Draft Outline
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Bulawayo City Mpilo Central Hospital
Province District Name of Site Bulawayo Bulawayo City E. F. Watson Clinic Bulawayo Bulawayo City Mpilo Central Hospital Bulawayo Bulawayo City Nkulumane Clinic Bulawayo Bulawayo City United Bulawayo Hospital Manicaland Buhera Birchenough Bridge Hospital Manicaland Buhera Murambinda Mission Hospital Manicaland Chipinge Chipinge District Hospital Manicaland Makoni Rusape District Hospital Manicaland Mutare Mutare Provincial Hospital Manicaland Mutasa Bonda Mission Hospital Manicaland Mutasa Hauna District Hospital Harare Chitungwiza Chitungwiza Central Hospital Harare Chitungwiza CITIMED Clinic Masvingo Chiredzi Chikombedzi Mission Hospital Masvingo Chiredzi Chiredzi District Hospital Masvingo Chivi Chivi District Hospital Masvingo Gutu Chimombe Rural Hospital Masvingo Gutu Chinyika Rural Hospital Masvingo Gutu Chitando Rural Health Centre Masvingo Gutu Gutu Mission Hospital Masvingo Gutu Gutu Rural Hospital Masvingo Gutu Mukaro Mission Hospital Masvingo Masvingo Masvingo Provincial Hospital Masvingo Masvingo Morgenster Mission Hospital Masvingo Mwenezi Matibi Mission Hospital Masvingo Mwenezi Neshuro District Hospital Masvingo Zaka Musiso Mission Hospital Masvingo Zaka Ndanga District Hospital Matabeleland South Beitbridge Beitbridge District Hospital Matabeleland South Gwanda Gwanda Provincial Hospital Matabeleland South Insiza Filabusi District Hospital Matabeleland South Mangwe Plumtree District Hospital Matabeleland South Mangwe St Annes Mission Hospital (Brunapeg) Matabeleland South Matobo Maphisa District Hospital Matabeleland South Umzingwane Esigodini District Hospital Midlands Gokwe South Gokwe South District Hospital Midlands Gweru Gweru Provincial Hospital Midlands Kwekwe Kwekwe General Hospital Midlands Kwekwe Silobela District Hospital Midlands Mberengwa Mberengwa District Hospital . -

Promotion of Climate-Resilient Lifestyles Among Rural Families in Gutu
Promotion of climate-resilient lifestyles among rural families in Gutu (Masvingo Province), Mutasa (Manicaland Province) and Shamva (Mashonaland Central Province) Districts | Zimbabwe Sahara and Sahel Observatory 26 November 2019 Promotion of climate-resilient lifestyles among rural families in Gutu Project/Programme title: (Masvingo Province), Mutasa (Manicaland Province) and Shamva (Mashonaland Central Province) Districts Country(ies): Zimbabwe National Designated Climate Change Management Department, Ministry of Authority(ies) (NDA): Environment, Water and Climate Development Aid from People to People in Zimbabwe (DAPP Executing Entities: Zimbabwe) Accredited Entity(ies) (AE): Sahara and Sahel Observatory Date of first submission/ 7/19/2019 V.1 version number: Date of current submission/ 11/26/2019 V.2 version number A. Project / Programme Information (max. 1 page) ☒ Project ☒ Public sector A.2. Public or A.1. Project or programme A.3 RFP Not applicable private sector ☐ Programme ☐ Private sector Mitigation: Reduced emissions from: ☐ Energy access and power generation: 0% ☐ Low emission transport: 0% ☐ Buildings, cities and industries and appliances: 0% A.4. Indicate the result ☒ Forestry and land use: 25% areas for the project/programme Adaptation: Increased resilience of: ☒ Most vulnerable people and communities: 25% ☒ Health and well-being, and food and water security: 25% ☐ Infrastructure and built environment: 0% ☒ Ecosystem and ecosystem services: 25% A.5.1. Estimated mitigation impact 399,223 tCO2eq (tCO2eq over project lifespan) A.5.2. Estimated adaptation impact 12,000 direct beneficiaries (number of direct beneficiaries) A.5. Impact potential A.5.3. Estimated adaptation impact 40,000 indirect beneficiaries (number of indirect beneficiaries) A.5.4. Estimated adaptation impact 0.28% of the country’s total population (% of total population) A.6. -
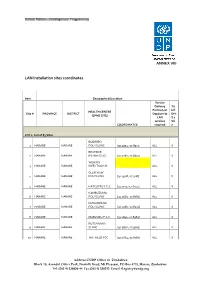
LAN Installation Sites Coordinates
ANNEX VIII LAN Installation sites coordinates Item Geographical/Location Service Delivery Tic Points (List k if HEALTH CENTRE Site # PROVINCE DISTRICT Dept/umits DHI (EPMS SITE) LAN S 2 services Sit COORDINATES required e LOT 1: List of 83 Sites BUDIRIRO 1 HARARE HARARE POLYCLINIC [30.9354,-17.8912] ALL X BEATRICE 2 HARARE HARARE RD.INFECTIO [31.0282,-17.8601] ALL X WILKINS 3 HARARE HARARE INFECTIOUS H ALL X GLEN VIEW 4 HARARE HARARE POLYCLINIC [30.9508,-17.908] ALL X 5 HARARE HARARE HATCLIFFE P.C.C. [31.1075,-17.6974] ALL X KAMBUZUMA 6 HARARE HARARE POLYCLINIC [30.9683,-17.8581] ALL X KUWADZANA 7 HARARE HARARE POLYCLINIC [30.9285,-17.8323] ALL X 8 HARARE HARARE MABVUKU P.C.C. [31.1841,-17.8389] ALL X RUTSANANA 9 HARARE HARARE CLINIC [30.9861,-17.9065] ALL X 10 HARARE HARARE HATFIELD PCC [31.0864,-17.8787] ALL X Address UNDP Office in Zimbabwe Block 10, Arundel Office Park, Norfolk Road, Mt Pleasant, PO Box 4775, Harare, Zimbabwe Tel: (263 4) 338836-44 Fax:(263 4) 338292 Email: [email protected] NEWLANDS 11 HARARE HARARE CLINIC ALL X SEKE SOUTH 12 HARARE CHITUNGWIZA CLINIC [31.0763,-18.0314] ALL X SEKE NORTH 13 HARARE CHITUNGWIZA CLINIC [31.0943,-18.0152] ALL X 14 HARARE CHITUNGWIZA ST.MARYS CLINIC [31.0427,-17.9947] ALL X 15 HARARE CHITUNGWIZA ZENGEZA CLINIC [31.0582,-18.0066] ALL X CHITUNGWIZA CENTRAL 16 HARARE CHITUNGWIZA HOSPITAL [31.0628,-18.0176] ALL X HARARE CENTRAL 17 HARARE HARARE HOSPITAL [31.0128,-17.8609] ALL X PARIRENYATWA CENTRAL 18 HARARE HARARE HOSPITAL [30.0433,-17.8122] ALL X MURAMBINDA [31.65555953980,- 19 MANICALAND -
Census Results in Brief
116 Appendix 1a: Census Questionnaire 117 118 119 120 Appendix 1b: Census Questionnaire Code List Question 6-8 and 10 Census District Country code MANICALAND 1 Sanyati 407 Shurugwi 726 Rural Districts Urban Areas MASVINGO 8 Buhera 101 Chinhoyi 421 Rural Districts Chimanimani 102 Kadoma 422 Bikita 801 Chipinge 103 Chegutu 423 Chiredzi 802 Makoni 104 Kariba 424 Chivi 803 Mutare Rural 105 Norton 425 Gutu 804 Mutasa 106 Karoi 426 Masvingo Rural 805 Nyanga 107 MATABELELAND NORTH 5 Mwenezi 806 Urban Areas Rural Districts Zaka 807 Mutare 121 Binga 501 Urban Areas Rusape 122 Bubi 502 Masvingo Urban 821 Chipinge 123 Hwange 503 Chiredzi Town 822 MASHONALAND CENTRAL 2 Lupane 504 Rural Districts Nkayi 505 HARARE 9 Bindura 201 Tsholotsho 506 Harare Rural 901 Centenary 202 Umguza 507 Harare Urban 921 Guruve 203 Urban Areas Chitungwiza 922 Mazowe 204 Hwange 521 Epworth 923 Mount Darwin 205 Victoria Falls 522 BULAWAYO 0 Rushinga 206 MATABELELAND SOUTH 6 Bulawayo Urban 21 Shamva 207 Rural Districts AFRICAN COUNTRIES Mbire 208 Beitbridge Rural 601 Zimbabwe 0 Urban Areas Bulilima 602 Botswana 941 Bindura 221 Mangwe 603 Malawi 942 Mvurwi 222 Gwanda Rural 604 Mozambique 943 MASHONALAND EAST 3 Insiza 605 South Africa 944 Rural Districts Matobo 606 Zambia 945 Chikomba 301 Umzingwane 607 Other African Countries 949 Goromonzi 302 Urban Areas OUTSIDE AFRICA Hwedza 303 Gwanda 621 United Kingdom 951 Marondera 304 Beitbridge Urban 622 Other European Countries 952 Mudzi 305 Plumtree 623 American Countries 953 Murehwa 306 MIDLANDS 7 Asian Countries 954 Mutoko 307 Rural Districts Other Countries 959 701 Seke 308 Chirumhanzu Uzumba-Maramba-Pfungwe 309 Gokwe North 702 Urban Areas Gokwe South 703 Marondera 321 Gweru Rural 704 Chivhu Town Board 322 Kwekwe Rural 705 Ruwa Local Board 323 Mberengwa 706 MASHONALAND WEST 4 Shurugwi 707 Rural Districts Zvishavane 708 Chegutu 401 Urban Areas Hurungwe 402 Gweru 721 Mhondoro-Ngezi 403 Kwekwe 722 Kariba 404 Redcliff 723 Makonde 405 Zvishavane 724 Gokwe Centre 725 . -

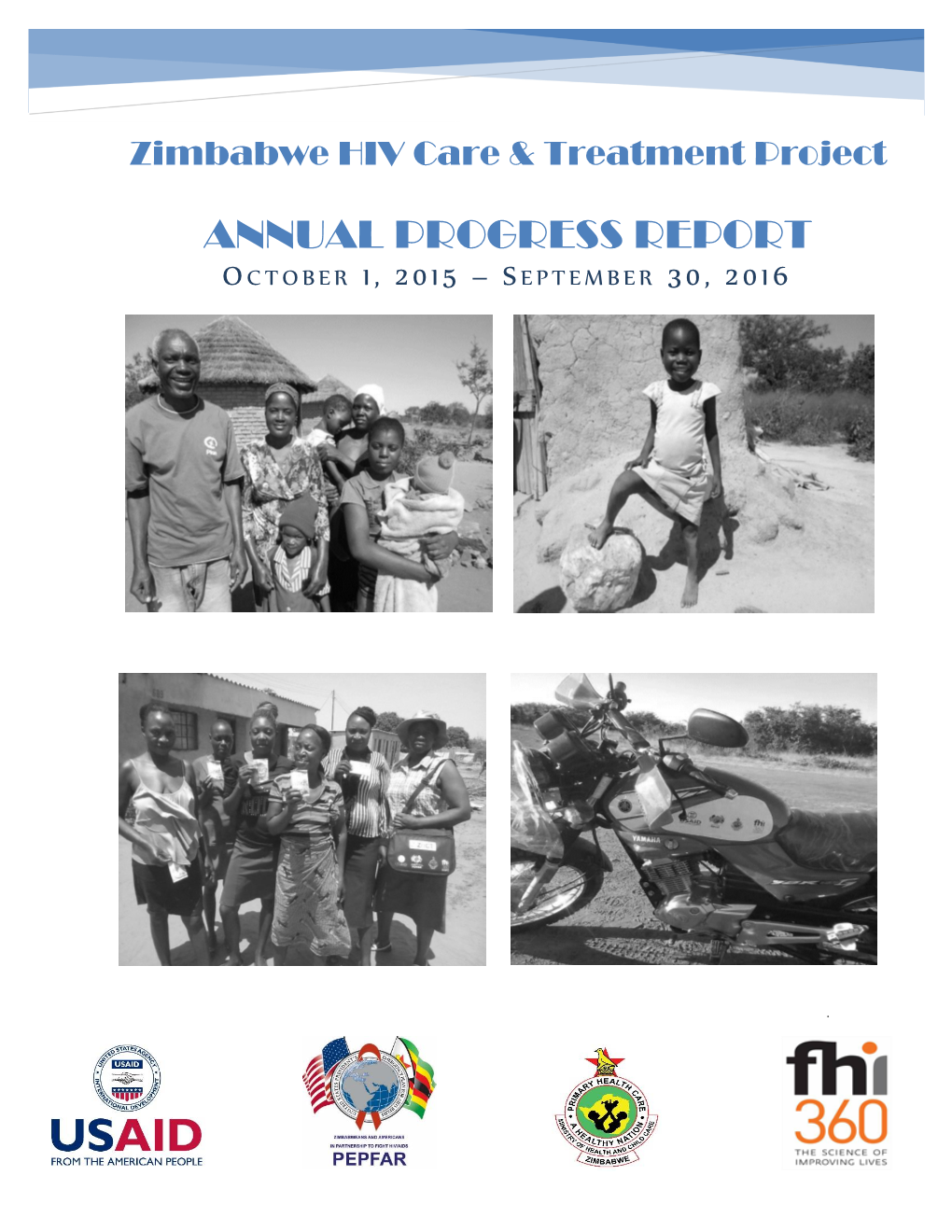
Zimbabwe HIV Care and Treatment Project Baseline Assessment Report
20 16 Zimbabwe HIV Care and Treatment Project Baseline Assessment Report '' CARG members in Chipinge meet for drug refill in the community. Photo Credits// FHI 360 Zimbabwe'' This study is made possible through the support of the American People through the United States Agency for International Development (USAID.) The contents are the sole responsibility of the Zimbabwe HIV care and Treatment (ZHCT) Project and do not necessarily reflect the views of USAID or the U.S. Government. FOREWORD The Government of Zimbabwe (GoZ) through the Ministry of Health and Child Care (MoHCC) is committed to strengthening the linkages between public health facilities and communities for HIV prevention, care and treatment services provision in Zimbabwe. The Ministry acknowledges the complementary efforts of non-governmental organisations in consolidating and scaling up community based initiatives towards achieving the UNAIDS ‘90-90-90’ targets aimed at ending AIDS by 2030. The contribution by Family Health International (FHI360) through the Zimbabwe HIV Care and Treatment (ZHCT) project aimed at increasing the availability and quality of care and treatment services for persons living with HIV (PLHIV), primarily through community based interventions is therefore, lauded and acknowledged by the Ministry. As part of the multi-sectoral response led by the Government of Zimbabwe (GOZ), we believe the input of the ZHCT project will strengthen community-based service delivery, an integral part of the response to HIV. The Ministry of Health and Child Care however, has noted the paucity of data on the cascade of HIV treatment and care services provided at community level and the ZHCT baseline and mapping assessment provides valuable baseline information which will be used to measure progress in this regard. -

MASHONALAND EAST PROVINCE - Overview Map 26 October 2009 Legend Province Capital
MASHONALAND EAST PROVINCE - Overview Map 26 October 2009 Legend Province Capital Hunyani Casembi Key Location Chikafa Chidodo Muzeza Musengezi Mine Mushumbi Musengezi Pools Chadereka Mission Mbire Mukumbura Place of Local Importance Hoya Kaitano Kamutsenzere Kamuchikukundu Bwazi Muzarabani Mavhuradonha Village Bakasa St. St. Gunganyama Pachanza Centenary Alberts Alberts Nembire Road Network Kazunga Chawarura Dotito Primary Chironga Rushinga Mount Rushinga Mukosa Guruve Karanda Rusambo Marymount Chimanda Secondary Marymount Shinje Darwin Rusambo Centenary Nyamatikiti Guruve Feeder azowe MashonalandMount M River Goromonzi Darwin Mudindo Dindi Kafura Bure Nyamanyora Railway Line Central Goora Kondo Madombwe Chistungo Mutepatepa Dendera Nyamapanda International Boundary Madziwa Borera Chiunye Kotwa Nyakudya Shinga Bradley Jester Mvurwi Madziwa Vanad Kasimbwi Institute Masarakufa Nzvimbo Madziwa Province Boundary Feock Mutawatawa Mudzi Muswewenhede Chakonda Suswe Mudzi Mutorashanga Charewa Chikwizo Howard District Boundary Nyota Shamva Nyamatawa Gozi Institute Bindura Chindengu Kawere Muriel Katiyo Rwenya Freda & Mont Dor Caesar Nyamuzuwe River Mazowe Rebecca Uzumba Nyamuzuwe Katsande Makaha River Shamva Mudzonga Makosa Trojan Shamva Nyamakope Fambe Glendale BINDURA MarambaKarimbika Sutton Amandas Uzumba All Nakiwa Kapondoro Concession Manhenga Kanyongo Souls Great Muonwe Mutoko PfungweMuswe Dyke Mushimbo Chimsasa Lake/Waterbody Madamombe Jumbo Bosha Nyadiri Avila Makumbe Mutoko Jumbo Mazowe Makumbe Parirewa Nyawa Rutope Conservation Area -

Manicaland-Province
School Level Province District School Name School Address Secondary Manicaland Buhera BANGURE ZVAVAHERA VILLAGE WARD 19 CHIEF NYASHANU BUHERA Secondary Manicaland Buhera BETERA HEADMAN BETERA CHIEF NYASHANU Secondary Manicaland Buhera BHEGEDHE BHEGEDHE VILLAGE CHIEF CHAMUTSA Secondary Manicaland Buhera BIKA KWARAMBA VILLAGE WARD 16 CHIEF NYASHANU Secondary Manicaland Buhera BUHERA GAVA VILLAGE WARD 5 CHIEF MAKUMBE BUHERA Secondary Manicaland Buhera CHABATA MUVANGIRWA VILLAGE WARD 29 Secondary Manicaland Buhera CHANGAMIRE MATSVAI VILLAGE WARD 32 NYASHANU Secondary Manicaland Buhera CHAPANDUKA CHAPANDUKA VILLAGE CHIEF NYASHANU Secondary Manicaland Buhera CHAPWANYA CHAPWANYA HIGH SCHOOL WARD 2 BUHERA Secondary Manicaland Buhera CHAWATAMA CHAWATAMA VILLAGE WARD 31 CHIEF MAKUMBE Secondary Manicaland Buhera CHIMBUDZI MATASVA VILLAGE WARD 32 CHIEF NYASHANU CHINHUWO VILLAGE CHIWENGA TOWNSHIP CHIEF Secondary Manicaland Buhera CHINHUWO NYASHANU Secondary Manicaland Buhera CHIROZVA CHIROZVA VILLAGE Secondary Manicaland Buhera CHIURWI CMAKUVISE VILLAGE WARD 32 Secondary Manicaland Buhera DEVULI NENDANDA VILLAGE CHIEF CHAMUTSA WARD 33 Secondary Manicaland Buhera GOSHO SOJINI VILLAGE WARD 5 CHIEF MAKUMBE Secondary Manicaland Buhera GOTORA GOTORA VILLAGE WARD 22 CHIEF NYASHANU BUHERA Secondary Manicaland Buhera GUNDE MABARA VILLAGE WARD 9 CHIEF CHITSUNGE BUHERA Secondary Manicaland Buhera GUNURA CHIEF CHAMUTSA NEMUPANDA VILLAGE WARD 30 BUHERA Secondary Manicaland Buhera GWEBU GWEBU SECONDARY GWEBU VILLAGE Secondary Manicaland Buhera HANDE KARIMBA VILLAGE -

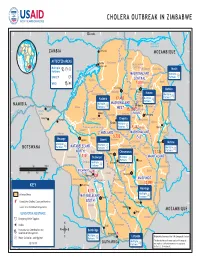
ZIMBABWE: Cholera Outbreak Snapshot
ZIMBABWE: Cholera outbreak snapshot (as of 10 October 2018) OVERVIEW KEY FIGURES By 10 October, 8,980 cholera cases (8,786 suspected and 194 confirmed cases), including 54 deaths (case fatality ratio 0.60 per cent), had been reported in seven provinces across 8,980 cholera cases 54 cholera deaths 18 areas with active Zimbabwe. Between 3 October and 10 October, 445 new cases were registered, including both new cases and older cases that were newly verified. New cases were recorded in four as of 10 October 2018 cholera outbreaks areas - Harare City, Chitungwiza (Harare), Buhera (Manicaland) and Bulawayo City (Bulawayo). Bulawayo City had not previously reported any infections. However, transmission is declining, with significantly fewer cases reported from 1 to 11 October (974) compared to Distribution of cholera cases by the same period in September (2,793). Harare City remains the epicentre of the outbreak, most affected suburbs, Harare City accounting for 97 per cent (8,721) of all cases and the majority of new cases. An estimated 22 per cent of all suspected and confirmed cases are children under age five. Glen View 46% The Oral Cholera Vaccine (OCV) mass vaccination campaign is underway and aims to protect 1.4 million people most at-risk of cholera in Harare, Chitungwiza and Epworth in two phases. HARARE CITY Budiriro 29% Phase one targeted 423,000 people in the most affected suburbs of Harare (Glen View, Other Suburbs 18% 8,721 Budiriro, Glen Norah and Mbare) and reached more than 378,100 people, 52.5 per cent of Kuwadzana Warren Park cases whom were females. -
Manicaland Province
USAID Zimbabwe USAID RESEARCH TECHNICAL ASSISTANCE CENTER February 2020 Zimbabwe Stakeholder Mapping Report: Manicaland Province Dominica Chingarande and Prosper Matondi This report is made possible by the generous support of the American people through the United States Agency for International Development (USAID) under the terms of contract no. 7200AA18C00057, which supports the Research Technical Assistance Center (RTAC). The contents of this report are the sole responsibility of RTAC and NORC at the University of Chicago and do not necessarily reflect the views of USAID or the United States Government. Month Year Acknowledgments The Research team expresses its gratitude to stakeholders participating in this study. Special appreciation to members of the District Food and Nutrition Committee and the District Drought Relief Committee, as well as to various nongovernmental organizations and private sector players who provided invaluable information about food security in Manicaland province. Research Technical Assistance Center The Research Technical Assistance Center is a network of academic researchers generating timely research for USAID to promote evidence-based policies and programs. The project is led by NORC at the University of Chicago in partnership with Arizona State University, Centro de Investigación de la Universidad del Pacífico (Lima, Peru), Davis Management Group, the DevLab@Duke University, Forum One, the Institute of International Education, the Pulte Institute for Global Development at the University of Notre Dame, Population Reference Bureau, the Resilient Africa Network at Makerere University (Kampala, Uganda), the United Negro College Fund, the University of Chicago, and the University of Illinois at Chicago. Suggested Citation Chingarande, D. and Matondi, P. 2020. Zimbabwe Stakeholder Mapping Report: Manicaland Province. -
Zimbabwe Program Map 2/19/09
CHOLERA OUTBREAK IN ZIMBABWE 24° 25° 26° 27° 28° Lusaka 29° 30° 31° 32° 33° 34° K afue ezi Z mb am a b Z è Albufeira de z Cahora Bassa e 16° ZAMBIA Chirundu MOZAMBIQUE 16° Guruve i n AFFECTED AREAS Kariba Hurungwe a y Muzarambani Kariba Dam n u (centenary) Multiple H Mt Darwin Rushinga Mudzi Partners B aJ Lake Kariba S MASHONALANDMASHONALAND Multiple a n Partners J UNICEF y a a Kariba t CENTRALCENTRAL Z i 17° a Shamva Mudzi 17° m WHO 7,200 b B D e Bindura U.M.P. z Chinhoyi i Mbare Mutoko Makonde Bindura Zvimba Harare Gokwe North Mutoko Multiple Kadoma 17,483 Multiple Partners J Harare Partners J Nyanga Multiple MASHONALANDMASHONALAND NAMIBIA Harare Victoria Falls Binga Partners J WESTWEST Murehwa e 15,1587Goromonzi b G ho Victoria M 18° C w u 18° i Gokwe n HARAREHARARE nt Falls a y Chegutu Marondera y Kadoma a at y i i in Matetsi Seke L Hwange Gokwe South Chegutu Marondera Sengwa Makoni Kadoma Multiple Partners J 5,412 Wedza Nyanga Lupane i Sh z angani MIDLANDSMIDLANDS MASHONALANDMASHONALAND d Mutasa Hwange S O a 5,732 v Nkayi EASTEAST e Hwange Lupane Gweru Kwekwe 19° Chikomba Mutare Mutare 19° Multiple Multiple Chirumanzu BOTSWANA Partners J MATABELELANDMATABELELAND Partners J Buhera Mutare MultipleLago Gweru PartnersChicamba J NORTHNORTH Bubi Chirumanzu 11,124 Gweru Gutu Tsholotsho 1,110 Bulawayo Multiple MANICALANDMANICALAND G w Partners J M Gutu a Umguza u y Multiple Shurugwi i t i Partners Shurugwi r 0 50 100 mi J i k Chimanimani a w Nat BULAWAYOBULAWAYO i Bikita 7 R 20° 0 50 100 150 km u 20° Insiza n d Masvingo Bulawayo 439 e zi MASVINGOMASVINGO Bu Bulalimamangwe Umzingwane Zvishavane Rio Chivi Zaka e Chipinge 10,053 v Plumtree a KEY S Masvingo Masvingo 5,171 Mberengwa Affected Areas Multiple MATABELELANDMATABELELAND Gwanda Partners J Cumulative Cholera Cases per Province SOUTHSOUTH Triangle 21°# 21° S Matobo Source: U.N. -

Manicaland Province
School Province District School Name School Address Level Primary Manicaland Buhera BANGURE MUKONYA VILLAGE,CHIKUWA AREA BUHERA Primary Manicaland Buhera BARURA BARURA PRIMARY SCHOOL WARD 28 BUHERA Primary Manicaland Buhera BASIRA BASIRA VILLAGE WARD 21 MURWIRA Primary Manicaland Buhera BERE CHIEF CHITAURO MABURUTSE VILLAGE Primary Manicaland Buhera BETERA BETERA VILLAGE WARD 20 CHIEF NYASHANU Primary Manicaland Buhera BHEGEDHE BHEGEDHE VILLGE WARD 29 CHIEF CHAMUTSA KWARAMBA VILLAGE WARD 16 CHIEF Primary Manicaland Buhera BIKA NYASHANU Primary Manicaland Buhera BIRCHENOUGH BRIDGE MUSHATI VILLAGE Primary Manicaland Buhera BUHERA VILLAGE TSODZO VILLAGE WARD 5 CHIEF MAKUMBE Primary Manicaland Buhera CHABATA WARD 29 BUHERA DISTRICT Primary Manicaland Buhera CHAKO NEMADARE VILLAGE WARD 30 BUHERA Primary Manicaland Buhera CHANGAMIRE MATSVAI VILLAGE WARD 32 CHIEF NYASHANU CHAPANDUKA PRIMARY SCHOOL NYASHANU Primary Manicaland Buhera CHAPANDUKA BUHERA Primary Manicaland Buhera CHAPUNGU MANYONDA VILLAGE WARD 2 BUHERA WEST Primary Manicaland Buhera CHATINDO BUHERA CHIEF MAKUMBE WARD 3 Primary Manicaland Buhera CHAWATAMA CHAWATAMBA VILLAGE CHIEF MAKUMBE Primary Manicaland Buhera CHIHERA CHIHERA VILLAGE HEADMAN BETERA WARD 20 Primary Manicaland Buhera CHIKUVIRE CHIKUVIRE VILLAGE WARD 4 NERUTANGA MUDZINGWA VILLAGE CHIEF MAKUMBE Primary Manicaland Buhera CHIKWEKWETE BUHERA Primary Manicaland Buhera CHIMBUDZI MATASVA VILLAGE WARD 32 NYASHANU Primary Manicaland Buhera CHIMOMBE CHIMOMBE VILLAGE CHIEF NYASHANU Primary Manicaland Buhera CHINHORO ST EDWARDS -

Zimbabwe Total Financialzimbabwe Requirements Flash Appeal (Us$) Total People in Need Total People Targeted
FLASH 2019 APPEAL (Revised following Cyclone Idai, March 2019) January - June 2019 Photo: GOAL\Anteneh Tadele ZIMBABWE TOTAL FINANCIALZIMBABWE REQUIREMENTS FLASH APPEAL (US$) TOTAL PEOPLE IN NEED TOTAL PEOPLE TARGETED $294M 5.57M 2.47M FINANCIAL REQUIREMENTS - FLOODS PEOPLE IN NEED - FLOODS PEOPLE TARGETED - FLOODS $60M 270K 270K FINANCIAL REQUIREMENTS - DROUGHT PEOPLE IN NEED - DROUGHT PEOPLE TARGETED - DROUGHT $234M 5.3M 2.2M MASHONALAND MASHONALAND CENTRAL WEST 0.3m Kariba! 0.4m MASHONALAND 0.3m HARARE EAST 260K 0.3m MIDLANDS MANICALAND MATABELELAND NORTH 02 0.4m 0.6m 10K BULAWAYO MASVINGO MATABELELAND SOUTH 0.4m 0.2m XX F insecur IPC Food Insecurity Phase 1 Mal XX P b 2 Sessed b ovince 3 A districts 4 Egency M 5 CatastrFamine A least e ! assistance Le Source: Zimbabwe IPC TWG This document is produced by the Humanitarian Country Team and the United Nations Resident Coordinator’s Office in Zimbabwe with the support of the United Nations Office for the Coordination of Humanitarian Affairs (OCHA). The projects reflected here support the national government. It covers the period from January to June 2019. The Plan has been revised in March 2019 to incorporate the immediate response to needs arising from the impact of Cyclone Idai. JANUARY - JUNE 2019 TABLE OF CONTENTS FOREWORD BY THE UN RESIDENT COORDINATOR 04 THE FLASH APPEAL AT A GLANCE 05 OVERVIEW OF THE CRISIS 06 RESPONSE STRATEGY AND STRATEGIC OBJECTIVES 11 RESPONSE STRATEGY AND CAPACITY 12 SUMMARY OF NEEDS, TARGETS & REQUIREMENTS 13 SECTOR RESPONSE PLANS AGRICULTURE