerves C4 C5 C 6 Cervical C 7 enlargement C8 T1 T2 T3 T4 T5 T6 T7 Thoracic T8 spinal Posterior nerves T9 median sulcus T10 Lumbosacral T11 enlargement T12 L Conus 1 medullaris L2 Lumbar L3 Inferior spinal tip of nerves spinal cord L4 Cauda equina L5 S1 Sacral spinal S nerves 2 S3 S4 S5 Coccygeal Filum terminale nerve (Co1) (in coccygeal ligament) Superficial anatomy and orientation of the adult spinal cord. The numbers to the left identify the spinal nerves and indicate where the nerve roots leave the vertebral canal. -

Neuroanatomy of the Spinal Cord: Current Research and Future Prospects
Paraplegia 25 (1987) 198-204 © 1987 International Medical Society of Paraplegia Neuroanatomy of the Spinal Cord: Current Research and Future Prospects J. V. Priestley, D.Phil. Departments of Physiology and Biochemistry, United Medical and Dental Schools, St Thomas' Campus, London SEI 7EH, England Introduction In this article my brief is to provide a succinct state of the art commentary on the neuroanatomy of the spinal cord. This is a fieldin which major developments in methodology are providing important information on the neuronal circuitry of the spinal cord and this work complements our existing knowledge of its basic structure and pathways. One of the most interesting areas of development has been in the application of neuroanatomy in combination with physiology and neurochemistry in order to provide a correlation between structure and function. In this article I will focus on three different but related areas to illustrate some of the current trends and future prospects for basic research on spinal cord neuroanatomy. Spinal cord circuitry and connections Much recent anatomical work has focused on the use of anterograde and retro grade axonal transport of specific tracers in order to examine neuronal pathways within the spinal cord. This approach gives detailed information on the exact location of the cells of origin of specific pathways and on the distribution of their terminals. The information obtained generally agrees with the results of earlier studies but provides more detail and may detect new pathways. For example, anterograde tracer studies have identified terminations of descending bulbospinal pathways in the superficial dorsal horn and in ventral horn moto neuronal cell groups (Kuypers and Huisman, 1982). -
Nervous System : Sylabus for Foreign Students
Department of Histology and Embryology, P. J. Šafárik University, Medical Faculty, Košice Nervous system : Sylabus for foreign students Author: Prof. MUDr. Eva Mechírová, CSc. NERVOUS SYSTEM 1.Central nervous system – brain, spinal cord 2. Peripheral nervous system – ganglia, peripheral nerves, peripheral nerve endings Central nervous system (CNS) gray matter – substantia grisea: nerve cells and neuroglial cells- protoplasmic astrocytes, microglia; neuropil - axons, dendrites, synapses, neuroglial processes; capillaries white matter – substantia alba: myelinated axons and neuroglia – oligodenrocytes, fibrilar astrocytes, microglia; capillaries gray matter - on the surface of the brain and cerebellum- cortex white matter – on the surface of the spinal cord Within the CNS, specific terms are used to describe arrangement of nerve cells and their connections: ● cortex - arrangement of neurons over the surface of the brain and cerebellum ● nuclei - clusters of neuron bodies forming islands of gray matter embedded in white matter ● column or horn - arrangement of neurons within the spinal cord ● funiculus or fascicle - bundle of axons running in white matter On the basis of phylogenetic development and microscopic structure, the following two types of cerebral cortices are recognized – Allocortex and Neocortex. Neocortex or isocortex This cortex is six layered and comprises 95% of the cerebral cortex on the surface of hemispheres in humans. Isocortex in which six layers are clearly evident (primary sensory cortex) is termed homotypical cortex. Isocortex in which some of the six layers are obscured (motor or visual cortex) is termed heterotypical cortex. CEREBELLUM ARBOR VITAE Cytoarchitecture of the cerebellar cortex Medulla spinalis - spinal cord 1. Cervical – 8 segments 2. Thoracic – 12 segments 3. Lumbar – 5 segments 4. -

The Changes in Human Spinal Sympathetic Preganglionic Neurons After Spinal Cord Injury
Spinal Cord (1999) 37, 6±13 ã 1999 International Medical Society of Paraplegia All rights reserved 1362 ± 4393/99 $12.00 http://www.stockton-press.co.uk/sc The changes in human spinal sympathetic preganglionic neurons after spinal cord injury AV Krassioukov1, RP Bunge2, WR Pucket2 and MA Bygrave1 1The Neurodegeneration Research Group, The JP Robarts Research Institute, The Department of Physiology of the University of Western Ontario, 100 Perth Drive, PO Box 5015, London, Ontario, Canada; 2The Miami Project to Cure Paralysis, University of Miami School of Medicine, Miami, Florida 33136, USA We have applied conventional histochemical, immunocytochemical and morphometric techniques to study the changes within the human spinal sympathetic preganglionic neurons (SPNs) after spinal cord injury. SPNs are localized within the intermediolateral nucleus (IML) of the lateral horn at the thoraco-lumbar level of the spinal cord and are the major contributors to central cardiovascular control. SPNs in dierent thoracic segments in the normal spinal cord were similar in soma size. SPNs in the IML were also identi®ed using immunoreactivity to choline acetyltransferase. Soma area of SPNs was 400.7+15 mm2 and 409.9+22 mm2 at the upper thoracic (T3) and middle thoracic (T7) segments, respectively. In the spinal cord obtained from a person who survived for 2 weeks following a spinal cord injury at T5, we found a signi®cant decrease in soma area of the SPNs in the segments below the site of injury: soma area of SPNs at T8 was 272.9+11 mm2. At T1 the soma area was 418+19 mm2.