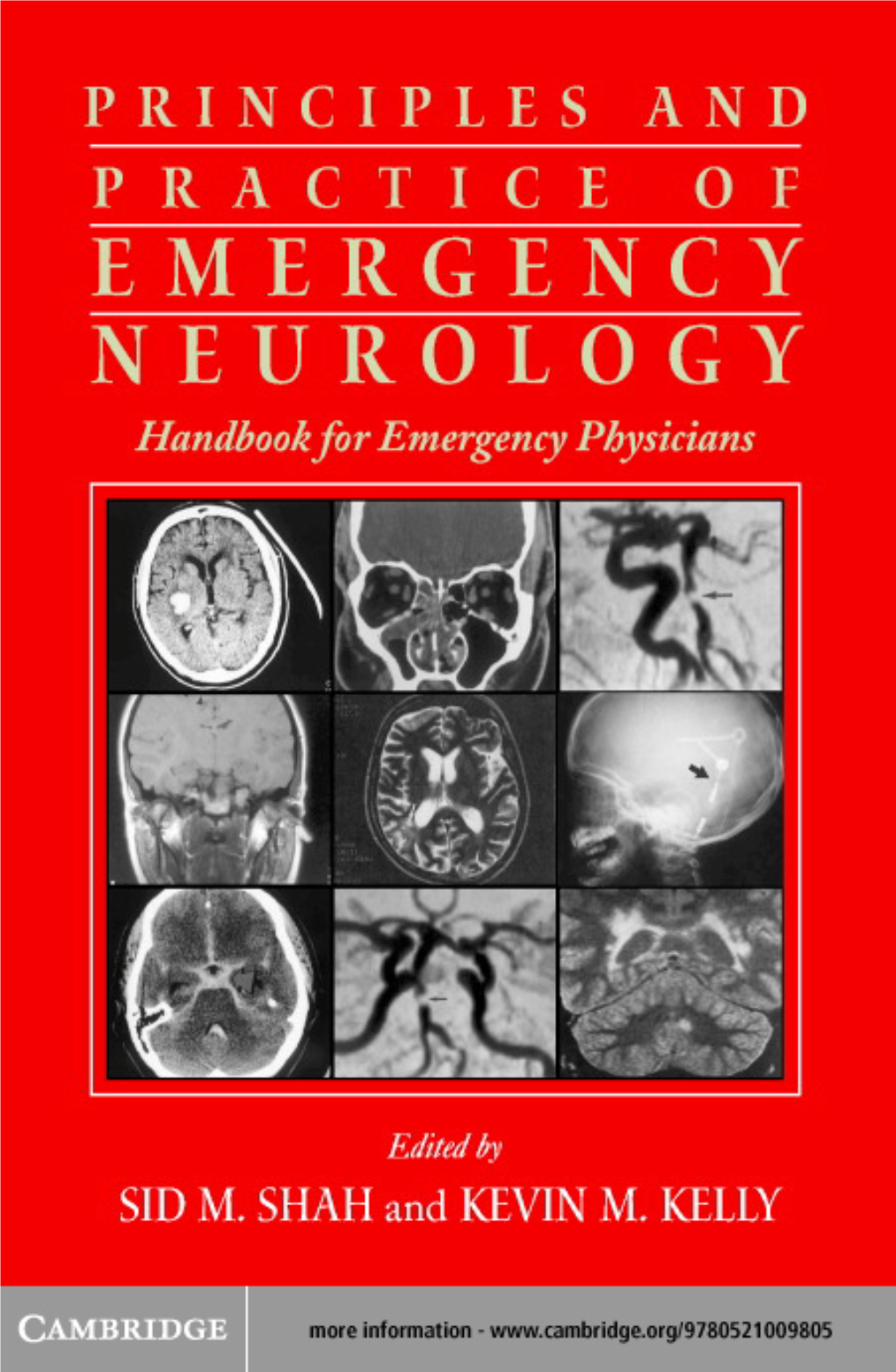
Sid M. Shah.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Detection of Focal Cerebral Hemisphere Lesions Using the Neurological Examination N E Anderson, D F Mason, J N Fink, P S Bergin, a J Charleston, G D Gamble
545 J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.2004.043679 on 16 March 2005. Downloaded from PAPER Detection of focal cerebral hemisphere lesions using the neurological examination N E Anderson, D F Mason, J N Fink, P S Bergin, A J Charleston, G D Gamble ............................................................................................................................... J Neurol Neurosurg Psychiatry 2005;76:545–549. doi: 10.1136/jnnp.2004.043679 Objective: To determine the sensitivity and specificity of clinical tests for detecting focal lesions in a prospective blinded study. Methods: 46 patients with a focal cerebral hemisphere lesion without obvious focal signs and 19 controls with normal imaging were examined using a battery of clinical tests. Examiners were blinded to the diagnosis. The sensitivity, specificity, and positive and negative predictive values of each test were measured. See end of article for authors’ affiliations Results: The upper limb tests with the greatest sensitivities for detecting a focal lesion were finger rolling ....................... (sensitivity 0.33 (95% confidence interval, 0.21 to 0.47)), assessment of power (0.30 (0.19 to 0.45)), rapid alternating movements (0.30 (0.19 to 0.45)), forearm rolling (0.24 (0.14 to 0.38)), and pronator Correspondence to: Dr Neil Anderson, drift (0.22 (0.12 to 0.36)). All these tests had a specificity of 1.00 (0.83 to 1.00). This combination of tests Department of Neurology, detected an abnormality in 50% of the patients with a focal lesion. In the lower limbs, assessment of power Auckland Hospital, Private was the most sensitive test (sensitivity 0.20 (0.11 to 0.33)). -

(Kir) Channels in Tick Salivary Gland Function Zhilin Li Louisiana State University and Agricultural and Mechanical College, [email protected]
Louisiana State University LSU Digital Commons LSU Master's Theses Graduate School 3-26-2018 Characterizing the Physiological Role of Inward Rectifier Potassium (Kir) Channels in Tick Salivary Gland Function Zhilin Li Louisiana State University and Agricultural and Mechanical College, [email protected] Follow this and additional works at: https://digitalcommons.lsu.edu/gradschool_theses Part of the Entomology Commons Recommended Citation Li, Zhilin, "Characterizing the Physiological Role of Inward Rectifier Potassium (Kir) Channels in Tick Salivary Gland Function" (2018). LSU Master's Theses. 4638. https://digitalcommons.lsu.edu/gradschool_theses/4638 This Thesis is brought to you for free and open access by the Graduate School at LSU Digital Commons. It has been accepted for inclusion in LSU Master's Theses by an authorized graduate school editor of LSU Digital Commons. For more information, please contact [email protected]. CHARACTERIZING THE PHYSIOLOGICAL ROLE OF INWARD RECTIFIER POTASSIUM (KIR) CHANNELS IN TICK SALIVARY GLAND FUNCTION A Thesis Submitted to the Graduate Faculty of the Louisiana State University and Agricultural and Mechanical College in partial fulfillment of the requirements for the degree of Master of Science in The Department of Entomology by Zhilin Li B.S., Northwest A&F University, 2014 May 2018 Acknowledgements I would like to thank my family (Mom, Dad, Jialu and Runmo) for their support to my decision, so I can come to LSU and study for my degree. I would also thank Dr. Daniel Swale for offering me this awesome opportunity to step into toxicology filed, ask scientific questions and do fantastic research. I sincerely appreciate all the support and friendship from Dr. -

A Neurological Examination
THE 3 MINUTE NEUROLOGICAL EXAMINATION DEMYSTIFIED Faculty: W.J. Oczkowski MD, FRCPC Professor and Academic Head, Division of Neurology, Department of Medicine, McMaster University Stroke Neurologist, Hamilton Health Sciences Relationships with commercial interests: ► Not Applicable Potential for conflict(s) of interest: ► Not Applicable Mitigating Potential Bias ► All the recommendations involving clinical medicine are based on evidence that is accepted within the profession. ► All scientific research referred to, reported, or used is in the support or justification of patient care. ► Recommendations conform to the generally accepted standards. ► Independent content validation. ► The presentation will mitigate potential bias by ensuring that data and recommendations are presented in a fair and balanced way. ► Potential bias will be mitigated by presenting a full range of products that can be used in this therapeutic area. ► Information of the history, development, funding, and the sponsoring organizations of the disclosure presented will be discussed. Objectives ► Overview of neurological assessment . It’s all about stroke! . It’s all about the chief complaint and history. ► Overview: . 3 types of clinical exams . Neurological signs . Neurological localization o Pathognomonic signs o Upper versus lower motor neuron signs ► Cases and practice Bill ► 72 year old male . Hypertension . Smoker ► Stroke call: dizzy, facial droop, slurred speech ► Neurological Exam: . Ptosis and miosis on left . Numb left face . Left palatal weakness . Dysarthria . Ataxic left arm and left leg . Numb right arm and leg NIH Stroke Scale Score ► LOC: a,b,c_________________ 0 ► Best gaze__________________ 0 0 ► Visual fields________________ 0 ► Facial palsy________________ 0 ► Motor arm and leg__________ -Left Ptosis 2 -Left miosis ► Limb ataxia________________ -Weakness of 1 ► Sensory_______________________ left palate ► Best Language______________ 0 1 ► Dysarthria_________________ 0 ► Extinction and inattention____ - . -

Statin Myopathy: a Common Dilemma Not Reflected in Clinical Trials
REVIEW CME EDUCATIONAL OBJECTIVE: Readers will assess possible statin-induced myopathy in their patients on statins CREDIT GENARO FERNANDEZ, MD ERICA S. SPATZ, MD CHARLES JABLECKI, MD PAUL S. PHILLIPS, MD Internal Medicine Residency Program, Robert Wood Johnson Clinical Scholars Department of Neurosciences, University Director, Interventional Cardiology, The University of Utah, Salt Lake City Program, Cardiovascular Disease Fellow, of California San Diego, La Jolla Department of Cardiology, Scripps Mercy Yale University School of Medicine, New Hospital, San Diego, CA Haven, CT Statin myopathy: A common dilemma not reflected in clinical trials ■■ ABSTRACT hen a patient taking a statin complains Wof muscle aches, is he or she experiencing Although statins are remarkably effective, they are still statin-induced myopathy or some other prob- underprescribed because of concerns about muscle toxic- lem? Should statin therapy be discontinued? Statins have proven efficacy in preventing ity. We review the aspects of statin myopathy that are 1 important to the primary care physician and provide a heart attacks and death, and they are the most guide for evaluating patients on statins who present with widely prescribed drugs worldwide. Neverthe- less, they remain underused, with only 50% of muscle complaints. We outline the differential diagnosis, those who would benefit from being on a statin the risks and benefits of statin therapy in patients with receiving one.2,3 In addition, at least 25% of possible toxicity, and the subsequent treatment options. adults who start taking statins stop taking them 4 ■■ by 6 months, and up to 60% stop by 2 years. KEY POINTS Patient and physician fears about myopathy There is little consensus on the definition of statin-in- remain a key reason for stopping. -

Serial Tap Test of Patients with Idiopathic Normal Pressure
da Rocha et al. Fluids Barriers CNS (2021) 18:22 https://doi.org/10.1186/s12987-021-00254-3 Fluids and Barriers of the CNS RESEARCH Open Access Serial Tap Test of patients with idiopathic normal pressure hydrocephalus: impact on cognitive function and its meaning Samanta Fabrício Blattes da Rocha1* , Pedro André Kowacs1,2, Ricardo Krause Martinez de Souza1, Matheus Kahakura Franco Pedro1, Ricardo Ramina1 and Hélio A. Ghizoni Teive3 Abstract Background: Idiopathic normal pressure hydrocephalus (INPH) is characterized by gait disturbance, urinary incon- tinence and cognitive decline. Symptoms are potentially reversible and treatment is based on cerebrospinal fuid shunting. The tap test (TT) is used to identify patients that will beneft from surgery. This procedure consists of the withdrawal of 20 to 50 mL of cerebrospinal fuid (CSF) through a lumbar puncture (LP) after which the symptoms of the triad are tested. Improvement in the quality and speed of gait are already recognized but cognitive improvement depends on several factors such as tests used, the time elapsed after LP for re-testing, and the number of punctures. Serial punctures may trigger similar conditions as external lumbar drainage (ELD) to the organism. Objective: This study aimed to identify how serial punctures afect cognition to increase the sensitivity of the test and consequently the accuracy of surgical indication. Methods: Sixty-one patients with INPH underwent baseline memory and executive tests repeatedly following the 2-Step Tap Test protocol (2-STT – two procedures of 30 mL lumbar CSF drainage separated by a 24-h interval). The baseline scores of INPH patients were compared with those of 55 healthy controls, and with intragroup post-puncture scores of the 2-STT. -

F-MARC Football Medicine Manual 2Nd Edition F-MARC Football Medicine Manual 2Nd Edition 2 Editors - Authors - Contributors | Football Medicine Manual
F-MARC Football Medicine Manual 2nd Edition F-MARC Football Medicine Manual 2nd Edition 2 Editors - Authors - Contributors | Football Medicine Manual Football Medicine Manual Editors DVORAK Jiri Prof. Dr F-MARC, Schulthess Clinic Zurich, Switzerland JUNGE Astrid Dr F-MARC, Schulthess Clinic Zurich, Switzerland GRIMM Katharina Dr FIFA Medical Offi ce Zurich, Switzerland Authors 2nd Edition 2009 ACKERMAN Kathryn E. Harvard Medical School Harvard, USA BABWAH Terence Dr Sports Medicine and Injury Rehabilitation Clinic Macoya, Trinidad BAHR Roald Prof. Dr Oslo Sports Trauma Research Center Oslo, Norway BANGSBO Jens Prof. Dr University of Copenhagen Copenhagen, Denmark BÄRTSCH Peter Prof. Dr University of Heidelberg Heidelberg, Germany BIZZINI Mario PT Schulthess Clinic Zurich, Switzerland CHOMIAK Jiri Dr Orthopaedic University Hospital Bulovka Prague, Czech Republic DVORAK Jiri Prof. Dr F-MARC, Schulthess Klinik Zurich, Switzerland EDWARDS Tony Dr Adidas Sports Medicine Auckland, New Zealand ENGEBRETSEN Lars Prof. Dr Oslo Sports Trauma Research Center Oslo, Norway FULLER Colin Prof. Dr University of Nottingham Nottingham, England GRIMM Katharina Dr FIFA Medical Offi ce Zurich, Switzerland JUNGE Astrid Dr F-MARC, Schulthess Clinic Zurich, Switzerland KHAN Karim Prof. Dr Editor in Chief British Journal of Sports Medicine Sydney, Australia Editors - Authors - Contributors | Football Medicine Manual 3 KOLBE John Prof. Dr University of Auckland Auckland, New Zealand LÜSCHER Thomas Prof. Dr University of Zurich Zurich, Switzerland MANDELBAUM Bert Dr Santa Monica Orthopaedic and Sports Medicine Group Santa Monica, USA MAUGHAN Ron Prof. Dr University of Loughborough Loughborough, Great Britain PETERSON Lars Prof. Dr Gothenburg Medical Center Gothenburg, Sweden REILLY Thomas Prof. Dr Liverpool John Moores University Liverpool, Great Britain SALTIN Bengt Prof. -

THE NEUROLOGY Exam & Clinical Pearls
THE NEUROLOGY Exam & Clinical Pearls Gaye McCafferty, RN, MS, NP-BC, MSCS, SCRN NPANYS-SPHP Education Day Troy, New York April 7, 2018 Objectives I. Describe the core elements of the neurology exam II. List clinical pearls of the neuro exam Neurology Exam . General Physical Exam . Mental Status . Cranial Nerves . Motor Exam . Reflex Examination . Sensory Exam . Coordination . Gait and Station 1 General Systemic Physical Exam Head Trauma Dysmorphism Neck Tone Thyromegaly Bruits MSOffice1 General Systemic Physical Exam .Cardiovascular . Heart rate, rhythm, murmur; peripheral pulses, JVD .Pulmonary . Breathing pattern, cyanosis, Mallampati airway .General Appearance Hygiene, grooming, weight (signs of self neglect) .Funduscopic Exam Mental Status Level of Consciousness . Awake . Drowsy . Somnolent . Comatose 2 Slide 5 MSOffice1 , 6/14/2009 Orientation & Attention . Orientation . Time . Place . Person Orientation & Attention . Attention . Digit Span-have the patient repeat a series of numbers, start with 3 or 4 in a series and increase until the patient makes several mistakes. Then explain that you want the numbers backwards. Normal-seven forward, five backward Hint; use parts of telephone numbers you know Memory Immediate recall and attention Tell the patient you want him to remember a name and address – Jim Green – 20 Woodlawn Road, Chicago Note how many errors are made in repeating it and how many times you have to repeat it before it is repeated correctly. Normal: Immediate registration 3 Memory . Short-term memory . About 5 minutes after asking the patient to remember the name and address, ask him to repeat it. Long –term memory . Test factual knowledge . Dates of WWII . Name a president who was shot dead Memory Mini-Mental State Exam – 30 items Mini-Cog – Rapid Screen for Cognitive Impairment – A Composite of 3 item recall and clock drawing – Takes about 5 minutes to administer Mini-Cog Mini-Cog Recall 0 Recall 1-2 Recall 3 Demented Non-demented Abnormal Clock Normal Clock Demented Non-demented 4 Memory . -
Toxicological Testing in Large Animals
Toxicological Testing in Large Animals Toxic causes of ill health and death in production animals are numerous. Toxin testing requires a specific toxin to be nominated as there is no suite of tests that covers all possibilities. Toxin testing is inherently expensive, requires specific sample types and false negatives can occur; for instance the toxin may have been eliminated from the body or be undetectable, but clinical signs may persist. Gribbles Veterinary Pathology can offer specific testing for a range of toxic substances, however it is important to consider the specific sample requirements and testing limitations for each toxin when advising your clients. Many tests are referred to external laboratories and may have extended turnaround times. Please contact the laboratory if you need testing for a specific toxin not listed here; we can often source unusual tests as needed from our network of referral laboratories. Clinicians should also consider syndromes which may mimic intoxication such as hypocalcaemia, hypoglycaemia, hepatic encephalopathy, peripheral neuropathies and primary CNS diseases. Examples of intoxicants that can be tested are provided below. See individual tests in the Pricelist for sample requirements and costs. Biological control agents Heavy metals • 1080 (fluoroacetate) • Arsenic • Strychnine • Lead • Synthetic pyrethroids • Copper • Organophosphates • Selenium • Organochlorines • Zinc • Carbamates • Metaldehyde • Anticoagulant rodenticides (warfarin, pindone, coumetetryl, bromadiolone, difenacoum, brodifacoum) -
Neuromuscular Disorders Neurology in Practice: Series Editors: Robert A
Neuromuscular Disorders neurology in practice: series editors: robert a. gross, department of neurology, university of rochester medical center, rochester, ny, usa jonathan w. mink, department of neurology, university of rochester medical center,rochester, ny, usa Neuromuscular Disorders edited by Rabi N. Tawil, MD Professor of Neurology University of Rochester Medical Center Rochester, NY, USA Shannon Venance, MD, PhD, FRCPCP Associate Professor of Neurology The University of Western Ontario London, Ontario, Canada A John Wiley & Sons, Ltd., Publication This edition fi rst published 2011, ® 2011 by Blackwell Publishing Ltd Blackwell Publishing was acquired by John Wiley & Sons in February 2007. Blackwell’s publishing program has been merged with Wiley’s global Scientifi c, Technical and Medical business to form Wiley-Blackwell. Registered offi ce: John Wiley & Sons Ltd, The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK Editorial offi ces: 9600 Garsington Road, Oxford, OX4 2DQ, UK The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK 111 River Street, Hoboken, NJ 07030-5774, USA For details of our global editorial offi ces, for customer services and for information about how to apply for permission to reuse the copyright material in this book please see our website at www.wiley.com/wiley-blackwell The right of the author to be identifi ed as the author of this work has been asserted in accordance with the UK Copyright, Designs and Patents Act 1988. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, except as permitted by the UK Copyright, Designs and Patents Act 1988, without the prior permission of the publisher. -

Information About Tick Paralysis? Adapted From: CDC
Peachtree Street NW, 15th Floor Atlanta, Georgia 30303-3142 Georgia Department of Public Health www.health.state.ga.us Tick Paralysis Q&A What is tick paralysis? Tick paralysis refers to acute onset of paralysis caused by a tick bite. The condition is primarily found in the Rocky Mountain and northwestern regions of the United States and is rare in Georgia. The number of cases per year is unknown because physicians are not required to report cases of tick paralysis to Public Health. How is tick paralysis spread? Tick paralysis results from a neurotoxin that is secreted in the saliva of certain ticks when they feed. The tick must be attached for several days. Person‐to‐person transmission of tick paralysis has not been documented. Who gets tick paralysis? Anyone who is bitten by a tick can get tick paralysis, but it most commonly affects children less than 10 years of age. What are the symptoms of tick paralysis? The symptoms of tick paralysis include weakness in the legs and arms, followed by paralysis beginning in the legs and moving upward. If unrecognized, tick paralysis may progress to respiratory failure and may be fatal in 10% of cases. What is the treatment for tick paralysis? Treatment for tick paralysis is simply removal of the tick. Once the tick is found and removed, the patient recovers fully, often within a matter of hours. It is often difficult to find the tick, which can be attached to the scalp and hidden in the hair. What can be done to prevent the spread of tick paralysis? There are no vaccines to prevent tick‐borne disease, so limiting exposure to ticks is very important. -

Cerebellar Examination 1. General Inspection As Above 2. Posture
Cerebellar Examination 1. General Inspection as above 2. Posture: - Whilst the child is sitting, get him/her to lift his feet from the ground with arms crossed (Truncal ataxia) - Get the child to stand up and maintain position with feet together and eyes opened. And then with eyes closed (Rhomberg ’s test). If the child is ataxic and unsteady with eyes closed (Rhomberg ’s test positive), then the problem is likely to be sensory ataxia, rather than cerebellar ataxia. 3. Gait - Get patient to walk (broad-based ataxic gait, falls towards the side of the lesion) , then ask him to STOP, turn back and do - Heel to toe walk 4. Face - Eyes : H test for extraocular muscles and pause at lateral gaze – horizontal nystagmus, towards the side of the lesion (lateral cerebellar lesion) - Speech: Ask the child question / ask him to read/ for older child, ask him to say baby hippotamus, West register street/ british constitution (staccato speech/ scanning dysarthria) 5. Upper limbs -Pronator drift – ask patient to hold his arms out with his palm facing upwards and his eyes closed : Pronator drift – weakness ; Upward drift – cerebellar lesion -Rebound test- whilst patients arms are held out, push his wrist down quickly (Holmes’ rebound phenomenon – over correction of passive displacement of limb) -Hypotonia - Rapid palm test (Dysdiadoschokinesia) -Finger-nose test (Dysmetria) 6. Lower limbs - Hypotonia - Reflex: pendular reflex, best seen when patients limb left hanging in the air - Heel-shin test To complete the examination, I would -check the fundi for papilloedema (space occupying lesion) - perform a full neurological examination Causes of cerebellar lesions: 1. -

Quantitative MRI for Rapid and User-Independent Monitoring of Intracranial CSF Volume in Hydrocephalus
ORIGINAL RESEARCH ADULT BRAIN Quantitative MRI for Rapid and User-Independent Monitoring of Intracranial CSF Volume in Hydrocephalus X J. Virhammar, X M. Warntjes, X K. Laurell, and X E.-M. Larsson ABSTRACT BACKGROUND AND PURPOSE: Quantitative MR imaging allows segmentation of different tissue types and automatic calculation of intracranial volume, CSF volume, and brain parenchymal fraction. Brain parenchymal fraction is calculated as (intracranial volume Ϫ CSF volume) / intracranial volume. The purpose of this study was to evaluate whether the automatic calculation of intracranial CSF volume or brain parenchymal fraction could be used as an objective method to monitor volume changes in the ventricles. MATERIALS AND METHODS: A lumbar puncture with drainage of 40 mL of CSF was performed in 23 patients under evaluation for idiopathic normal pressure hydrocephalus. Quantitative MR imaging was performed twice within 1 hour before the lumbar puncture and was repeated 30 minutes, 4 hours, and 24 hours afterward. For each time point, the volume of the lateral ventricles was manually segmented and total intracranial CSF volume and brain parenchymal fraction were automatically calculated by using Synthetic MR postprocessing. RESULTS: At 30 minutes after the lumbar puncture, the volume of the lateral ventricles decreased by 5.6 Ϯ 1.9 mL (P Ͻ .0001) and the total intracranial CSF volume decreased by 11.3 Ϯ 5.6 mL (P Ͻ .001), while brain parenchymal fraction increased by 0.78% Ϯ 0.41% (P Ͻ .001). Differences were significant for manual segmentation and brain parenchymal fraction even at 4 hours and 24 hours after the lumbar tap.