Vol24no6 Pdf-Version.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Heartland and Bourbon Virus Testing Guideance for Healthcare Providers
Heartland and Bourbon Virus Testing Guidance for Healthcare Providers Heartland virus is an RNA virus believed to be transmitted by the Lone Star tick (Amblyomma americanum). Most patients reported tick exposure in the two weeks prior to illness onset. While no cases have been reported in Louisiana, this tick is found in Louisiana. First discovered as a cause of human illness in 2009 in Missouri, more than 40 cases have been reported from states in Midwestern and southern U.S. to date. Initial symptoms of Heartland virus disease are very similar to those of ehrlichiosis or anaplasmosis, which include fever, fatigue, anorexia, nausea and diarrhea. Cases have also had leukopenia, thrombocytopenia, and mild to moderate elevation of liver transaminases. Heartland virus disease should be considered in patients being treated for ehrlichiosis who do not respond to treatment with doxycycline. For several years, CDC has been working under IRB-approved protocols to identify additional cases and validate diagnostic test for several novel pathogens. Now the CDC Arboviral Diseases Branch offers routine diagnostic testing for Heartland and Bourbon viruses (RT-PCR, IgM and IgG MIA, PRNT). There is no commercial testing available. Treatment of Heartland virus disease is supportive only. Many patients diagnosed with the disease have required hospitalization. With supportive care, most people have fully recovered; however, a few older individuals with medical comorbidities have died. The best way to prevent Heartland virus infection is to avoid exposure -

2016 New Jersey Reportable Communicable Disease Report (January 3, 2016 to December 31, 2016) (Excl
10:34 Friday, June 30, 2017 1 2016 New Jersey Reportable Communicable Disease Report (January 3, 2016 to December 31, 2016) (excl. Sexually Transmitted Diseases, HIV/AIDS and Tuberculosis) (Refer to Technical Notes for Reporting Criteria) Case Jurisdiction Disease Counts STATE TOTAL AMOEBIASIS 98 STATE TOTAL ANTHRAX 0 STATE TOTAL ANTHRAX - CUTANEOUS 0 STATE TOTAL ANTHRAX - INHALATION 0 STATE TOTAL ANTHRAX - INTESTINAL 0 STATE TOTAL ANTHRAX - OROPHARYNGEAL 0 STATE TOTAL BABESIOSIS 174 STATE TOTAL BOTULISM - FOODBORNE 0 STATE TOTAL BOTULISM - INFANT 10 STATE TOTAL BOTULISM - OTHER, UNSPECIFIED 0 STATE TOTAL BOTULISM - WOUND 1 STATE TOTAL BRUCELLOSIS 1 STATE TOTAL CALIFORNIA ENCEPHALITIS(CE) 0 STATE TOTAL CAMPYLOBACTERIOSIS 1907 STATE TOTAL CHIKUNGUNYA 11 STATE TOTAL CHOLERA - O1 0 STATE TOTAL CHOLERA - O139 0 STATE TOTAL CREUTZFELDT-JAKOB DISEASE 4 STATE TOTAL CREUTZFELDT-JAKOB DISEASE - FAMILIAL 0 STATE TOTAL CREUTZFELDT-JAKOB DISEASE - IATROGENIC 0 STATE TOTAL CREUTZFELDT-JAKOB DISEASE - NEW VARIANT 0 STATE TOTAL CREUTZFELDT-JAKOB DISEASE - SPORADIC 2 STATE TOTAL CREUTZFELDT-JAKOB DISEASE - UNKNOWN 1 STATE TOTAL CRYPTOSPORIDIOSIS 198 STATE TOTAL CYCLOSPORIASIS 29 STATE TOTAL DENGUE FEVER - DENGUE 43 STATE TOTAL DENGUE FEVER - DENGUE-LIKE ILLNESS 3 STATE TOTAL DENGUE FEVER - SEVERE DENGUE 4 STATE TOTAL DIPHTHERIA 0 STATE TOTAL EASTERN EQUINE ENCEPHALITIS(EEE) 1 STATE TOTAL EBOLA 0 STATE TOTAL EHRLICHIOSIS/ANAPLASMOSIS - ANAPLASMA PHAGOCYTOPHILUM (PREVIOUSLY HGE) 109 STATE TOTAL EHRLICHIOSIS/ANAPLASMOSIS - EHRLICHIA CHAFFEENSIS (PREVIOUSLY -

Joint Statement on Insect Repellents by EPA And
Joint Statement on Insect Repellents from the Environmental Protection Agency and the Centers for Disease Control and Prevention July 17, 2014 The Environmental Protection Agency (EPA) and Centers for Disease Control and Prevention (CDC) are recommending that the public use insect repellents and take other precautions to avoid biting insects that carry serious diseases. The incidence of these diseases is on the rise. This joint statement discusses diseases that are transmitted by ticks and mosquitoes, the role of government in vector control and disease prevention, the history of repellents, how to use repellents as part of an integrated control program, and how to select and use a repellent. Introduction and Purpose CDC and EPA developed this joint statement to promote awareness of repellents and to highlight the effectiveness of repellents in preventing mosquito and tick bites. The agencies believe that promoting the use of repellents may reduce the impact of diseases and nuisance effects caused by these pests. Vector-borne diseases, such as those transmitted by mosquitoes and ticks, are among the world's leading causes of illness and death today. A wide variety of arthropods, including mosquitoes, ticks, fleas, black flies, sand flies, horse flies, stable flies, kissing bugs, lice and mites, feed on human blood. Among these, mosquitoes and ticks transmit some of the most serious vector- borne diseases both globally and within the United States. Diseases Transmitted by Mosquitoes and Ticks Mosquito-transmitted West Nile virus caused over 36,000 disease cases and 1,500 deaths in the United States between 1999 and 2012 (CDC, 2012). Mosquitoes also transmit other viruses that cause severe disease in the United States, including La Crosse encephalitis, eastern equine encephalitis and dengue. -

HIV (Human Immunodeficiency Virus)
TABLE OF CONTENTS AFRICAN TICK BITE FEVER .........................................................................................3 AMEBIASIS .....................................................................................................................4 ANTHRAX .......................................................................................................................5 ASEPTIC MENINGITIS ...................................................................................................6 BACTERIAL MENINGITIS, OTHER ................................................................................7 BOTULISM, FOODBORNE .............................................................................................8 BOTULISM, INFANT .......................................................................................................9 BOTULISM, WOUND .................................................................................................... 10 BOTULISM, OTHER ...................................................................................................... 11 BRUCELLOSIS ............................................................................................................. 12 CAMPYLOBACTERIOSIS ............................................................................................. 13 CHANCROID ................................................................................................................. 14 CHLAMYDIA TRACHOMATIS INFECTION ................................................................. -

Chiroptera: Vespertilionidae) from Taiwan and Adjacent China
Zootaxa 3920 (1): 301–342 ISSN 1175-5326 (print edition) www.mapress.com/zootaxa/ Article ZOOTAXA Copyright © 2015 Magnolia Press ISSN 1175-5334 (online edition) http://dx.doi.org/10.11646/zootaxa.3920.2.6 http://zoobank.org/urn:lsid:zoobank.org:pub:8B991675-0C48-40D4-87D2-DACA524D17C2 Molecular phylogeny and morphological revision of Myotis bats (Chiroptera: Vespertilionidae) from Taiwan and adjacent China MANUEL RUEDI1,5, GÁBOR CSORBA2, LIANG- KONG LIN3 & CHENG-HAN CHOU3,4 1Department of Mammalogy and Ornithology, Natural History Museum of Geneva, Route de Malagnou 1, BP 6434, 1211 Geneva (6), Switzerland. E-mail: [email protected] 2Department of Zoology, Hungarian Natural History Museum, Budapest, Baross u. 13., H-1088. E-mail: [email protected] 3Laboratory of Wildlife Ecology, Department of Biology, Tunghai University, Taichung, Taiwan 407, R.O.C. E-mail: [email protected] 4Division of Zoology, Endemic Species Research Institute, Nantou, Taiwan 552, R.O.C. E-mail: [email protected] 5Corresponding author Table of contents Abstract . 301 Introduction . 302 Material and methods . 310 Results . 314 Discussion . 319 Systematic account . 319 Submyotodon latirostris (Kishida, 1932) . 319 Myotis fimbriatus (Peters, 1870) . 321 Myotis laniger (Peters, 1870) . 322 Myotis secundus sp. n. 324 Myotis soror sp. n. 327 Myotis frater Allen, 1923 . 331 Myotis formosus (Hodgson, 1835) . 334 Myotis rufoniger (Tomes, 1858) . 335 Biogeography and conclusions . 336 Key to the Myotinae from Taiwan and adjacent mainland China . 337 Acknowledgments . 337 References . 338 Abstract In taxonomic accounts, three species of Myotis have been traditionally reported to occur on the island of Taiwan: Watase’s bat (M. -
Summer Safety Guide C L I N T O N C O U N T Y H E a L T H D E P a R T M E N T
SUMMER SAFETY GUIDE C L I N T O N C O U N T Y H E A L T H D E P A R T M E N T S U M M E R 2 0 1 7 WHAT'S INSIDE... 2 7 W H A T ' S B I T I N G Y O U ? P R O T E C T Y O U R H O M E 3 8-9 M O S Q U I T O E S A N I M A L S A N D R A B I E S 4-5 10 T I C K S A N D L Y M E D I S E A S E B E D B U G S 6 11-12 P R O T E C T Y O U R S E L F S U N A N D W A T E R S A F E T Y WHAT'S BITING YOU? P R E V E N T I O N I S Y O U R B E S T D E F E N S E SUMMER HAS ARRIVED! THAT Mosquitoes West Nile virus (WNV) and Eastern MEANS SUN AND FUN, BUT IT equine encephalitis (EEE) are the most common diseases transmitted IS ALSO THE TIME OF YEAR Animals by local mosquitoes. There are no Wildlife is part of the beauty of our WHEN PEOPLE ARE MOST human vaccines for these diseases, Adirondack region, but animals are but there are simple steps you can best viewed from afar. -

Tick-Borne Disease Working Group 2020 Report to Congress
2nd Report Supported by the U.S. Department of Health and Human Services • Office of the Assistant Secretary for Health Tick-Borne Disease Working Group 2020 Report to Congress Information and opinions in this report do not necessarily reflect the opinions of each member of the Working Group, the U.S. Department of Health and Human Services, or any other component of the Federal government. Table of Contents Executive Summary . .1 Chapter 4: Clinical Manifestations, Appendices . 114 Diagnosis, and Diagnostics . 28 Chapter 1: Background . 4 Appendix A. Tick-Borne Disease Congressional Action ................. 8 Chapter 5: Causes, Pathogenesis, Working Group .....................114 and Pathophysiology . 44 The Tick-Borne Disease Working Group . 8 Appendix B. Tick-Borne Disease Working Chapter 6: Treatment . 51 Group Subcommittees ...............117 Second Report: Focus and Structure . 8 Chapter 7: Clinician and Public Appendix C. Acronyms and Abbreviations 126 Chapter 2: Methods of the Education, Patient Access Working Group . .10 to Care . 59 Appendix D. 21st Century Cures Act ...128 Topic Development Briefs ............ 10 Chapter 8: Epidemiology and Appendix E. Working Group Charter. .131 Surveillance . 84 Subcommittees ..................... 10 Chapter 9: Federal Inventory . 93 Appendix F. Federal Inventory Survey . 136 Federal Inventory ....................11 Chapter 10: Public Input . 98 Appendix G. References .............149 Minority Responses ................. 13 Chapter 11: Looking Forward . .103 Chapter 3: Tick Biology, Conclusion . 112 Ecology, and Control . .14 Contributions U.S. Department of Health and Human Services James J. Berger, MS, MT(ASCP), SBB B. Kaye Hayes, MPA Working Group Members David Hughes Walker, MD (Co-Chair) Adalbeto Pérez de León, DVM, MS, PhD Leigh Ann Soltysiak, MS (Co-Chair) Kevin R. -

(Sciurus Carolinensis) with the Contraceptive Agent Diazacontm
Integrative Zoology 2011; 6: 409-419 doi: 10.1111/j.1749-4877.2011.00247.x 1 1 2 2 3 Feeding of grey squirrels (Sciurus carolinensis) with the contraceptive 3 4 4 5 agent DiazaConTM: effect on cholesterol, hematology, and blood 5 6 6 7 chemistry 7 8 8 9 9 10 10 1 2 1 3 11 Christi A. YODER, Brenda A. MAYLE, Carol A. FURCOLOW, David P. COWAN and 11 12 Kathleen A. FAGERSTONE1 12 13 13 1 2 14 National Wildlife Research Center, Fort Collins, Colorado, USA, Forest Research, Alice Holt Lodge, Farnham, Surrey, UK and 14 15 3Central Science Laboratory, Sand Hutton, York, UK 15 16 16 17 17 18 18 19 Abstract 19 20 Grey squirrels (Sciurus carolinensis) are an invasive species in Britain and Italy. They have replaced native 20 21 red squirrels (Sciurus vulgaris) throughout most of Britain, and cause damage to trees. Currently, lethal con- 21 22 trol is used to manage grey squirrel populations in Britain, but nonlethal methods might be more acceptable to 22 23 the public. One such method is contraception with 20,25-diazacholesterol dihydrochloride (DiazaConTM). Di- 23 24 azaConTM inhibits the conversion of desmosterol to cholesterol, resulting in increasing desmosterol concentra- 24 25 tions and decreasing cholesterol concentrations. Because cholesterol is needed for the synthesis of steroid repro- 25 26 ductive hormones, such as progesterone and testosterone, inhibition of cholesterol synthesis indirectly inhibits 26 27 reproduction. Desmosterol is used as a marker of efficacy in laboratory studies with species that do not repro- 27 28 duce readily in captivity. -

ADV Heartland and Bourbon Virus Testing Guidance in Pennsylvania
PENNSYLVANIA DEPARTMENT OF HEALTH 201 8– PAHAN –418 –07-27- ADV Heartland and Bourbon Virus Testing Guidance in Pennsylvania DATE: July 27, 2018 TO:DATE: Health Alert Network FROM: Rachel Levine, MD, Secretary of Health SUBJECT: Heartland and Bourbon Virus Testing Guidance DISTRIBUTION: Statewide LOCATION: Statewide STREET ADDRESS: n/a COUNTY: n/a MUNICIPALITY: n/a ZIP CODE: n/a This transmission is a “Health Advisory” provides important information for a specific incident or situation; may not require immediate action. HOSPITALS : PLEASE SHARE WITH ALL MEDICAL, PEDIATRIC, INFECTION CONTROL, NURSING AND LABORATORY STAFF IN YOUR HOSPITAL; EMS COUNCILS: PLEASE DISTRIBUTE AS APPROPRIATE; FQHCs: PLEASE DISTRIBUTE AS APPROPRIATE LOCAL HEALTH JURISDICTIONS: PLEASE DISTRIBUTE AS APPROPRIATE; PROFESSIONAL ORGANIZATIONS: PLEASE DISTRIBUTE TO YOUR MEMBERSHIP Summary • CDC Arboviral Diseases Branch will now offer routine diagnostic testing for Heartland and Bourbon viruses (transmitted by the Lone Star tick). • To submit samples for testing, send to PADOH BOL with both BOL and CDC submission forms. • In addition to testing for more likely arboviruses in Pennsylvania (such as West Nile, Powassan, Eastern equine encephalitis, etc.), testing for Heartland or Bourbon virus should be considered for patients with an acute febrile illness within the past 3 months AND at least one epidemiologic criterion AND at least one clinical criterion (see below for details). Background on Heartland and Bourbon virus Heartland virus is an RNA virus in the genus Phlebovirus, family Phenuiviridae believed to be transmitted by the Lone Star tick (Amblyomma americanum). First discovered as a cause of human illness in 2009 in Missouri, more than 35 cases of Heartland virus disease have been reported from states in the midwestern and southern United States to date. -
OPTIONS X Programme
Options X for the Control of Influenza | WELCOME MESSAGES BREAKTHROUGH INFLUENZA VACCINES TAKE LARGE DOSES OF INNOVATION Protecting people from the ever-changing threat of influenza takes unwavering commitment. That’s why we’re dedicated to developing advanced technologies and vaccines that can fight influenza as it evolves. We’re with you. ON THE FRONT LINETM BREAKTHROUGH INFLUENZA VACCINES TAKE LARGE DOSES OF INNOVATION CONTENT OPTIONS X SUPPORTERS ------------------- 4 OPTIONS X EXHIBITORS & COMMITTEES ------------------- 5 AWARD INFORMATION ------------------- 6 WELCOME MESSAGES ------------------- 7 SCHEDULE AT A GLANCE ------------------- 10 CONFERENCE INFORMATION ------------------- 11 SOCIAL PROGRAMME ------------------- 14 ABOUT SINGAPORE ------------------- 15 SUNTEC FLOORPLAN ------------------- 16 SCIENTIFIC COMMUNICATIONS ------------------- 17 PROGRAMME ------------------- 19 SPEAKERS ------------------- 31 SPONSORED SYMPOSIA ------------------- 39 ORAL PRESENTATION LISTINGS ------------------- 42 POSTER PRESENTATION LISTINGS ------------------- 51 ABSTRACTS POSTER DISPLAY LISTINGS ------------------- 54 SPONSOR AND EXHIBITOR LISTINGS ------------------- 80 EXHIBITION FLOORPLAN ------------------- 83 Protecting people from the ever-changing threat of NOTE ------------------- 84 influenza takes unwavering commitment. That’s why we’re dedicated to developing advanced technologies and vaccines that can fight influenza as it evolves. We’re with you. ON THE FRONT LINETM Options X for the Control of Influenza | OPTIONS X SUPPORTERS -
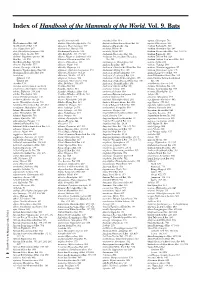
Index of Handbook of the Mammals of the World. Vol. 9. Bats
Index of Handbook of the Mammals of the World. Vol. 9. Bats A agnella, Kerivoula 901 Anchieta’s Bat 814 aquilus, Glischropus 763 Aba Leaf-nosed Bat 247 aladdin, Pipistrellus pipistrellus 771 Anchieta’s Broad-faced Fruit Bat 94 aquilus, Platyrrhinus 567 Aba Roundleaf Bat 247 alascensis, Myotis lucifugus 927 Anchieta’s Pipistrelle 814 Arabian Barbastelle 861 abae, Hipposideros 247 alaschanicus, Hypsugo 810 anchietae, Plerotes 94 Arabian Horseshoe Bat 296 abae, Rhinolophus fumigatus 290 Alashanian Pipistrelle 810 ancricola, Myotis 957 Arabian Mouse-tailed Bat 164, 170, 176 abbotti, Myotis hasseltii 970 alba, Ectophylla 466, 480, 569 Andaman Horseshoe Bat 314 Arabian Pipistrelle 810 abditum, Megaderma spasma 191 albatus, Myopterus daubentonii 663 Andaman Intermediate Horseshoe Arabian Trident Bat 229 Abo Bat 725, 832 Alberico’s Broad-nosed Bat 565 Bat 321 Arabian Trident Leaf-nosed Bat 229 Abo Butterfly Bat 725, 832 albericoi, Platyrrhinus 565 andamanensis, Rhinolophus 321 arabica, Asellia 229 abramus, Pipistrellus 777 albescens, Myotis 940 Andean Fruit Bat 547 arabicus, Hypsugo 810 abrasus, Cynomops 604, 640 albicollis, Megaerops 64 Andersen’s Bare-backed Fruit Bat 109 arabicus, Rousettus aegyptiacus 87 Abruzzi’s Wrinkle-lipped Bat 645 albipinnis, Taphozous longimanus 353 Andersen’s Flying Fox 158 arabium, Rhinopoma cystops 176 Abyssinian Horseshoe Bat 290 albiventer, Nyctimene 36, 118 Andersen’s Fruit-eating Bat 578 Arafura Large-footed Bat 969 Acerodon albiventris, Noctilio 405, 411 Andersen’s Leaf-nosed Bat 254 Arata Yellow-shouldered Bat 543 Sulawesi 134 albofuscus, Scotoecus 762 Andersen’s Little Fruit-eating Bat 578 Arata-Thomas Yellow-shouldered Talaud 134 alboguttata, Glauconycteris 833 Andersen’s Naked-backed Fruit Bat 109 Bat 543 Acerodon 134 albus, Diclidurus 339, 367 Andersen’s Roundleaf Bat 254 aratathomasi, Sturnira 543 Acerodon mackloti (see A. -

Bin Brook Easter 2018
Bin Brook Draft 4 AW.qxp_Layout 1 01/08/2018 13:48 Page 1 BIN EASTER 2018 BROOK ROBINSON COLLEGE UNIVERSITY OF CAMBRIDGE Diversifying Robinson Bringing Focus on Medicine From bats to Travels with our students India Remembering Robinson the brightest and best to Cambridge herpes with Robinson's medics and Iraq with Zhuan and Molly Dr Mary Stewart's living legacy Bin Brook Draft 4 AW.qxp_Layout 1 01/08/2018 13:48 Page 2 02 Contents WELCOME 03 News in brief 04 Diversifying Robinson Bin Brook is Robinson’s flagship publication, keeping our alumni and friends 05 Access to Robinson Eleanor Humphrey in touch with the College and with each other. In view of its importance 06 My Robinson Dr Ben Guy we felt it was owed a facelift, and we hope you like the new look. 07 e Cancer Problem Dr Gary Doherty 08 Must all that lives die? Dr Anke Timmerman Easter 2018 is the first in a series of themed issues, focusing this time on the ground- breaking work of our Fellows in Medicine. ere can be few of us whose lives have 09 Fighting fluProfessor Wendy Barclay been untouched by illnesses such as cancer, viral disease or dementia, and it’s exciting to see that the research that may change the direction of our approaches 10 Bats in the limelight Dr Oliver Restif to these modern-day plagues may come out of Robinson. 11 Learning about memory Dr Brian McCabe Oxbridge admissions have been in the media spotlight recently and we are pleased to offer an 12 Brain Training Dr Duncan Astle insight into our outreach work, answering some of our readers’ questions on this most important 13 e Medic’s Tale Oliver Fox subject that is so close to Robinson’s heart and heritage.